Abstract
Purpose
Cranial lacunae (foci of attenuated calvarial bone) are CT equivalents of “copper beating” seen on plain skull radiographs in children with craniosynostosis. The qualitative presence of copper beating has not been found to be useful for the diagnosis of intracranial hypertension (IH) in these patients. 3D morphometric analysis (3DMA) allows a more systematic and quantitative assessment of calvarial attenuation. We used 3DMA to examine the relationship between cranial lacunae and IH in children with Crouzon and Apert syndromic craniosynostosis.
Methods
Patients were divided into IH and non-IH groups defined on an intention-to-treat basis. Pre-operative CT scans were converted into 3D skull models and processed to quantify lacunae as a percentage of calvarium surface area (LCP). This was done on individual bone and whole skull basis.
Results
Eighteen consecutive children with Crouzon’s syndrome and 17 with Apert syndrome were identified. Median age at CT scan was 135 days (range 6–1778). Of the 35 children, 21 required surgery for IH at median age of 364 days (range 38–1710). Of these 21 children, 14 had lacunae with mean LCP of 3% (0–28%). Of the 14 non-IH children, 8 had lacunae with mean LCP of 2% (0–8%). LCP was not significantly different between IH and non-IH groups. Parietal bones were most likely to show lacunae (IH 14/21, non-IH 9/14), followed by occipital (IH 8/21, non-IH 3/14), and frontal (IH 6/21, non-IH 2/14).
Conclusion
Results suggest that cranial lacunae, measured using quantitative 3DMA, do not correlate with IH, in agreement with evidence from qualitative plain skull radiograph studies.
Similar content being viewed by others
Introduction
Craniosynostosis is defined as the premature fusion of skull sutures and can cause cranial deformities and functional problems including intracranial hypertension (IH), which in turn may cause ophthalmic and neurological deficits. Syndromic forms, such as Crouzon syndrome (CS) and Apert syndrome (AS), are associated with variable phenotypes but multisutural craniosynostosis and IH are much more common than in single-suture disease [1, 2].
The diagnosis of IH in children with syndromic craniosynostosis can be challenging. “Textbook” symptoms such as headache and vomiting are often absent [3], and the gold standard for diagnosis remains invasive monitoring, which, while safe, does carry a small complication rate and need for inpatient admission [4, 5]. Therefore, there has been great historical interest in non-invasive modalities for assessing the presence or absence of IH. Options that have been utilized, with varying degrees of success and uptake, include fundoscopy [6], visual electrodiagnostic tests [7], optical coherence tomography [8], and optic nerve sheath ultrasound [9]. Because none of these tests are 100% sensitive or specific, there has also been interest in exploring radiographic correlates for IH in craniosynostosis. A common finding in children with craniosynostosis is the presence of “copper beating” or “digital markings” on plain radiography. Because these radiological findings are the correlate of the intraoperative finding of impressions made by brain gyri on the inner table, it was thought that they may reflect the result of prolonged intracranial hypertension “pushing” the brain against the inside of the skull. However, several studies have shown that the presence or absence of copper beating is not helpful in predicting intracranial hypertension [3, 5, 6, 10]. However, copper beating is a subjective measure based on plain radiography. Modern imaging techniques allow accurate three-dimensional reconstruction (3DR) of the skull. On 3DR, thinned areas of bone that on plain radiographs appear as copper beating are represented as cranial “holes” or lacunae (Fig. 1). These are a common feature of 3DR CT scans of infants with syndromic craniosynostosis.
Modern image processing techniques can measure the extent of the cranial lacunae in relation to the overall skull surface area. This allows a quantitative measurement of the extent of bone thinning compared to the qualitative assessment available on plain radiography. Unlike many craniofacial units, our philosophy at Great Ormond Street Hospital has been not to perform prophylactic vault expansion surgery on syndromic craniosynostosis cases but rather wait until the child demonstrates evidence of IH on clinical, ophthalmic, electrophysiological, or direct measurement grounds [1, 2, 7, 11]. Therefore, we have a cohort of patients in which we can compare extent of cranial lacunae to IH on an intention-to-treat basis, to assess whether the more quantitative measure on 3DR CT is more or less useful than the qualitative assessment of copper beating on plain radiograph. We undertook this analysis in cohorts of children with Crouzon and Apert syndrome, two of the major forms of syndromic craniosynostosis.
