Abstract
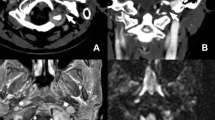
Langerhans cell histiocytosis (LCH) is a rare disease of young children that can be difficult to diagnose and treat. Clinical manifestations can sometimes be quite unusual, and bony lesions can reach a large size before treatment is sought. We present a unique case of a 3-year-old male child with a painless giant calvarial defect and cystic swelling. Complete removal of the cyst with curettage of the involved bone margins and cranioplasty was done using bone cement (polymethyl methacrylate, PMMA). However, there was a flare up of the disease due to abnormal inflammatory reaction to PMMA, and cranioplasty bone flap had to be removed. The child did well after PMMA bone flap removal.
LCH should be suspected in a male child presenting with a large calvarial defect and no history of trauma. The use of materials, viz., hydroxyapatite, poly-DL-lactide (PDLLA), and PMMA for cranioplasty in LCH, may cause reactivation of the disease process and therefore must be used cautiously in these patients.


Similar content being viewed by others
References
Abla O, Weitzman S (2015) Treatment of Langerhans cell histiocytosis: role of BRAF/MAPK inhibition. Hematology Am Soc Hematol Educ Program 2015:565–570
Anthony DC, Tucker JA (1996) Langerhans cell histiocytosis (histiocytosis X). In: Wilkins RH, Rengachary SS (eds) Neurosurgery, 2nd edn. McGraw-Hill, New York, pp 1751–1756
Atsumi Y, Saito Y, Hataya H, Yuza Y (2019) Initial symptoms of Langerhans cell histiocytosis: a case series. Glob Pediatr Health 6:2333794X19857377
Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F (1997) Langerhans’-cell histiocytosis in adults. Med Pediatr Oncol 28:9–14
Ceci A, de Terlizzi M, Colella R et al (1993) Langerhans cell histiocytosis in childhood: results from the Italian cooperative AIEOP-CNR-H.X ‘83 study. Med Pediatr Oncol 21:259–264
Cochrane LA, Prince M, Clarke K (2003) Langerhans’ cell histiocytosis in the paediatric population: presentation and treatment of head and neck manifestations. J Otolaryngol 32:33–37
Gosal JS, Behari S, Joseph J et al (2018) Surgical excision of large-to-giant petroclival meningiomas focusing on the middle fossa approaches: the lessons learnt. Neurol India 66(5):1434–1446
Majumder A, Wick CC, Collins R, Booth TN, Isaacson B, Kutz JW (2017) Pediatric Langerhans cell histiocytosis of the lateral skull base. Int J Pediatr Otorhinolaryngol 99:135–140
Moteki Y, Yamada M, Shimizu A, Suzuki N, Kobayashi T (2019) Langerhans cell histiocytosis of the skull in a Burr hole site covered with hydroxyapatite material. World Neurosurg 122:632–637
Sadashiva N, Baruah S, Rao S, Mahadevan A, Rao KN, Vazhayil V, Somanna S (2017) Eosinophilic granuloma of skull with fluid level and epidural hematoma: a case report and review of the literature. Pediatr Neurosurg 52(1):41–45
Ugga L, Cuocolo R, Cocozza S, Ponsiglione A, Stanzione A, Chianca V, D'Amico A, Brunetti A, Imbriaco M (2018) Spectrum of lytic lesions of the skull: a pictorial essay. Insights Imaging 9(5):845–856
Yamaguchi S, Oki S, Kurisu K (2004) Spontaneous regression of Langerhans cell histiocytosis: a case report. Surg Neurol 62(2):136–140
Yee KS, Combs PD, Kelley PK, George TM, Harshbarger RJ (2013) Resorption of PDLLA plates as a nidus for recurrent Langerhans cell histiocytosis. Pediatr Neurosurg 49(4):243–247
Zhang XH, Zhang J, Chen ZH et al (2017) Langerhans cell histiocytosis of skull: a retrospective study of 18 cases. Ann Palliat Med 6:159–164
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gosal, J.S., Ruparelia, J., Garg, M. et al. Giant skull vault defect in a child caused by Langerhans cell histiocytosis: the “calvaria-eating disease”. Childs Nerv Syst 36, 651–654 (2020). https://doi.org/10.1007/s00381-019-04459-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04459-8