Abstract
Purpose
To analyze the long-term efficacy of the ventriculoatrial shunt (VAS) in pediatric patients with hydrocephalus, focusing on the atrial catheter and suitable revision procedures of the distal catheter following VAS malformation performed at our institution.
Methods
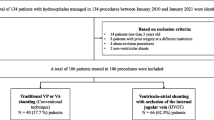
The authors retrospectively analyzed data of 28 pediatric patients under the age of 10 years who were treated with VAS for hydrocephalus and who had a follow-up period of at least 5 years.
Results
A total of 42 atrial tube revision procedures were performed in 28 patients during the study period. The median atrial tube survival time due to atrial tube obstruction was 2.32 years (n = 31, range: 0.4–8.08 years). Atrial tube survival time was shorter in younger children (p < 0.0001) and in children who were shorter in height (p = 0.0001). As a revision procedure following atrial tube malfunction, 22 (78.6%) out of the 28 patients who had an inserted VAS had the VAS reconversion into a VPS at the last follow-up.
Conclusions
VAS can be a useful alternative to VPS, but it requires frequent atrial tube revisions, especially in younger children. Reconversion to VPS after VAS malfunction is a reasonable option and is associated with longer shunt survival time despite its previously observed difficulties.


Similar content being viewed by others
Abbreviations
- VAS:
-
Ventriculoatrial shunt
- VPS:
-
Ventriculoperitoneal shunt
References
Rymarczuk GN, Keating RF, Coughlin DJ et al (2019) A comparison of ventriculoperitoneal and ventriculoatrial shunts in a population of 544 consecutive pediatric patients. Neurosurgery 87(1):80–85
Vernet O, Campiche R, de Tribolet N (1995) Long-term results after ventriculo-atrial shunting in children. Childs Nerv Syst 11(3):176–179
Borgbjerg BM, Gjerris F, Albeck MJ, Hauerberg J, Børgesen SV (1998) A comparison between ventriculo-peritoneal and ventriculo-atrial cerebrospinal fluid shunts in relation to rate of revision and durability. Acta Neurochir 140(5):459–464 discussion 465
Martin JE, Keating RF, Cogen PH, Midgley FM (2003) Long-term follow-up of direct heart shunts in the management of hydrocephalus. Pediatr Neurosurg 38(2):94–97
Keucher TR, Mealey J Jr (1979) Long-term results after ventriculoatrial and ventriculoperitoneal shunting for infantile hydrocephalus. J Neurosurg 50(2):179–186
Kariyattil R, Steinbok P, Singhal A, Cochrane DD (2007) Ascites and abdominal pseudocysts following ventriculoperitoneal shunt surgery: variations of the same theme. J Neurosurg 106(5 Suppl):350–353
Mobley LW 3rd, Doran SE, Hellbusch LC (2005) Abdominal pseudocyst: predisposing factors and treatment algorithm. Pediatr Neurosurg 41(2):77–83
Erwood A, Rindler RS, Motiwala M et al (2019) Management of sterile abdominal pseudocysts related to ventriculoperitoneal shunts. J Neurosurg Pediatr 2019:1–5
Habibi Z, Golpayegani M, Ashjaei B et al (2020) Suprahepatic space as an alternative site for distal catheter insertion in pseudocyst-associated ventriculoperitoneal shunt malfunction. J Neurosurg Pediatr 2020:1–8
Symss NP, Oi S (2015) Is there an ideal shunt? A panoramic view of 110 years in CSF diversions and shunt systems used for the treatment of hydrocephalus: from historical events to current trends. Childs Nerv Syst 31(2):191–202
Steele J, Stewart R, Komarlu R, Najm H (2018) Large superior vena cava thrombus requiring thrombectomy as a complication of ventriculo-atrial shunt. J Card Surg 33(7):397–398
Tonn P, Gilsbach JM, Kreitschmann-Andermahr I, Franke A, Blindt R (2005) A rare but life-threatening complication of ventriculo-atrial shunt. Acta Neurochir 147(12):1303–1304
Grover SK, Puri R, Wong TL, Dundon BK, Tayeb H, Steele PM (2010) Ventriculo-atrial shunt induced severe pulmonary arterial hypertension: a time for routine screening? Intern Med J 40(5):386–387
Amelot A, Bouazza S, George B, Bresson D (2014) Causative role of infection in chronic non-thromboembolic pulmonary hypertension following ventriculo-atrial shunt. Br J Neurosurg 28(4):559–561
Clark DJ, Chakraborty A, Roebuck DJ, Thompson DN (2016) Ultrasound guided placement of the distal catheter in paediatric ventriculoatrial shunts-an appraisal of efficacy and complications. Childs Nerv Syst 32(7):1219–1225
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamashita, S., Kimiwada, T., Hayashi, T. et al. Reconversion to ventriculoperitoneal shunt following ventriculoatrial shunt malfunction in children. Childs Nerv Syst 37, 2207–2213 (2021). https://doi.org/10.1007/s00381-021-05045-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05045-7