Abstract
Introduction
Phase II monitoring with intracranial electroencephalography (ICEEG) occasionally requires bilateral placement of subdural (SD) strips, grids, and/or depth electrodes. While phase I monitoring often demonstrates a preponderance of unilateral findings, individual studies (video EEG, single photon emission computed tomography [SPECT], and positron emission tomography [PET]) can suggest or fail to exclude a contralateral epileptogenic onset zone. This study describes previously unreported techniques of trans-falcine and sub-frontal insertion of contralateral SD grids and depth electrodes for phase II monitoring in pediatric epilepsy surgery patients when concern about bilateral abnormalities has been elicited during phase I monitoring.
Methods
Pediatric patients with medically refractory epilepsy undergoing stage I surgery for phase II monitoring involving sub-frontal and/or trans-falcine insertion of SD grids and/or depth electrodes at the senior author’s institution were retrospectively reviewed. Intra-operative technical details of sub-frontal and trans-falcine approaches were studied, while intra-operative complications or events were noted. Operative techniques included gentle subfrontal retraction and elevation of the olfactory tracts (while preserving the relationship between the olfactory bulb and cribriform plate) to insert SD grids across the midline for coverage of the contralateral orbito-frontal regions. Trans-falcine approaches involved accessing the inter-hemispheric space, bipolar cauterization of the anterior falx cerebri below the superior sagittal sinus, and sharp dissection using a blunt elevator and small blade scalpel. The falcine window allowed contralateral SD strip, grid, and depth electrodes to be inserted for coverage of the contralateral frontal regions.
Results
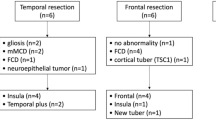
The study cohort included seven patients undergoing sub-frontal and/or trans-falcine insertion of contralateral SD strip, grid, and/or depth electrodes from February 2012 through June 2015. Five patients (71%) experienced no intra-operative events related to contralateral ICEEG electrode insertion. Intra-operative events of frontal territory venous engorgement (1/7, 14%) due to sacrifice of anterior bridging veins draining into the SSS and avulsion of a contralateral bridging vein (1/7, 14%), probably due to prior anterior corpus callosotomy, each occurred in one patient. There were no intra-operative or peri-operative complications in any of the patients studied. Two patients required additional surgery for supplemental SD strip and/or depth electrodes via burr hole craniectomy to enhance phase II monitoring. All patients proceeded to stage II surgery for resection of ipsilateral epileptogenic onset zones without adverse events.
Conclusions
Trans-falcine and sub-frontal insertion of contralateral SD strip, grid, and depth electrodes are previously unreported techniques for achieving bilateral frontal coverage in phase II monitoring in pediatric epilepsy surgery. This technique obviates the need for contralateral craniotomy and parenchymal exposure with limited, remediable risks. Larger case series using the method described herein are now necessary.

Similar content being viewed by others
References
Abuelem T, Friedman D, Agadi S, Wilfong AA, Yoshor D (2013) Interhemispheric Subdural Electrodes: Technique, Utility, and Safety. Neurosurgery 73(2 Suppl Operative):ons253–60
Davidson L, McComb GJ (2012) The safety of the intraoperative sacrifice of the deep cerebral veins. Childs Nerv Syst 29:199–207
Elsharkawy AE, May T, Thorbecke R, Ebner A (2009) Predictors of quality of life after resective extratemporal epilepsy surgery in adults in long-term follow-up. Seizure 18:498–503
Engel J (1996) Surgery for seizures. New Eng J Med 334:647–652
Goel A (1995) Transfalcine approach to a contralateral hemispheric tumour. Acta Neurochir 135:210–212
Janszky J, Jokeit H, Schulz R, Hoppe M, Ebner A (2000) EEG predicts surgical outcome in lesional frontal lobe epilepsy. Neurology 54:1470–1476
Jobst BC, Siegel AM, Thadani VM, Roberts DW, Rhodes HC, Williamson PD (2000) Intractable seizures of frontal lobe origin: clinical characteristics, localizing signs, and results of surgery. Epilepsia 41:1139–1152
Kazemi NJ, So EL, Mosewich RK, O’Brien TJ, Cascino GD, Trenerry MR et al (1997) Resection of frontal encephalomalacias for intractable epilepsy: outcome and prognostic factors. Epilepsia 38:670–677
Kral T, Kuczaty S, Blümcke I, Urbach H, Clusmann H, Wiestler OD et al (2001) Postsurgical outcome of children and adolescents with medically refractory frontal lobe epilepsies. Childs Nerv Syst 17:595–601
Lawton MT, Golfinos JG, Spetzler RF (1996) The contralateral transcallosal approach: experience with 32 patients. Neurosurgery 39:729
Lazow SP, Thadani VM, Gilbert KL, Morse RP, Bujarski KA, Kulandaivel K et al (2012) Outcome of frontal lobe epilepsy surgery. Epilepsia 53:1746–1755
Lee JJ, Lee SK, Lee S-YY, Park K-II, Kim DW, Lee DS et al (2008) Frontal lobe epilepsy: clinical characteristics, surgical outcomes and diagnostic modalities. Seizure 17:514–523
Machado de Almeida G, Shibata MK, Nakagawa EJ (1984) Contralateral parafalcine approach for parasagittal and callosal arteriovenous malformations. Neurosurgery 14:744–746
Malekpour M, Cohen-Gadol AA (2015) Interhemispheric transfalcine approach and awake cortical mapping for resection of peri-atrial gliomas associated with the central lobule. J Clin Neurosci 22:383–386
McNatt SA, Sosa IJ, Krieger MD, McComb JG (2011) Incidence of venous infarction after sacrificing middle-third superior sagittal sinus cortical bridging veins in a pediatric population. J Neurosurg Pediatr 7:224–228
Mortazavi MM, Denning M, Yalcin B, Shoja MM, Loukas M, Tubbs SR (2013) The intracranial bridging veins: a comprehensive review of their history, anatomy, histology, pathology, and neurosurgical implications. Childs Nerv Syst 29:1073–1078
Placantonakis DG, Shariff S, Lafaille F, Labar D, Harden C, Hosain S et al (2010) Bilateral intracranial electrodes for lateralizing intractable epilepsy: efficacy, risk, and outcome. Neurosurgery 66:274–283
Siegel AM, Jobst BC, Thadani VM, Rhodes CH, Lewis PJ, Roberts DW et al (2001) Medically intractable, localization-related epilepsy with normal MRI: presurgical evaluation and surgical outcome in 43 patients. Epilepsia 42:883–888
Sperling MR (1997) Clinical challenges in invasive monitoring in epilepsy surgery. Epilepsia 38(Suppl 4):12
Yun C-HH, Lee SK, Lee SY, Kim KK, Jeong SW, Chung C-KK (2006) Prognostic factors in neocortical epilepsy surgery: multivariate analysis. Epilepsia 47:574–579
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study received Institutional Review Board (IRB) approval at the senior author’s institution and abided by all applicable IRB regulations and guidelines.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings described in this paper. There were no sources of financial or material support for this work.
Rights and permissions
About this article
Cite this article
Pindrik, J., Hoang, N., Tubbs, R.S. et al. Trans-falcine and contralateral sub-frontal electrode placement in pediatric epilepsy surgery: technical note. Childs Nerv Syst 33, 1379–1388 (2017). https://doi.org/10.1007/s00381-017-3469-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3469-z