Abstract
Background
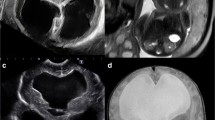
Fetal ventriculomegaly (VM) is a frequent finding in prenatal ultrasound. Rather than a proper diagnosis, VM is a sonographic sign, making prenatal counseling a complex and challenging undertaking. VM can range from severe pathologic processes leading to severe neurodevelopmental delay to normal variants.
Discussion
A growing number of genetic conditions with different pathophysiological mechanisms, inheritance patterns, and long-term prognosis have been associated both to isolated and complex fetal VM. These include chromosomal abnormalities, copy number variants, and several single gene diseases. In this review, we describe some of the most common genetic conditions associated with fetal VM and provide a simplified diagnostic workflow for the clinician.





Similar content being viewed by others
References
Cardoza JD, Goldstein RB, Filly RA (1988) Exclusion of fetal ventriculomegaly with a single measurement: the width of the lateral ventricular atrium. Radiology 169:711–714
Griffiths PD, Reeves MJ, Morris JE et al (2010) A prospective study of fetuses with isolated ventriculomegaly investigated by antenatal sonography and in utero MR imaging. Am J Neuroradiol 31:106–111
Gaglioti P, Oberto M, Todros T (2009) The significance of fetal ventriculomegaly: etiology, short- and long-term outcomes. Prenat Diagn 29:381–388
Van den Veyver IB (2019) Prenatally diagnosed developmental abnormalities of the central nervous system and genetic syndromes: a practical review. Prenat Diagn. https://doi.org/10.1002/pd.5520
Falip C, Blanc N, Maes E et al (2007) Postnatal clinical and imaging follow-up of infants with prenatal isolated mild ventriculomegaly: a series of 101 cases. Pediatr Radiol 37:981–989
Griffiths PD, Brackley K, Bradburn M et al (2017) Anatomical subgroup analysis of the MERIDIAN cohort: ventriculomegaly. Ultrasound Obstet Gynecol 50:736–744
Schrander-Stumpel C, Fryns JP (1998) Congenital hydrocephalus: nosology and guidelines for clinical approach and genetic counselling. Eur J Pediatr 157:355–362
Rekate HL (2008) The definition and classification of hydrocephalus: a personal recommendation to stimulate debate. Cerebrospinal Fluid Res 5:2
International Society of Ultrasound in Obstetrics & Gynecology Education Committee (2007) Sonographic examination of the fetal central nervous system: guidelines for performing the “basic examination” and the “fetal neurosonogram.”. Ultrasound Obstet Gynecol 29:109–116
Guibaud L (2009) Fetal cerebral ventricular measurement and ventriculomegaly: time for procedure standardization. Ultrasound Obstet Gynecol 34:127–130
Nyberg DA, Luthy DA, Cheng EY et al (1995) Role of prenatal ultrasonography in women with positive screen for Down syndrome on the basis of maternal serum markers. Am J Obstet Gynecol 173:1030–1035
Deren O, Mahoney MJ, Copel JA, Bahado-Singh RO (1998) Subtle ultrasonographic anomalies: do they improve the Down syndrome detection rate? Am J Obstet Gynecol 178:441–445
Sohl BD, Scioscia AL, Budorick NE, Moore TR (1999) Utility of minor ultrasonographic markers in the prediction of abnormal fetal karyotype at a prenatal diagnostic center. Am J Obstet Gynecol 181:898–903
Wax JR, Guilbert J, Mather J et al (2000) Efficacy of community-based second trimester genetic ultrasonography in detecting the chromosomally abnormal fetus. J Ultrasound Med 19:689–694
Aagaard-Tillery KM, Malone FD, Nyberg DA et al (2009) Role of second-trimester genetic sonography after Down syndrome screening. Obstet Gynecol 114:1189–1196
