Abstract
Purpose
Posterior fossa ependymomas (PFE) are among the most frequently occurring solid tumors in children. Their definitive treatment is surgical excision and adjuvant radio-chemotherapy. This study aimed to investigate prognostic effects of age, H3K27me3 status, extent of resection, radiation treatment (RT), Ki67 index, WHO grade, and ATRX and H3K27M mutations in PFE patients.
Methods
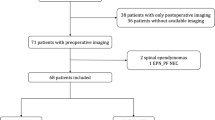
This retrospective study included 42 pediatric patients with PFE who had undergone operation at our institution between 1996 and 2018. Patient demographics and treatment information were obtained from patient notes. Information on radiological location of tumors (median vs paramedian), extent of tumor resection, and recurrence was obtained from preoperative and postoperative magnetic resonance imaging. Formalin-fixed paraffin-embedded tumor samples were evaluated for H3K27me3 immunostaining, Ki67 index, WHO grades, and ATRX and H3K27M mutations. Tumor samples with global reduction in H3K27me3 were grouped as posterior fossa ependymoma group A (PFA) and those with H3K27me3 nuclear immunopositivity as posterior fossa ependymoma group B (PFB). We evaluated the cohort’s 5-year progression-free survival (PFS) and overall survival (OS).
Results
There were 20 (47.6%) female and 22 (52.4%) male patients in the cohort. The mean age of patients was 4.4 (range, 0.71–14.51) years. Overall, tumors in 31 (73.8%) and 11 (26.2%) patients were found to be PFA and PFB, respectively. There was no statistically significant age or sex difference between PFA and PFB. All patients received chemotherapy, whereas only 28 (66.6%) received RT. The WHO grades of PFA were statistically higher than those of PFB. There was no significant difference between PFA and PFB in terms of extent of resection, disease recurrence, and survival parameters. Nine of 42 tumor samples had ATRX mutations. One patient with PFA showed H3K27M mutation. Age, WHO grade, H3K27me3 status, and RT had no effect on patients’ PFS and OS. Patients with total surgical excisions had significantly better PFS and OS rates. Those with Ki67 < 50% also had better OS rates.
Conclusions
Determining H3K27me3 status by immunohistochemistry is a widely accepted method for molecular subgrouping of PFEs. Most of the reports in the literature state that molecular subgroups of PFEs have significantly different clinical outcomes. However, in our present series, we have shown that the extent of surgical excision is still the most important prognostic indicator in PFEs. We also conclude that the prognostic effect of H3K27me3 status–based molecular subgrouping may be minimized with a more aggressive surgical strategy followed in PFAs.






Similar content being viewed by others
References
Ostrom QT, Cioffi G, Gittleman H, Patil N, Waite K, Kruchko C, Barnholtz-Sloan JS (2019) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro-Oncology 21:v1–v100
Komori T, Sasaki H, Yoshida K (2016) Revised WHO classification of tumours of the central nervous system:summary of the revision and perspective. No Shinkei Geka 44:625–635
Poppleton H, Gilbertson RJ (2007) Stem cells of ependymoma. Br J Cancer 96:6–10
Dyer S, Prebble E, Davison V, Davies P, Ramani P, Ellison D, Grundy R (2002) Genomic imbalances in pediatric intracranial ependymomas define clinically relevant groups. Am J Pathol 161:2133–2141
Ellison DW, Kocak M, Figarella-Branger D, Felice G, Catherine G, Pietsch T, Frappaz D, Massimino M, Grill J, Boyett JM, Grundy RG (2011) Histopathological grading of pediatric ependymoma: reproducibility and clinical relevance in European trial cohorts. J Negat Results Biomed 10:7
