Abstract
Introduction
Infant hydrocephalus represents an important public health issue. Recent analysis of registry-based data has improved our understanding of the variable epidemiology of infant hydrocephalus around the world and the consequent burden of disease that this vulnerable population must carry throughout their lifetimes. The purpose of this article is to review the epidemiology of infant hydrocephalus, highlighting the ways in which analysis of prospectively collected registry data has contributed to our current knowledge and how similar methods may lead to new discovery.
Discussion
Congenital abnormalities and spina bifida-associated hydrocephalus, along with acquired postnatal hydrocephalus secondary to intraventricular hemorrhage of prematurity and infection, represent the most common etiologies of infant hydrocephalus, with their relative prevalence dependent on geographic region and socioeconomic status. Best current estimates suggest that the incidence of congenital and acquired infant hydrocephalus may be between 80 and 125 cases/100,000 births depending on world region. These incidence figures and their forecasts, together with improved survival associated with promptly diagnosed and treated hydrocephalus, suggest that the burden of hydrocephalus, as measured by prevalence, is primed to increase.
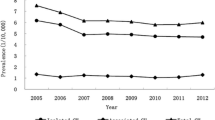
Counterbalancing these statistics is evidence that perhaps, in some regions, improvements in neurosurgical and general perinatal care, as well as shifting indications for initial surgical intervention in these infants (and therefore in the very definition of hydrocephalus itself), the number of infants who require first time surgical treatment for hydrocephalus, may be decreasing. Further longitudinal data collection will undoubtedly assist in determining whether these trends are robust.
Conclusion
When one takes a global perspective, complexities related to the underlying epidemiology of infant hydrocephalus become abundantly clear. The causes of infant hydrocephalus vary from one world region to another, largely related to the underlying income characteristics of the population. Likewise, increased birth rates in low-income areas of the world are likely to result in an increased incidence and prevalence of infant hydrocephalus in those regions, whereas sophisticated and resource-intensive advancements in perinatal care available in other regions may result in decreased epidemiological estimates of disease burden in others. Further analysis of high-quality registry-based data may help clarify these issues.
Similar content being viewed by others
References
Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Dabrowiak ME, Sutton LN, Gupta N, Tulipan NB, D'Alton ME, Farmer DL, Investigators M (2011) A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364:993–1004. https://doi.org/10.1056/NEJMoa1014379
Ahrens K, Yazdy MM, Mitchell AA, Werler MM (2011) Folic acid intake and spina bifida in the era of dietary folic acid fortification. Epidemiology 22:731–737. https://doi.org/10.1097/EDE.0b013e3182227887
Ballabh P, de Vries LS (2021) White matter injury in infants with intraventricular haemorrhage: mechanisms and therapies. Nat Rev Neurol. https://doi.org/10.1038/s41582-020-00447-8
Boulet SL, Yang Q, Mai C, Kirby RS, Collins JS, Robbins JM, Meyer R, Canfield MA, Mulinare J, National Birth Defects Prevention N (2008) Trends in the postfortification prevalence of spina bifida and anencephaly in the United States. Birth Defects Res A Clin Mol Teratol 82:527–532. https://doi.org/10.1002/bdra.20468
Dewan MC, Rattani A, Mekary R, Glancz LJ, Yunusa I, Baticulon RE, Fieggen G, Wellons JC, Park KB, Warf BC (2018) Global hydrocephalus epidemiology and incidence: systematic review and meta-analysis. J Neurosurg 130:1–15. https://doi.org/10.3171/2017.10.JNS17439
Diehl D, Belke F, Kohl T, Axt-Fliedner R, Degenhardt J, Khaleeva A, Oehmke F, Faas D, Ehrhardt H, Kolodziej M, Uhl E, Windhorst AC, Neubauer BA (2021) Fully percutaneous fetoscopic repair of myelomeningocele: 30-month follow-up data. Ultrasound Obstet Gynecol 57:113–118. https://doi.org/10.1002/uog.22116
Fernandez-Mendez R, Richards HK, Seeley HM, Pickard JD, Joannides AJ, collaborators U (2019) Current epidemiology of cerebrospinal fluid shunt surgery in the UK and Ireland (2004-2013). J Neurol Neurosurg Psychiatry 90:747–754. https://doi.org/10.1136/jnnp-2018-319927
