Abstract
Background
Diagnosis and treatment of pseudotumor cerebri syndrome in children is still a challenge for clinicians. The aim of this study is to reveal the influence of presentation age and CSF opening pressure on long-term prognosis of pseudotumor cerebri and share our clinical data of the very young age (≤ 5-year) group.
Method
This retrospective study includes the patients followed by the Marmara University Pediatric Neurology Clinic between years 2012 and 2020 diagnosed with definite, probable, or suggestive pseudotumor cerebri syndrome according to modified Friedman criteria. Patients were classified into three groups according to presentation age: group 1: ≤ 5 years old; group 2: 6–10 years; and group 3 > 10 years old. CSF opening pressure was also categorized into three groups as CSF < 20 cmH20; CSF 20–30 cmH20; and CSF > 30 cmH20.
Results
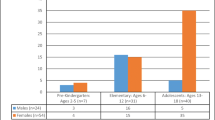
One hundred three patients, 62.1% female (n = 64), were enrolled in the study. Group 1 consisted of 16 patients (60% male), group 2 consisted of 30 patients (63.3% female), and group 3 consisted of 57 patients (66.7% female). The mean CSF opening pressure did not differ between the three age groups in our study (p > 0.05). Treatment response was not correlated with CSF opening pressure. Papilledema presence and level of CSF opening pressure were independent of age (p > 0.05).
Conclusions
Age at presentation and CSF opening pressure at diagnosis are not any predictive factors that influence long-term prognosis of pseudotumor cerebri syndrome in children. Evaluation and follow-up of children should be done in personalized approach.
Similar content being viewed by others
Availability of data and materials
All raw data included in this study will be freely available from the corresponding author on reasonable request without breaching patient confidentiality.
References
Balbi GGM, Matas SL, Len CA, Frage MM, Sousa IO, Terreri MT (2018) Pseudotumor cerebri in childhood and adolescence: data from a specialized service. Arq Neuropsiquiatr 76(11):751–755. https://doi.org/10.1590/0004-282X20180131
Per H, Canpolat M, Gümüş H, Poyrazoğlu HG, Yıkılmaz A, Karaküçük S et al (2013) Clinical spectrum of the pseudotumor cerebri in children: etiological, clinical features, treatment and prognosis. Brain Dev 35(6):561–568. https://doi.org/10.1016/j.braindev.2012.08.008
Wall M, Kupersmith M, Kieburtz K, Corbett J, Feldon S, Friedman D et al (2014) Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA 311(16):1641–1651. https://doi.org/10.1001/jama.2014.3312
Gersti L, Schoppe N, Albers L, Erti-Wagner B, Alperin N, Ehrt O et al (2017) Pediatric idiopathic intracranial hypertension - is the fixed threshold value of elevated LP opening pressure set too high? - Eur J Paediatr Neurol 21(6):833–841. https://doi.org/10.1016/j.ejpn.2017.08.002
Spitze A, Lam P, Al-Zubidi N, Yalamanchili S, Lee AG (2014) Controversies: optic nerve sheath fenestration versus shunt placement for the treatment of idiopathic intracranial hypertension. Indian J Ophtalmol 62(10):1015–1021. https://doi.org/10.4103/0301-4738.146012
Friedman DI, Liu GT, Digre KB (2013) Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 81:1–7. https://doi.org/10.1212/WNL.0b013e3182a55f17
Sheldon CA, Paley GL, Beres SJ, McCormack SE, Liu GT (2017) Pediatric pseudotumor cerebri syndrome: diagnosis, classification, and underlying pathophysiology. Semin Pediatr Neurol 24(2):110–115. https://doi.org/10.1016/j.spen.2017.04.002
Burkett JG, Ailani J (2018) An up to date review of pseudotumor cerebri syndrome. Curr Neurol Neurosci Rep 18(6):33. https://doi.org/10.1007/s11910-018-0839-1
Rangwala LM, Lui GT (2007) Pediatric idiopathic intracranial hypertension. Surv Ophtalmol 52(6). https://doi.org/10.1016/j.survophthal.2007.08.018. https://doi.org/10.1007/s00701-016-3050-7
Portelli M, Papageorgiou PN (2017) An update on idiopathic intracranial hypertension. Acta Neurochir (Wien) 159(3):491–499. https://doi.org/10.1007/s00701-016-3050-7
Barmberzig R, Szperka CL (2019) Pseudotumor cerebri syndrome in children. Curr Pain Headache Rep 23(8):58. https://doi.org/10.1007/s11916-019-0795-8
Hilely A, Hecht I, Cohen NG, Leiba H (2019) Long term follow-up of pseudotumor cerebri syndrome in pre-pubertal children, adolescents and adults. Pediatr Neurol 101(57):63. https://doi.org/10.1016/j.pediatrneurol.2019.04.018
Aylward SC (2013) Pediatric idiopathic intracranial hypertension: a need for clarification. Pediatr Neurol 49. https://doi.org/10.1016/j.pediatrneurol.2013.05.019
Dandy WE (1937) Intracranial pressure without brain tumor. Ann Surg 106:492–513. https://doi.org/10.1097/00000658-193710000-00002
Kohli AA, Vossough A, Mallery RM, Woo JH, Sheldon CA, Paley GL, Digre KB, Friedman DI, Farrar JT, Mc Cormack SE, Liu GT, Szperka CL (2019) Magnetic resonance imaging findings in pediatric pseudotumor cerebri syndrome. Pediatr Neurol 99:31–39. https://doi.org/10.1016/j.pediatrneurol.2019.04.010
Mollan SP, Markey KA, Benzimra JD, Jacks A, Matthews TD, Burdon MA, Sinclair AJ (2014) A practical approach to diagnosis, assesment and management of idiopathic intracranial hypertension. Pract Neurol 14:380–390. https://doi.org/10.1136/practneurol-2014-000821