Methods
Patient identification and exclusion criteria
Consecutive newly referred patients with a genetically confirmed diagnosis of either Crouzon or Apert, from 2014 to 2016, were identified from our hospital Craniofacial Patient Platform database. Inclusion criteria were as follows. (1) Confirmed diagnosis of Crouzon or Apert. (2) Availability of complete fine-cut index (pre-operative) CT head scan suitable for 3DR. (3) No previous cranial vault surgery (for example, patients initially managed, and operated, at other centers). Patients who had previous non-vault cranial surgery, such as ventriculoperitoneal shunt insertion, were included. (4) Complete set of clinical records to allow accurate assessment of presence or absence of IH as defined below.
Definition of intracranial hypertension
IH was defined on an “intention-to-treat” basis. Patients were divided into IH or non-IH groups dependent on whether they had surgical treatment aimed at cure of IH within 2 years of the index CT scan. Triggers for surgery in our department are (1) clinical—bulging fontanelle, headache, vomiting; (2) ophthalmologic—papilloedema, disc changes, deterioration in electrophysiological tests of vision; and (3) radiologic—progressive hydrocephalus, obliteration of basal cisterns, or progressive cerebellar tonsillar ectopia. We have previously described our protocols around management of IH in Crouzon and Apert [1, 2, 7, 11]. The IH criteria was established by a clinician (GJ) who was not involved with the 3DR surface area analysis (AM and NRF). The data was only matched after completion of both the 3DR surface area analysis and the decision on the clinical group, allowing an element of blinding into the analysis.
Measurement of cranial lacunae
The head CT scans containing the most number of slices were selected and exported in DICOM format to OsiriX (Pixmeo, Bernex, Switzerland). 3DRs of the skull were then created with a threshold of 245 Hounsfield Units (HU) and exported to 3D surface meshes in stereolithography (STL) format.
STL files were then post-processed using Meshmixer (Autodesk Inc., Toronto, ON, Canada). Extraneous objects such as nasogastric and endotracheal tubes were removed and the 3D models were re-meshed at 60% of their original density. The skull was then repositioned and sectioned along the Frankfurt plane with retention of the superior section, such that only the calvarium was being processed. The calvarium was separated into the paired frontal, paired parietal and single occipital bones (five bones per case). The external surface area of each of these bones was calculated. Thereafter, the cranial lacunae were defined (Fig. 2) and automatically filled using the appropriate function on Meshmixer and the external surface areas were re-calculated, allowing a calculation of the size of the lacunae in relation to the overall bone. Cranial lacunae could therefore be expressed as a percentage of surface area, on both on individual bone and whole skull basis (lacunae-calvarial proportion).
Statistical analysis
Student’s paired t test was used and significance was defined as a p < 0.05. SPSS Version 24 was used to run the statistical analyses (IBM Corp., Armonk, NY, USA).
Results
Patient identification and demographics
An initial search of our institution’s Craniofacial Patient Platform identified 45 potential CS and AS cases. Of these, 38 (84%) had pre-op fine-cut CT head scans available. In 2 cases, the CTs were unsuitable for conversion into 3DR, and in 1 follow-up clinical information was not available, leaving a total of 35 cases for analysis (Fig. 3).
Of these 35 cases, 18 had a diagnosis of CS, and 17 had AS. Of the 18 CS patients, 9 were males and 9 were females. Of the AS patients, 11 were males and 6 were females. The overall median age at index CT scan was 135 days old (range 6–1778 days old). The median age at index CT scan for CS patients was 498 days old (range 37–1778 days old), and the median age at index CT scan for AS patients was 77 days old (range 6–186 days old).