Duan H-L, Zhu X-Y, Zhu Y-J et al (2019) The application of chromosomal microarray analysis to the prenatal diagnosis of isolated mild ventriculomegaly. Taiwan J Obstet Gynecol 58:251–254
Pagani G, Thilaganathan B, Prefumo F (2014) Neurodevelopmental outcome in isolated mild fetal ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet Gynecol 44:254–260
Melchiorre K, Bhide A, Gika AD et al (2009) Counseling in isolated mild fetal ventriculomegaly. Ultrasound Obstet Gynecol 34:212–224
Zhao D, Cai A, Wang B et al (2018) Presence of chromosomal abnormalities in fetuses with isolated ventriculomegaly on prenatal ultrasound in China. Mol Genet Genomic Med 6:1015–1020
D’Addario V, Rossi AC (2012) Neuroimaging of ventriculomegaly in the fetal period. Semin Fetal Neonatal Med 17:310–318
Pilu G, Falco P, Gabrielli S et al (1999) The clinical significance of fetal isolated cerebral borderline ventriculomegaly: report of 31 cases and review of the literature. Ultrasound Obstet Gynecol 14:320–326
Iwamoto H, Muroi A, Sekine T et al (2019) Unusual form of obstructive hydrocephalus in association with 6q terminal deletion syndrome: a case report and literature review. Pediatr Neurosurg 54:419–423
Bromley B, Frigoletto FD, Benacerraf BR (1991) Mild fetal lateral cerebral ventriculomegaly: clinical course and outcome. Am J Obstet Gynecol 164:863–867
Graham E, Duhl A, Ural S et al (2001) The degree of antenatal ventriculomegaly is related to pediatric neurological morbidity. J Matern Fetal Neonatal Med 10:258–263
Hannon T, Tennant PWG, Rankin J, Robson SC (2012) Epidemiology, natural history, progression, and postnatal outcome of severe fetal ventriculomegaly. Obstet Gynecol 120:1345–1353
Devaseelan P, Cardwell C, Bell B, Ong S (2010) Prognosis of isolated mild to moderate fetal cerebral ventriculomegaly: a systematic review. J Perinat Med 38:401–409
Sethna F, Tennant PWG, Rankin JC, Robson S (2011) Prevalence, natural history, and clinical outcome of mild to moderate ventriculomegaly. Obstet Gynecol 117:867–876
Nicolaides KH, Berry S, Snijders RJ et al (1990) Fetal lateral cerebral ventriculomegaly: associated malformations and chromosomal defects. Fetal Diagn Ther 5:5–14
Gezer C, Ekin A, Ozeren M et al (2014) Chromosome abnormality incidence in fetuses with cerebral ventriculomegaly. J Obstet Gynaecol 34:387–391
Wang Y, Cao L, Liang D et al (2018) Prenatal chromosomal microarray analysis in fetuses with congenital heart disease: a prospective cohort study. Am J Obstet Gynecol 218:244.e1–244.e17
Wang Y, Hu P, Xu Z (2018) Copy number variations and fetal ventriculomegaly. Curr Opin Obstet Gynecol 30:104–110
Van den Hof MC, Wilson RD, Diagnostic Imaging Committee, Society of Obstetricians and Gynaecologists of Canada, Genetics Committee, Society of Obstetricians and Gynaecologists of Canada (2005) Fetal soft markers in obstetric ultrasound. J Obstet Gynaecol Can 27:592–636
Agathokleous M, Chaveeva P, Poon LCY et al (2013) Meta-analysis of second-trimester markers for trisomy 21. Ultrasound Obstet Gynecol 41:247–261
American College of Obstetricians and Gynecologists Committee on Genetics (2013) Committee Opinion No. 581: the use of chromosomal microarray analysis in prenatal diagnosis. Obstet Gynecol 122:1374–1377
Society for Maternal-Fetal Medicine (SMFM), Dugoff L, Norton ME, Kuller JA (2016) The use of chromosomal microarray for prenatal diagnosis. Am J Obstet Gynecol 215:B2–B9
Duncan A, Langlois S, Douglas Wilson R et al (2011) Use of array genomic hybridization technology in prenatal diagnosis in Canada. J Obstet Gynaecol Can 33:1256–1259
Hillman S, McMullan DJ, Maher ER, Kilby MD (2013) The use of chromosomal microarray in prenatal diagnosis. Obstet Gynaecol 15:80–84