Isaacs AM, Riva-Cambrin J, Yavin D, Hockley A, Pringsheim TM, Jette N, Lethebe BC, Lowerison M, Dronyk J, Hamilton MG (2018) Age-specific global epidemiology of hydrocephalus: systematic review, metanalysis and global birth surveillance. PLoS One 13:e0204926. https://doi.org/10.1371/journal.pone.0204926
Koschnitzky JE, Keep RF, Limbrick DD Jr, McAllister JP 2nd, Morris JA, Strahle J, Yung YC (2018) Opportunities in posthemorrhagic hydrocephalus research: outcomes of the Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. Fluids Barriers CNS 15:11. https://doi.org/10.1186/s12987-018-0096-3
Leijser LM, Miller SP, van Wezel-Meijler G, Brouwer AJ, Traubici J, van Haastert IC, Whyte HE, Groenendaal F, Kulkarni AV, Han KS, Woerdeman PA, Church PT, Kelly EN, van Straaten HLM, Ly LG, de Vries LS (2018) Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology 90:e698–e706. https://doi.org/10.1212/WNL.0000000000004984
Mazzola CA, Choudhri AF, Auguste KI, Limbrick DD Jr, Rogido M, Mitchell L, Flannery AM, Pediatric Hydrocephalus Systematic R, Evidence-Based Guidelines Task F (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: Management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr 14(Suppl 1):8–23. https://doi.org/10.3171/2014.7.PEDS14322
McCarthy DJ, Sheinberg DL, Luther E, McCrea HJ (2019) Myelomeningocele-associated hydrocephalus: nationwide analysis and systematic review. Neurosurg Focus 47:E5. https://doi.org/10.3171/2019.7.FOCUS19469
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sanchez PJ, O'Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID 3rd, Watterberg KL, Saha S, Das A, Higgins RD, Eunice Kennedy Shriver National Institute of Child H, Human Development Neonatal Research N (2010) Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126:443–456. https://doi.org/10.1542/peds.2009-2959
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, Laptook AR, Sanchez PJ, Van Meurs KP, Wyckoff M, Das A, Hale EC, Ball MB, Newman NS, Schibler K, Poindexter BB, Kennedy KA, Cotten CM, Watterberg KL, D'Angio CT, DeMauro SB, Truog WE, Devaskar U, Higgins RD, Eunice Kennedy Shriver National Institute of Child H, Human Development Neonatal Research N (2015) Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314:1039–1051. https://doi.org/10.1001/jama.2015.10244
Tamber MS, Flannery AM, McClung-Smith C, Assassi N, Bauer DF, Beier AD, Blount JP, Durham SR, Klimo P Jr, Nikas DC, Rehring P, Tyagi R, Mazzola CA (2019) Congress of neurological surgeons systematic review and evidence-based guideline on the incidence of shunt-dependent hydrocephalus in infants with myelomeningocele after prenatal versus postnatal repair. Neurosurgery 85:E405–E408. https://doi.org/10.1093/neuros/nyz262
Tamber MS, Kestle JRW, Reeder RW, Holubkov R, Alvey J, Browd SR, Drake JM, Kulkarni AV, Limbrick DD, McDonald PJ, Rozzelle CJ, Simon TD, Naftel R, Shannon CN, Wellons JC, Whitehead WE, Riva-Cambrin J, Hydrocephalus Clinical Research N (2020) Temporal trends in surgical procedures for pediatric hydrocephalus: an analysis of the Hydrocephalus Clinical Research Network Core Data Project. J Neurosurg Pediatr 27:1–8. https://doi.org/10.3171/2020.7.PEDS20142
Thomale UW, Cinalli G, Kulkarni AV, Al-Hakim S, Roth J, Schaumann A, Buhrer C, Cavalheiro S, Sgouros S, Constantini S, Bock HC (2019) TROPHY registry study design: a prospective, international multicenter study for the surgical treatment of posthemorrhagic hydrocephalus in neonates. Childs Nerv Syst 35:613–619. https://doi.org/10.1007/s00381-019-04077-4
Tirado-Caballero J, Rivero-Garvia M, Arteaga-Romero F, Herreria-Franco J, Lozano-Gonzalez A, Marquez-Rivas J (2020) Neuroendoscopic lavage for the management of posthemorrhagic hydrocephalus in preterm infants: safety, effectivity, and lessons learned. J Neurosurg Pediatr 26:1–10. https://doi.org/10.3171/2020.2.PEDS2037
Tulipan N, Wellons JC 3rd, Thom EA, Gupta N, Sutton LN, Burrows PK, Farmer D, Walsh W, Johnson MP, Rand L, Tolivaisa S, D'Alton ME, Adzick NS, Investigators M (2015) Prenatal surgery for myelomeningocele and the need for cerebrospinal fluid shunt placement. J Neurosurg Pediatr 16:613–620. https://doi.org/10.3171/2015.7.PEDS15336
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tamber, M.S. Insights into the epidemiology of infant hydrocephalus. Childs Nerv Syst 37, 3305–3311 (2021). https://doi.org/10.1007/s00381-021-05157-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05157-0