Cranial lacunae
The presence of cranial lacunae was noted in 22 of 35 (63%) cases. For all 35 cases, the overall mean lacunae-calvarial proportion (LCP) was 3% (range 0 to 28%). The most commonly affected bone across the whole series were the parietal bones (23/35, 66%), followed by the occipital bones (11/35, 31%), with the frontal bones least affected (8/35, 23%). Mean LCP for each bone was parietal 3% (range 0–33%), occipital 2% (range 0–19%), and frontal 2% (range 0–41%) (Fig. 4). LCP decreased with age, with 21 of 27 patients aged less than 18 months having cranial lacunae (mean LCP 4%, range 0–28%), with only 1 of 8 patients aged over 18 months having lacunae (mean LCP 0%, range 0–1%). There was no statistical difference in LCP between the group aged less than 18 months and the group aged more than 18 months (p = 0.13).
Relationship to intracranial hypertension
Of the 35 patients in the study, 21 (60%) patients were assigned to the IH group as they had operative treatment to relieve IH. Seventeen patients underwent posterior vault expansion, 2 had insertion of ventriculoperitoneal shunt, 1 had spring-assisted cranioplasty, and 1 had fronto-orbital advancement. The remaining non-operated 14 patients were assigned to the non-IH group.
Of these 21 children in the IH group, 14 (67%) had the presence of lacunae, with a mean LCP of 3% (range 0–28%). Of the 14 children in the non-IH group, 8 (58%) had lacunae, with a mean LCP of 2 (range 0–8%) (Fig. 5). There was no statistical difference between the two groups (p = 0.4). For the two groups, a number of patients with craniolacunae and LCP for the individual calvarial bones are displayed in Table 1. There were no significant differences detected between the two groups when scans were subdivided into individual calvarial bones (p = 0.4, p = 0.5, and p = 0.7 for frontal, parietal, and occipital bones respectively).
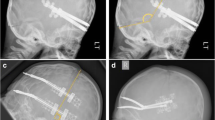
The highest LCP in the series was 28% (a female with CS, FGFR2 c.1040C > G mutation), with the second highest being 19% (a male with AS). These were outliers in the series, with the rest of the 33 patients falling between 0 and 8% LCP (Fig. 6). Both of these very high LCP patients had IH (Fig. 7).
a 3DR CT images from the most severe AS case (AS12) and b 3DR CT images from the most severe CS case (CS9). Although the “cloverleaf” skull deformity seen in CS9 resembles that seen in Pfeiffer, this girl had no associated limb defects and genetics confirmed Crouzon (FGFR2 mutation c.1040 C > G, p.Ser347Cys)
Relationship to intracranial hypertension in Crouzon syndrome
Of the 18 CS patients, 9 were in the IH group and 9 in the non-IH group. Of the 9 in the IH group, 7 required posterior vault expansion with 2 having insertion of ventriculoperitoneal shunt. Of the 9 in the IH group, 2 (23%) had lacunae with a mean LCP of 4% (range 0–28%). In the 9 of the non-IH group, 3 (33%) had lacunae with a mean LCP of 1% (range 0–5%). There was no significant difference between groups (p = 0.4) (Fig. 5).
Relationship to intracranial hypertension in Apert syndrome
Of the 17 AS patients, 12 were in the IH group and 5 in the non-IH group. Of the 12 in the IH group, 10 required posterior vault expansion, 1 spring-assisted cranioplasty, and 1 fronto-orbital advancement. Of the 12 in the IH group, 12 (100%) had lacunae with a mean LCP of 3% (range 1–20%). In the 5 of the non-IH group, 5 (100%) had lacunae with a mean LCP of 3% (range 1–8%). There was no significant difference between groups (p = 0.9) (Fig. 5).
Discussion
This study found no significant difference in lacunae-cranial proportion (LCP) between syndromic craniosynostosis children with intracranial hypertension (IH) and those where this was not present. This finding is broadly in line with previously published studies which suggest that the presence or absence of copper beating on plain radiography is not a useful indicator of the presence or absence of IH [3, 5, 6, 10]. This suggests that even the addition of quantitative 3D analysis does not improve radiological prediction of IH when compared to traditional quantitative assessment of plain radiographs.