Hu P, Wang Y, Sun R, et al (2017) Copy number variations with isolated fetal ventriculomegaly. Curr Mol Med 17
Shaffer LG, Rosenfeld JA, Dabell MP et al (2012) Detection rates of clinically significant genomic alterations by microarray analysis for specific anomalies detected by ultrasound. Prenat Diagn 32:986–995
Donnelly JC, Platt LD, Rebarber A et al (2014) Association of copy number variants with specific ultrasonographically detected fetal anomalies. Obstet Gynecol 124:83–90
Zhang Y, Huang L, Huang X et al (2018) Chromosomal aberrations and CNVs in twin fetuses with cardiovascular anomalies: comparison between monochorionic diamniotic and dichorionic diamniotic twins. Prenat Diagn 38:318–327
Martin CL, Kirkpatrick BE, Ledbetter DH (2015) Copy number variants, aneuploidies, and human disease. Clin Perinatol 42(227–42):vii
Fox NS, Monteagudo A, Kuller JA et al (2018) Mild fetal ventriculomegaly: diagnosis, evaluation, and management. Am J Obstet Gynecol 219:B2–B9
Shaheen R, Sebai MA, Patel N et al (2017) The genetic landscape of familial congenital hydrocephalus. Ann Neurol 81:890–897
Bickers DS, Adams RD (1949) Hereditary stenosis of the aqueduct of SYLVIUS as a cause of congenital hydrocephalus. Brain 72:246–262
Sun Y, Li Y, Chen M, et al (2019) A novel silent mutation in the L1CAM gene causing fetal hydrocephalus detected by whole-exome sequencing. Front Genet 10
Tully HM, Dobyns WB (2014) Infantile hydrocephalus: a review of epidemiology, classification and causes. Eur J Med Genet 57:359–368
Chow CW, Halliday JL, McD Anderson R et al (1985) Congenital absence of pyramids and its significance in genetic diseases. Acta Neuropathol 65:313–317
Vos YJ, de Walle HEK, Bos KK et al (2010) Genotype-phenotype correlations in L1 syndrome: a guide for genetic counselling and mutation analysis. J Med Genet 47:169–175
Schrander-Stumpel C, Höweler C, Jones M et al (1995) Spectrum of X-linked hydrocephalus (HSAS), MASA syndrome, and complicated spastic paraplegia (SPG1): clinical review with six additional families. Am J Med Genet 57:107–116
Huo L, Teng Z, Wang H, Liu X (2019) A novel splice site mutation in AP 1S2 gene for X-linked mental retardation in a Chinese pedigree and literature review. Brain Behav 9:e01221
Ruggeri G, Timms AE, Cheng C et al (2018) Bi-allelic mutations of CCDC88C are a rare cause of severe congenital hydrocephalus. Am J Med Genet A 176:676–681
Kousi M, Katsanis N (2016) The genetic basis of hydrocephalus. Annu Rev Neurosci 39:409–435
Rauen KA (2013) The RASopathies. Annu Rev Genomics Hum Genet 14:355–369
Roberts AE, Allanson JE, Tartaglia M, Gelb BD (2013) Noonan syndrome. Lancet 381:333–342
Ali MM, Chasen ST, Norton ME (2017) Testing for Noonan syndrome after increased nuchal translucency. Prenat Diagn 37:750–753
Bakker M, Pajkrt E, Mathijssen IB, Bilardo CM (2011) Targeted ultrasound examination and DNA testing for Noonan syndrome, in fetuses with increased nuchal translucency and normal karyotype. Prenat Diagn 31:833–840
Gaudineau A, Doray B, Schaefer E et al (2013) Postnatal phenotype according to prenatal ultrasound features of Noonan syndrome: a retrospective study of 28 cases. Prenat Diagn 33:238–241
de Mooij YM, de Mooij YM, van den Akker NMS et al (2011) Aberrant lymphatic development in euploid fetuses with increased nuchal translucency including Noonan syndrome. Prenat Diagn 31:159–166
Baldassarre G, Mussa A, Dotta A et al (2011) Prenatal features of Noonan syndrome: prevalence and prognostic value. Prenat Diagn 31:949–954
Houweling AC, de Mooij YM, van der Burgt I, et al (2010) Prenatal detection of Noonan syndrome by mutation analysis of the PTPN11 and the KRASgenes. Prenat Diagn