Pajtler KW, Witt H, Sill M, Jones DT, Hovestadt V, Kratochwil F, Wani K, Tatevossian R, Punchihewa C, Johann P, Reimand J, Warnatz HJ, Ryzhova M, Mack S, Ramaswamy V, Capper D, Schweizer L, Sieber L, Wittmann A, Huang Z, van Sluis P, Volckmann R, Koster J, Versteeg R, Fults D, Toledano H, Avigad S, Hoffman LM, Donson AM, Foreman N, Hewer E, Zitterbart K, Gilbert M, Armstrong TS, Gupta N, Allen JC, Karajannis MA, Zagzag D, Hasselblatt M, Kulozik AE, Witt O, Collins VP, von Hoff K, Rutkowski S, Pietsch T, Bader G, Yaspo ML, von Deimling A, Lichter P, Taylor MD, Gilbertson R, Ellison DW, Aldape K, Korshunov A, Kool M, Pfister SM (2015) Molecular classification of ependymal tumors across all CNS compartments, Histopathological grades, and age groups. Cancer Cell 27:728–743
Ramaswamy V, Taylor MD (2016) Treatment implications of posterior fossa ependymoma subgroups. Chin J Cancer 35:93
Ramaswamy V, Hielscher T, Mack SC, Lassaletta A, Lin T, Pajtler KW, Jones DT, Luu B, Cavalli FM, Aldape K, Remke M, Mynarek M, Rutkowski S, Gururangan S, McLendon RE, Lipp ES, Dunham C, Hukin J, Eisenstat DD, Fulton D, van Landeghem FK, Santi M, van Veelen ML, Van Meir EG, Osuka S, Fan X, Muraszko KM, Tirapelli DP, Oba-Shinjo SM, Marie SK, Carlotti CG, Lee JY, Rao AA, Giannini C, Faria CC, Nunes S, Mora J, Hamilton RL, Hauser P, Jabado N, Petrecca K, Jung S, Massimi L, Zollo M, Cinalli G, Bognar L, Klekner A, Hortobagyi T, Leary S, Ermoian RP, Olson JM, Leonard JR, Gardner C, Grajkowska WA, Chambless LB, Cain J, Eberhart CG, Ahsan S, Massimino M, Giangaspero F, Buttarelli FR, Packer RJ, Emery L, Yong WH, Soto H, Liau LM, Everson R, Grossbach A, Shalaby T, Grotzer M, Karajannis MA, Zagzag D, Wheeler H, von Hoff K, Alonso MM, Tunon T, Schuller U, Zitterbart K, Sterba J, Chan JA, Guzman M, Elbabaa SK, Colman H, Dhall G, Fisher PG, Fouladi M, Gajjar A, Goldman S, Hwang E, Kool M, Ladha H, Vera-Bolanos E, Wani K, Lieberman F, Mikkelsen T, Omuro AM, Pollack IF, Prados M, Robins HI, Soffietti R, Wu J, Metellus P, Tabori U, Bartels U, Bouffet E, Hawkins CE, Rutka JT, Dirks P, Pfister SM, Merchant TE, Gilbert MR, Armstrong TS, Korshunov A, Ellison DW, Taylor MD (2016) Therapeutic impact of cytoreductive surgery and irradiation of posterior fossa ependymoma in the molecular era: a retrospective multicohort analysis. J Clin Oncol 34:2468–2477
Zapotocky M, Beera K, Adamski J, Laperierre N, Guger S, Janzen L, Lassaletta A, Figueiredo Nobre L, Bartels U, Tabori U, Hawkins C, Urbach S, Tsang DS, Dirks PB, Taylor MD, Bouffet E, Mabbott DJ, Ramaswamy V (2019) Survival and functional outcomes of molecularly defined childhood posterior fossa ependymoma: cure at a cost. Cancer
Healey EA, Barnes PD, Kupsky WJ, Scott RM, Sallan SE, Black PM, Tarbell NJ (1991) The prognostic significance of postoperative residual tumor in ependymoma. Neurosurgery 28: 666–671; discussion 671-662
Wani K, Armstrong TS, Vera-Bolanos E, Raghunathan A, Ellison D, Gilbertson R, Vaillant B, Goldman S, Packer RJ, Fouladi M, Pollack I, Mikkelsen T, Prados M, Omuro A, Soffietti R, Ledoux A, Wilson C, Long L, Gilbert MR, Aldape K, Collaborative Ependymoma Research N (2012) A prognostic gene expression signature in infratentorial ependymoma. Acta Neuropathol 123:727–738
Tihan T, Zhou T, Holmes E, Burger PC, Ozuysal S, Rushing EJ (2008) The prognostic value of histological grading of posterior fossa ependymomas in children: a Children’s Oncology Group study and a review of prognostic factors. Mod Pathol 21:165–177
Mack SC, Taylor MD (2017) Put away your microscopes: the ependymoma molecular era has begun. Curr Opin Oncol 29:443–447
Witt H, Mack SC, Ryzhova M, Bender S, Sill M, Isserlin R, Benner A, Hielscher T, Milde T, Remke M, Jones DT, Northcott PA, Garzia L, Bertrand KC, Wittmann A, Yao Y, Roberts SS, Massimi L, Van Meter T, Weiss WA, Gupta N, Grajkowska W, Lach B, Cho YJ, von Deimling A, Kulozik AE, Witt O, Bader GD, Hawkins CE, Tabori U, Guha A, Rutka JT, Lichter P, Korshunov A, Taylor MD, Pfister SM (2011) Delineation of two clinically and molecularly distinct subgroups of posterior fossa ependymoma. Cancer Cell 20:143–157