This lack of correlation between LCP and IH also existed on subgroup analysis, when groups were stratified by individual cranial bone, or by syndrome (AS or CS). Posterior bones—parietal and occipital—were more affected in general than the frontal bones, but their LCP was no more predictive of the presence of IH. Lacunae were ubiquitous in AS (IH and non-IH groups alike), whereas a number of CS patients did not have any lacunae—this was true in both IH and non-IH groups.
Although the overall findings were not significant, it was noticeable that the 2 children (one CS and one AS) with markedly high LCPs (both over double the LCP of the third ranked case) both did have IH. It may be that the presence of very extensive lacunae is a more robust predictor of IH, but the number of cases in the current series was too small to assess this possibility.
In regard to the analysis, we are limited by the relatively small case number (n = 35). This is due to the rarity of syndromic craniosynostosis and is common across studies in this group [12]. We selected syndromic craniosynostosis as the study group as the risk of IH is much higher than in single-suture patients, and because clear radiological detection of IH would be very useful for management in CS and AS, for which we currently rely on a combination of clinical, ophthalmic, and radiological factors [1, 2]. A similar study using 3DR would be interesting in single-suture synostosis; however, our unit (in keeping with practice with many of the larger craniofacial units worldwide) does not routinely undertake CT scanning for single-suture cases in the absence of other concerns [13, 14] which limits the dataset available for analysis. 3D optical imaging, which avoids ionizing radiation, can reliably assess head shape in children with craniosynostosis [15, 16] but does not allow delimitation of cranial lacunae. Another issue is regarding age at index scan, which varied considerably in our study group. This was predominantly due to late presentation in the Crouzon group, which can be phenotypically mild and not be diagnosed early in infancy [17, 18]. Calvarial bone thickens with age [19] and this may influence the sensitivity of LCP.
3DR allows accurate calculation of LCP in children with craniosynostosis. This study, in agreement to studies that have looked at quantitative copper beating, did not find a relationship between the degree of LCP and IH. However, the 3DR technique may be useful for further studies in this patient group.
References
Abu-Sittah GS, Jeelani O, Dunaway D, Hayward R (2016) Raised intracranial pressure in Crouzon syndrome: incidence, causes, and management. J Neurosurg Pediatr 17:469–475. https://doi.org/10.3171/2015.6.PEDS15177
Marucci DD, Dunaway DJ, Jones BM, Hayward RD (2008) Raised intracranial pressure in Apert syndrome. Plast Reconstr Surg 122:1162–1168. https://doi.org/10.1097/PRS.0b013e31818458f0
Tamburrini G, Caldarelli M, Massimi L, Gasparini G, Pelo S, di Rocco C (2012) Complex craniosynostoses: a review of the prominent clinical features and the related management strategies. Childs Nerv Syst 28:1511–1523. https://doi.org/10.1007/s00381-012-1819-4
Ma R, Rowland D, Judge A et al (2018) Complications following intracranial pressure monitoring in children: a 6-year single-center experience. J Neurosurg Pediatr:1–6. https://doi.org/10.3171/2017.9.PEDS17360
Tamburrini G, Caldarelli M, Massimi L, Santini P, di Rocco C (2005) Intracranial pressure monitoring in children with single suture and complex craniosynostosis: a review. Childs Nerv Syst 21:913–921. https://doi.org/10.1007/s00381-004-1117-x
Tuite GF, Chong WK, Evanson J, Narita A, Taylor D, Harkness WF, Jones BM, Hayward RD (1996) The effectiveness of papilledema as an indicator of raised intracranial pressure in children with craniosynostosis. Neurosurgery 38:272–278