Lenfeldt N, Koskinen LOD, Berenheim AT, Malm J, Eklund A (2007) CSF pressure assesed by lumbar puncture agrees with intracranial pressure. Neurology 68(2):155–158. https://doi.org/10.1212/01.wnl.0000250270.54587.71
Mahajnah M, Genizi J, Zahalka H, Andreus R, Zelnik N (2020) Pseudotumor cerebri syndrome: from childhood to adulthood risk factors and clinical presentation. J Child Neurol 35(5):311–316. https://doi.org/10.1177/0883073819895179
Bar-Joseph G, Guilburd Y, Tamir A, Guilburd JN (2009) Effectiveness of ketamine in decreasing intracranial pressure in children with intracranial hypertension. J Neurosurg Pediatr 4:40–46. https://doi.org/10.3171/2009.1.PEDS08319
Inger H, Rogers DL, McGregor ML, Aylward AC, Reem RE (2017) Diagnostic criteria in pediatric intracranial hypertension. J AAPOS 21(6):492-495.e2. https://doi.org/10.1016/j.jaapos.2017.08.003
Philips PH, Sheldon CA (2017) Pediatric pseudotumor cerebri syndrome. J Neuro-Ophtalmol 37(Suppl):S33–S40. https://doi.org/10.1097/WNO.0000000000000548
Bole S, Martinez-Rios C, Tibussek D, Pohl D (2019) Infantile idiopathic intracranial hypertension: a case study and review of the literature. J Child Neurol 34(13):806–814. https://doi.org/10.1177/0883073819860393
Kattah JC, Pula JH, Mejico LJ, McDermott MP, Kupersmith MJ, Wall M (2015) CSF Pressure, pilledema grade and response to acetozolamide in the idiopathic Intracranial Hypertension Treatment Trial. J Neurol 262(10):2271–2274. https://doi.org/10.1007/s00415-015-7838-9
Lim M, Kurian M, Penn A, Calver D, Lin JP (2005) Visual failure without headache in idiopathic intracranial hypertension. Arch Dis Child 90:206–210. https://doi.org/10.1136/adc.2003.039305
Gondi KT, Chen KS, Gratton SM (2019) Asymptomatic versus symptomatic idiopathic intracranial hypertension in children. J Child Neurol 34(12):751–756. https://doi.org/10.1177/0883073819858455
Reid JE, Reem RE, Aylward SC, Rogers DL (2016) Sixth nerve palsy in pediatric intracranial hypertension. Neuroophtalmology 40(1):23–27. https://doi.org/10.3109/01658107.2015.1117498
Mallery RM, Friedman DI, Liu GT (2014) Headache and the pseudotumor cerebri syndrome. Curr Pain Headache Rep 18:446. https://doi.org/10.1007/s11916-014-0446-z
Lin A, Foroozan R, Danesh-Meyer HV, De Salvo G, Savino PJ, Sergott RC (2006) Occurrence of cerebral venous sinus thrombosis in patients with presumed idiopathic intracranial hypertension. Ophtalmology 113(12):2281–2284. https://doi.org/10.1016/j.ophtha.2006.05.065
Fonseca PL, Rigamonti D, Miller NR, Subramanian PS (2014) Visual outcomes of surgical intervention for pseudotumor cerebri:optic nerve sheath fenestration versus cerebrospinal fluid diversion. Br J Ophtalmol 98:1360. https://doi.org/10.1136/bjophthalmol-2014-304953
Bruce BB, Digre KB, McDermott MP, Schron EB, Wall M (2016) NORDIC Idiopathic Intracranial Hypertension Study Group. Quality of life at 6 months in the idiopathic intracranial hypertension treatment trial. Neurology 87:18717. https://doi.org/10.1212/WNL.0000000000003280
Soiberman U, Stolovitch C, Balcer LJ, Regenbogen M, Constantini S, Kesler A (2011) Idiopathic intracranial hypertension in children:visual outcome and risk recurrence. Childs Nerv Syst 27(11):1913–8. https://doi.org/10.1007/s00381-011-1470-5
Masri A, Jaafar A, Noman R, Gharaibeh A, Ababneh OH (2015) Intracranial hypertension in children: etiologies, clinical features and outcome. J Child Neurol 30(12):1562–8. https://doi.org/10.1177/0883073815574332
Author information
Authors and Affiliations
Contributions
GO designed the study, collected and analyzed data and wrote the manuscript. OU and DT read and critically revised the manuscript. VD performed the ophtalmologic examination of the patients, BA performed the radiological evaluation of cranial MRIs, and AD performed the surgical procedures to the patients when necessary.
Corresponding author
Ethics declarations
Ethical approval
Ethics committee approval was obtained from the local ethics committee of the university with approval number 674 (12.06.2020). Informed consent was obtained from the parents of patients involved in the study. The authors also affirm that the participants gave consent for their data in a journal article.
Conflict of interest
The authors declare no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript presents a comprehensive study about Pediatric Pseudotumor Cerebri Syndrome based on demonstrative characteristics according to age and CSF opening pressure. Long follow-up experience of a tertiary pediatric neurology clinic is given with specific emphasis on pitfalls on diagnosis, and correlation of our findings is done compared to the literature.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ozturk, G., Turkdogan, D., Unver, O. et al. How do presentation age and CSF opening pressure level affect long-term prognosis of pseudotumor cerebri syndrome in children? Experience of a single tertiary clinic. Childs Nerv Syst 38, 95–102 (2022). https://doi.org/10.1007/s00381-021-05365-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05365-8