UK-I JM, Taylor MD, Raybaud C (2010) Posterior fossa ependymomas: new radiological classification with surgical correlation. Childs Nerv Syst 26:1765–1772
Kersemans V, Cornelissen B, Allen PD, Beech JS, Smart SC (2013) Subcutaneous tumor volume measurement in the awake, manually restrained mouse using MRI. J Magn Reson Imaging 37:1499–1504
Lundin P, Pedersen F (1992) Volume of pituitary macroadenomas: assessment by MRI. J Comput Assist Tomogr 16:519–528
Tsang DS, Burghen E, Klimo P Jr, Boop FA, Ellison DW, Merchant TE (2018) Outcomes after Reirradiation for recurrent pediatric intracranial ependymoma. Int J Radiat Oncol Biol Phys 100:507–515
Bennetto L, Foreman N, Harding B, Hayward R, Ironside J, Love S, Ellison D (1998) Ki-67 immunolabelling index is a prognostic indicator in childhood posterior fossa ependymomas. Neuropathol Appl Neurobiol 24:434–440
Rogers L, Pueschel J, Spetzler R, Shapiro W, Coons S, Thomas T, Speiser B (2005) Is gross-total resection sufficient treatment for posterior fossa ependymomas? J Neurosurg 102:629–636
Stuben G, Stuschke M, Kroll M, Havers W, Sack H (1997) Postoperative radiotherapy of spinal and intracranial ependymomas: analysis of prognostic factors. Radiother Oncol 45:3–10
Pajtler KW, Wen J, Sill M, Lin T, Orisme W, Tang B, Hubner JM, Ramaswamy V, Jia S, Dalton JD, Haupfear K, Rogers HA, Punchihewa C, Lee R, Easton J, Wu G, Ritzmann TA, Chapman R, Chavez L, Boop FA, Klimo P, Sabin ND, Ogg R, Mack SC, Freibaum BD, Kim HJ, Witt H, Jones DTW, Vo B, Gajjar A, Pounds S, Onar-Thomas A, Roussel MF, Zhang J, Taylor JP, Merchant TE, Grundy R, Tatevossian RG, Taylor MD, Pfister SM, Korshunov A, Kool M, Ellison DW (2018) Molecular heterogeneity and CXorf67 alterations in posterior fossa group A (PFA) ependymomas. Acta Neuropathol 136:211–226
Haresh KP, Gandhi AK, Mallick S, Benson R, Gupta S, Sharma DN, Julka PK, Rath GK (2017) Prognostic factors and survival outcomes of intracranial ependymoma treated with multimodality approach. Indian J Med Paediatr Oncol 38:420–426
Araki A, Chocholous M, Gojo J, Dorfer C, Czech T, Heinzl H, Dieckmann K, Ambros IM, Ambros PF, Slavc I, Haberler C (2016) Chromosome 1q gain and tenascin-C expression are candidate markers to define different risk groups in pediatric posterior fossa ependymoma. Acta Neuropathol Commun 4:88
Godfraind C, Kaczmarska JM, Kocak M, Dalton J, Wright KD, Sanford RA, Boop FA, Gajjar A, Merchant TE, Ellison DW (2012) Distinct disease-risk groups in pediatric supratentorial and posterior fossa ependymomas. Acta Neuropathol 124:247–257
Bayliss J, Mukherjee P, Lu C, Jain SU, Chung C, Martinez D, Sabari B, Margol AS, Panwalkar P, Parolia A, Pekmezci M, McEachin RC, Cieslik M, Tamrazi B, Garcia BA, La Rocca G, Santi M, Lewis PW, Hawkins C, Melnick A, David Allis C, Thompson CB, Chinnaiyan AM, Judkins AR, Venneti S (2016) Lowered H3K27me3 and DNA hypomethylation define poorly prognostic pediatric posterior fossa ependymomas. Sci Transl Med 8:366ra161
Zhang RR, Kuo JS (2017) Reduced H3K27me3 is a new epigenetic biomarker for pediatric posterior fossa ependymomas. Neurosurgery 81:N7–N8
Reinhardt A, Stichel D, Schrimpf D, Sahm F, Korshunov A, Reuss DE, Koelsche C, Huang K, Wefers AK, Hovestadt V, Sill M, Gramatzki D, Felsberg J, Reifenberger G, Koch A, Thomale UW, Becker A, Hans VH, Prinz M, Staszewski O, Acker T, Dohmen H, Hartmann C, Mueller W, Tuffaha MSA, Paulus W, Hess K, Brokinkel B, Schittenhelm J, Monoranu CM, Kessler AF, Loehr M, Buslei R, Deckert M, Mawrin C, Kohlhof P, Hewer E, Olar A, Rodriguez FJ, Giannini C, NageswaraRao AA, Tabori U, Nunes NM, Weller M, Pohl U, Jaunmuktane Z, Brandner S, Unterberg A, Hanggi D, Platten M, Pfister SM, Wick W, Herold-Mende C, Jones DTW, von Deimling A, Capper D (2018) Anaplastic astrocytoma with piloid features, a novel molecular class of IDH wildtype glioma with recurrent MAPK pathway, CDKN2A/B and ATRX alterations. Acta Neuropathol 136:273–291