Liasis A, Nischal KK, Walters B, Thompson D, Hardy S, Towell A, Dunaway D, Jones B, Evans R, Hayward R (2006) Monitoring visual function in children with syndromic craniosynostosis: a comparison of 3 methods. Arch Ophthalmol 124:1119–1126
Swanson J, Xu W, Aleman T, Mitchell B, Wes A, Chen SS, Bender L, Heuer G, Katowitz W, Bartlett S, Taylor J (2015) Optical coherence tomography can detect intracranial hypertension in young children with craniosynostosis. Plast Reconstr Surg 136:39
Driessen C, van Veelen M-LC, Lequin M, Joosten KFM, Mathijssen IMJ (2012) Nocturnal ultrasound measurements of optic nerve sheath diameter correlate with intracranial pressure in children with craniosynostosis. Plast Reconstr Surg 130:448e–451e
Tuite GF, Evanson J, Chong WK, Thompson DNP, Harkness WF, Jones BM, Hayward RD (1996) The beaten copper cranium: a correlation between intracranial pressure, cranial radiographs, and computed tomographic scans in children with craniosynostosis. Neurosurgery 39:691–699
Liasis A, Thompson DA, Hayward R, Nischal KK (2003) Sustained raised intracranial pressure implicated only by pattern reversal visual evoked potentials after cranial vault expansion surgery. Pediatr Neurosurg 39:75–80. https://doi.org/10.1159/000071318
Boulet SL, Rasmussen SA, Honein MA (2008) A population-based study of craniosynostosis in metropolitan Atlanta, 1989-2003. Am J Med Genet A 146A:984–991. https://doi.org/10.1002/ajmg.a.32208
Cerovac S, Neil-Dwyer JG, Rich P, Jones BM, Hayward RD (2009) Are routine preoperative CT scans necessary in the management of single suture craniosynostosis? Br J Neurosurg 16:348–354. https://doi.org/10.1080/0268869021000007560
Schweitzer T, Bohm H, Meyer-Marcotty P et al (2012) Avoiding CT scans in children with single-suture craniosynostosis. Childs Nerv Syst 28:1077–1082. https://doi.org/10.1007/s00381-012-1721-0
Rodriguez-Florez N, Goktekin OK, Bruse JL et al (2017) Quantifying the effect of corrective surgery for trigonocephaly: a non-invasive, non-ionizing method using three-dimensional handheld scanning and statistical shape modelling. J Cranio-Maxillofac Surg 45:387–394. https://doi.org/10.1016/j.jcms.2017.01.002
Tenhagen M, Bruse JL, Rodriguez-Florez N, Angullia F, Borghi A, Koudstaal MJ, Schievano S, Jeelani O, Dunaway D (2016) Three-dimensional handheld scanning to quantify head-shape changes in spring-assisted surgery for sagittal craniosynostosis. Journal of Craniofacial Surgery 27:2117–2123
Wood BC, Oh AK, Keating RF, Boyajian MJ, Myseros JS, Magge SN, Rogers GF (2015) Progressive postnatal pansynostosis: an insidious and pernicious form of craniosynostosis. J Neurosurg Pediatr 16:309–316. https://doi.org/10.3171/2015.1.PEDS14464
Rogers GF, Greene AK, Proctor MR, Mulliken JB, Goobie SM, Stoler JM (2015) Progressive postnatal pansynostosis. The Cleft Palate-Craniofacial Journal 52:751–757. https://doi.org/10.1597/14-092
Delye H, Clijmans T, Mommaerts MY, Sloten JV, Goffin J (2015) Creating a normative database of age-specific 3D geometrical data, bone density, and bone thickness of the developing skull: a pilot study. J Neurosurg Pediatr 16:687–702. https://doi.org/10.3171/2015.4.PEDS1493
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No financial or material supports were received for the work undertaken in this paper. None of the authors have any conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mondal, A., Rodriguez-Florez, N., O’Hara, J. et al. Lack of association of cranial lacunae with intracranial hypertension in children with Crouzon syndrome and Apert syndrome: a 3D morphometric quantitative analysis. Childs Nerv Syst 35, 501–507 (2019). https://doi.org/10.1007/s00381-019-04059-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04059-6