Allanson JE (2007) Noonan syndrome. Am J Med Genet C: Semin Med Genet 145C:274–279
Godfrey C, Clement E, Mein R et al (2007) Refining genotype phenotype correlations in muscular dystrophies with defective glycosylation of dystroglycan. Brain 130:2725–2735
Dobyns WB, Pagon RA, Armstrong D et al (1989) Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet 32:195–210
Falsaperla R, Praticò AD, Ruggieri M, et al (2016) Congenital muscular dystrophy: from muscle to brain. Ital J Pediatr 42
Low ASC, Lee SL, Tan ASA et al (2005) Difficulties with prenatal diagnosis of the walker-Warburg syndrome. Acta Radiol 46:645–651
Lacalm A, Nadaud B, Massoud M et al (2016) Prenatal diagnosis of cobblestone lissencephaly associated with Walker-Warburg syndrome based on a specific sonographic pattern. Ultrasound Obstet Gynecol 47:117–122
Schwartz RS (2011) Ciliopathies. N Engl J Med 364:1533–1543
Waters AM, Beales PL (2011) Ciliopathies: an expanding disease spectrum. Pediatr Nephrol 26:1039–1056
Badano JL, Mitsuma N, Beales PL, Katsanis N (2006) The ciliopathies: an emerging class of human genetic disorders. Annu Rev Genomics Hum Genet 7:125–148
Putoux A, Thomas S, Coene KLM et al (2011) KIF7 mutations cause fetal hydrolethalus and acrocallosal syndromes. Nat Genet 43:601–606
Sotak BN, Gleeson JG (2012) Can’t get there from here: cilia and hydrocephalus. Nat Med 18:1742–1743
Barisic I, Boban L, Loane M et al (2015) Meckel–Gruber syndrome: a population-based study on prevalence, prenatal diagnosis, clinical features, and survival in Europe. Eur J Hum Genet 23:746–752
Hartill V, Szymanska K, Sharif SM, et al (2017) Meckel–Gruber syndrome: an update on diagnosis, clinical management, and research advances. Front Pediatr 5
Khurana S, Saini V, Wadhwa V, Kaur H (2017) Meckel–Gruber syndrome: ultrasonographic and fetal autopsy correlation. J Ultrasound 20:167–170
Knopp C, Rudnik-Schöneborn S, Eggermann T et al (2015) Syndromic ciliopathies: from single gene to multi gene analysis by SNP arrays and next generation sequencing. Mol Cell Probes 29:299–307
Chen C-P (2007) Meckel syndrome: genetics, perinatal findings, and differential diagnosis. Taiwan J Obstet Gynecol 46:9–14
Saraiva JM, Baraitser M (1992) Joubert syndrome: a review. Am J Med Genet 43:726–731
Parisi MA (2009) Clinical and molecular features of Joubert syndrome and related disorders. Am J Med Genet C: Semin Med Genet 151C:326–340
Brancati F, Dallapiccola B, Valente EM (2010) Joubert syndrome and related disorders. Orphanet J Rare Dis 5:20
Zhu L, Xie L (2017) Prenatal diagnosis of Joubert syndrome: a case report and literature review. Medicine 96:e8626
Shen O, Ben-Sira L, Rosenak D, Michaelson-Cohen R (2014) Early second-trimester molar tooth sign. Fetal Diagn Ther 36:259–262
Haratz KK, Shulevitz SL, Leibovitz Z et al (2019) Fourth ventricle index: sonographic marker for severe fetal vermian dysgenesis/agenesis. Ultrasound Obstet Gynecol 53:390–395
Quarello E, Molho M, Garel C et al (2014) Prenatal abnormal features of the fourth ventricle in Joubert syndrome and related disorders. Ultrasound Obstet Gynecol 43:227–232
Bachmann-Gagescu R, Dempsey JC, Phelps IG et al (2015) Joubert syndrome: a model for untangling recessive disorders with extreme genetic heterogeneity. J Med Genet 52:514–522
Dempsey JC, Phelps IG, Bachmann-Gagescu R et al (2017) Mortality in Joubert syndrome. Am J Med Genet A 173:1237–1242
Salonen R, Herva R (1990) Hydrolethalus syndrome. J Med Genet 27:756–759
Wei Q, Zhang Y, Schouteden C et al (2016) The hydrolethalus syndrome protein HYLS-1 regulates formation of the ciliary gate. Nat Commun 7:12437