Ebrahimi A, Skardelly M, Bonzheim I, Ott I, Muhleisen H, Eckert F, Tabatabai G, Schittenhelm J (2016) ATRX immunostaining predicts IDH and H3F3A status in gliomas. Acta Neuropathol Commun 4:60
Wiestler B, Capper D, Holland-Letz T, Korshunov A, von Deimling A, Pfister SM, Platten M, Weller M, Wick W (2013) ATRX loss refines the classification of anaplastic gliomas and identifies a subgroup of IDH mutant astrocytic tumors with better prognosis. Acta Neuropathol 126:443–451
Orillac C, Thomas C, Dastagirzada Y, Hidalgo ET, Golfinos JG, Zagzag D, Wisoff JH, Karajannis MA, Snuderl M (2016) Pilocytic astrocytoma and glioneuronal tumor with histone H3 K27M mutation. Acta Neuropathol Commun 4:84
Gessi M, Capper D, Sahm F, Huang K, von Deimling A, Tippelt S, Fleischhack G, Scherbaum D, Alfer J, Juhnke BO, von Hoff K, Rutkowski S, Warmuth-Metz M, Chavez L, Pfister SM, Pietsch T, Jones DT, Sturm D (2016) Evidence of H3 K27M mutations in posterior fossa ependymomas. Acta Neuropathol 132:635–637
Ryall S, Guzman M, Elbabaa SK, Luu B, Mack SC, Zapotocky M, Taylor MD, Hawkins C, Ramaswamy V (2017) H3 K27M mutations are extremely rare in posterior fossa group a ependymoma. Childs Nerv Syst 33:1047–1051
Perilongo G, Massimino M, Sotti G, Belfontali T, Masiero L, Rigobello L, Garre L, Carli M, Lombardi F, Solero C, Sainati L, Canale V, del Prever AB, Giangaspero F, Andreussi L, Mazza C, Madon E (1997) Analyses of prognostic factors in a retrospective review of 92 children with ependymoma: Italian pediatric Neuro-oncology group. Med Pediatr Oncol 29:79–85
Zacharoulis S, Ashley S, Moreno L, Gentet JC, Massimino M, Frappaz D (2010) Treatment and outcome of children with relapsed ependymoma: a multi-institutional retrospective analysis. Childs Nerv Syst 26:905–911
Hanzlik E, Woodrome SE, Abdel-Baki M, Geller TJ, Elbabaa SK (2015) A systematic review of neuropsychological outcomes following posterior fossa tumor surgery in children. Childs Nerv Syst 31:1869–1875
Khatua S, Ramaswamy V, Bouffet E (2017) Current therapy and the evolving molecular landscape of paediatric ependymoma. Eur J Cancer 70:34–41
Thompson YY, Ramaswamy V, Diamandis P, Daniels C, Taylor MD (2015) Posterior fossa ependymoma: current insights. Childs Nerv Syst 31:1699–1706
Sanford RA, Merchant TE, Zwienenberg-Lee M, Kun LE, Boop FA (2009) Advances in surgical techniques for resection of childhood cerebellopontine angle ependymomas are key to survival. Childs Nerv Syst 25:1229–1240
Kilday JP, Rahman R, Dyer S, Ridley L, Lowe J, Coyle B, Grundy R (2009) Pediatric ependymoma: biological perspectives. Mol Cancer Res 7:765–786
Zacharoulis S, Levy A, Chi SN, Gardner S, Rosenblum M, Miller DC, Dunkel I, Diez B, Sposto R, Ji L, Asgharzadeh S, Hukin J, Belasco J, Dubowy R, Kellie S, Termuhlen A, Finlay J (2007) Outcome for young children newly diagnosed with ependymoma, treated with intensive induction chemotherapy followed by myeloablative chemotherapy and autologous stem cell rescue. Pediatr Blood Cancer 49:34–40
Acknowledgments
We would like to thank Dr. Alp Inanıcı for his valuable cooperation during statistical data analysis of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This retrospective study was approved by ethical committee of Acibadem University School of Medicine, Istanbul, Turkey. Informed consent was obtained from patients’ legal guardians.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tanrıkulu, B., Danyeli, A.E. & Özek, M.M. Is H3K27me3 status really a strong prognostic indicator for pediatric posterior fossa ependymomas? A single surgeon, single center experience. Childs Nerv Syst 36, 941–949 (2020). https://doi.org/10.1007/s00381-020-04518-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04518-5