Abstract
Purpose
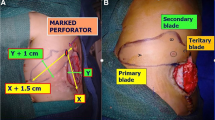
Of the many suggested techniques, we used dorsal intercostal perforator artery flap (DIPAF) for the closure of myelomeningocele defects. This study compared the outcomes of primary closure and DIPAF in the closure of myelomeningoceles.
Methods
Data of 24 patients that underwent myelomeningocele surgery at a single institution between November 2015 and September 2019 were retrospectively reviewed.
Results
The primary closure group had 13 patients (54.17%) and the DIPAF group had 11 (45.83%). The mean age was 7.91 ± 13.27 days (1–60 days). Twelve patients were female and 12 were male. In 22 patients, the myelomeningocele sacs were in the lumbosacral region, while in 2, they were in the thoracolumbar region. The mean defect sizes were 14.20 ± 4.62 cm2 and 18.44 ± 3.49 cm2 in the primary closure and DIPAF groups, respectively. In each group, four patients had a kyphotic deformity. In the primary closure group, three patients had wound necrosis, two had wound dehiscence, and four had cerebrospinal fluid (CSF) leakage. In the DIPAF group, one patient had wound necrosis and one had CSF leakage. Significantly fewer complications related to the operation area were observed in the DIPAF group (p < 0.05). Increased defect size, kyphotic deformity, and presence of hydrocephalus were found to be risk factors for complications related to the operation area.
Conclusion
This surgical treatment protects neural tissue, prevent CSF leakage, and reduce central nervous system infection rates in myelomeningocele patients. Closure technique with the fasciocutaneous skin flap has more satisfying results than primary closure.

Similar content being viewed by others
References
Wallingford JB (2005) Neural tube closure and neural tube defects: studies in animal models reveal known knowns and known unknowns. Am J Med Genet C Semin Med Genet 135C(1):59–68
Lobo GJ, Nayak M (2018) V-Y plasty or primary repair closure of myelomeningocele: our experience. J Pediatr Neurosci 13(4):398–403
Shaer CM, Chescheir N, Schulkin J (2007) Myelomeningocele: a review of the epidemiology, genetics, risk factors for conception, prenatal diagnosis, and prognosis for affected individuals. Obstet Gynecol Surv 62(7):471–479
Lien SC, Maher CO, Garton HJL, Kasten SJ, Muraszko KM, Buchman SR (2010) Local and regional flap closure in myelomeningocele repair: a 15-year review. Childs Nerv Syst 26(8):1091–1095
El-khatib HA (2004) Large thoracolumbar meningomyelocele defects: incidence and clinical experiences with different modalities of latissimus dorsi musculocutaneus flap. Br J Plast Surg 57(5):411–417
Peranteau WH, Adzick NS (2016) Prenatal surgery for myelomeningocele. Curr Opin Obstet Gynecol 28(2):111–118
Atik B, Tan O, Kiymaz N, Yilmaz N, Tekes L (2006) Bilobed fasciocutaneous flap closure of large meningomyeloceles. Ann Plast Surg 56(5):562–564
Isik D, Tekes L, Eseoglu M, Isik Y, Bilici S, Atik B (2011) Closure of large myelomeningocele defects using dorsal intercostal artery perforator flap. Ann Plast Surg 67(2):159–163
Ramirez OM, Ramasastry SS, Granick MS, Pang D, Futrell JW (1987) A new surgical approach to closure of large lumbosacral meningomyelocele defects. Plast Reconstr Surg 80(6):799–809
Lapid O, Rosenberg L, Cohen A (2001) Meningomyelocele reconstruction with bilobed flaps. Br J Plast Surg 54(7):570–572
Ozcelik D, Yildiz KH, Is M, Dosoglu M (2005) Soft tissue closure and plastic surgical aspects of large dorsal myelomeningocele defects (review of techniques). Neurosurg Rev 28(3):218–225
Sarifakioglu N, Bingul F, Terzioglu A, Ates L, Aslan G (2003) Bilateral split latissimus dorsi V-Y flaps for closure of large thoracolumbar meningomyelocele defects. Br J Plast Surg 56(3):303–306
Cruz NI, Ariyan S, Duncan CC, Cuono CB (1983) Repair of lumbosacral myelomeningoceles with double Z-rhomboid flaps. Technical note. J Neurosurg 59(4):714–717
Duffy FJ Jr, Weprin BE, Swift DM (2004) A new approach to closure of large lumbosacral myelomeningoceles: the superior gluteal artery perforator flap. Plast Reconstr Surg 114(7):1864–1868
Atik B, Tan O, Mutaf M, Senel B, Yilmaz N, Kiymaz N (2008) Skin perforators of back region: anatomical study and clinical applications. Ann Plast Surg 60(1):70–75
De Brito Henriques JG, Filho GP, Gusmao SN, Henriques KSW, Miranda ME (2007) Intraoperative acute tissue expansion for the closure of large myelomeningoceles. J Neurosurg 107(2 Suppl):98–102
Luce EA, Walsh J (1985) Wound closure of the myelomeningocele defect. Plast Reconstr Surg 75(3):389–393
Moore TS, Dreyer TM, Bevin AG (1984) Closure of large spina bifida cystica defects with bilateral bipedicled musculocutaneous flaps. Plast Reconstr Surg 73(2):288–292
Campobasso P, Pesce C, Costa L, Cimaglia ML (2004) The use of the Limberg skin flap for closure of large lumbosacral myelomeningoceles. Pediatr Surg Int 20(2):144–147
Ulusoy MG, Kocer U, Sungur N, Karaaslan O, Kankaya Y, Ozdemir R, Gumus M (2005) Closure of meningomyelocele defects with bilateral modified V-Y advancement flaps. Ann Plast Surg 54(6):640–644
Kankaya Y, Sungur N, Aslan ÖÇ, Ozer K, Ulusoy MG, Karatay M, Oruç M, Gürsoy K, Karaaslan Ö, Koçer U (2015) Alternative method for the reconstruction of meningomyelocele defects: V-Y rotation and advancement flap. J Neurosurg Pediatr 15(5):467–474
Shim JH, Hwang NH, Yoon ES, Dhong ES, Kim DW, Kim SD (2016) Closure of myelomeningocele defects using a Limberg flap or direct repair. Arch Plast Surg 43(1):26–31
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Atalay, T., Oktay, K., Guzel, E. et al. Comparison of dorsal intercostal perforator artery flap and primary closure in myelomeningocele repair. Childs Nerv Syst 37, 229–233 (2021). https://doi.org/10.1007/s00381-020-04796-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04796-z