Ferrante MI, Feather SA, Bulfone A et al (2001) Identification of the gene for oral-facial-digital type I syndrome. Am J Hum Genet 68:569–576
Feather SA, Winyard PJ, Dodd S, Woolf AS (1997) Oral-facial-digital syndrome type 1 is another dominant polycystic kidney disease: clinical, radiological and histopathological features of a new kindred. Nephrol Dial Transplant 12:1354–1361
Bruel A-L, Franco B, Duffourd Y et al (2017) Fifteen years of research on oral–facial–digital syndromes: from 1 to 16 causal genes. J Med Genet 54:371–380
Bouman A, Alders M, Oostra RJ et al (2017) Oral-facial-digital syndrome type 1 in males: congenital heart defects are included in its phenotypic spectrum. Am J Med Genet A 173:1383–1389
Alby C, Boutaud L, Bonnière M et al (2018) In utero ultrasound diagnosis of corpus callosum agenesis leading to the identification of orofaciodigital type 1 syndrome in female fetuses. Birth Defects Res 110:382–389
Drury S, Williams H, Trump N et al (2015) Exome sequencing for prenatal diagnosis of fetuses with sonographic abnormalities. Prenat Diagn 35:1010–1017
Thauvin-Robinet C, Rousseau T, Durand C et al (2001) Familial orofaciodigital syndrome type I revealed by ultrasound prenatal diagnosis of porencephaly. Prenat Diagn 21:466–470
Hogan GR, Bauman ML (1971) Hydrocephalus in Apert’s syndrome. J Pediatr 79:782–787
Murovic JA, Posnick JC, Drake JM et al (1993) Hydrocephalus in Apert syndrome: a retrospective review. Pediatr Neurosurg 19:151–155
Fukumitsu H, Ohmiya M, Nitta A et al (2000) Aberrant expression of neurotrophic factors in the ventricular progenitor cells of infant congenitally hydrocephalic rats. Childs Nerv Syst 16:516–521
Tan AP, Mankad K (2018) Apert syndrome: magnetic resonance imaging (MRI) of associated intracranial anomalies. Childs Nerv Syst 34:205–216
Collmann H, Sörensen N, Krauss J (2005) Hydrocephalus in craniosynostosis: a review. Childs Nerv Syst 21:902–912
Hassed S, Shewmake K, Teo C et al (1997) Shprintzen-Goldberg syndrome with osteopenia and progressive hydrocephalus. Am J Med Genet 70:450–453
Pierre-Kahn A, Hirsch JF, Renter D et al (1980) Hydrocephalus and achondroplasia. Pediatr Neurosurg 7:205–219
Swift D, Nagy L, Robertson B (2012) Endoscopic third ventriculostomy in hydrocephalus associated with achondroplasia. J Neurosurg Pediatr 9:73–81
Steinbok P, Hall J, Flodmark O (1991) Hydrocephalus in achondroplasia: the possible role of intracranial venous hypertension. Ann Rev Hydrocephalus:104–104
McKechnie L, Vasudevan C, Levene M (2012) Neonatal outcome of congenital ventriculomegaly. Semin Fetal Neonatal Med 17:301–307
Laskin MD, Kingdom J, Toi A et al (2005) Perinatal and neurodevelopmental outcome with isolated fetal ventriculomegaly: a systematic review. J Matern Fetal Neonatal Med 18:289–298
Wyldes M (2004) Isolated mild fetal ventriculomegaly. Arch Dis Child Fetal Neonatal Ed 89:9F–13F
Pisapia JM, Sinha S, Zarnow DM et al (2017) Fetal ventriculomegaly: diagnosis, treatment, and future directions. Childs Nerv Syst 33:1113–1123
Breeze ACG, Alexander PMA, Murdoch EM et al (2007) Obstetric and neonatal outcomes in severe fetal ventriculomegaly. Prenat Diagn 27:124–129
Carta S, Kaelin Agten A, Belcaro C, Bhide A (2018) Outcome of fetuses with prenatal diagnosis of isolated severe bilateral ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet Gynecol 52:165–173
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Etchegaray, A., Juarez-Peñalva, S., Petracchi, F. et al. Prenatal genetic considerations in congenital ventriculomegaly and hydrocephalus. Childs Nerv Syst 36, 1645–1660 (2020). https://doi.org/10.1007/s00381-020-04526-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04526-5