Abstract
Background
Despite the recent advent of various radiographic imaging techniques, it is still very difficult to correctly distinguish a pediatric osteolytic lesion in the occipital condyle, which makes it further complicated to decide on the necessity of and the adequate timing for radical resection and craniocervical fusions. To establish a legitimate therapeutic strategy for this deep-seated lesion, surgical biopsy is a reasonable choice for first-line intervention. The choice of surgical approach becomes very important because a sufficient amount of histological specimen must be obtained to confirm the diagnosis but, ideally, the residual bony structures and the muscular structures should be preserved so as not to increase craniocervical instability. In this report, we present our experience with a case of solitary Langerhans cell histiocytosis (LCH) involving the occipital condyle that was successfully treated with minimally invasive surgical biopsy with a far lateral condylar approach supported by preoperative 3D computer graphic simulation.
Case report
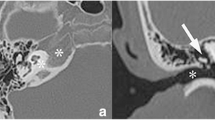
An 8-year-old girl presented with neck pain. Magnetic resonance imaging and computed tomography (CT) revealed an osteolytic lesion of the left occipital condyle. At surgery, the patient was placed in the prone position. A 3-cm skin incision was made in the posterior auricular region, and the sternocleidomastoid and splenius capitis muscles were dissected in the middle of the muscle bundle along the direction of the muscle fiber. Under a navigation system, we approached the occipital condyle through the space between the longissimus capitis muscle and the posterior belly of the digastric muscle and lateral to the superior oblique muscle, verifying each muscle at each depth of the surgical field and, finally, obtained sufficient surgical specimen. After the biopsy, her craniocervical instability had not worsened, and chemotherapy was performed. Twelve weeks after chemotherapy, her neck pain had gradually disappeared along with her torticollis, and CT showed remission of the lesion and marked regeneration of the left occipital condyle. Within our knowledge, this is the first reported case of LCH involving the occipital condyle. Although very rare, our case indicated that LCH can be an alternative in the differential diagnosis of osteolytic lesions in the craniocervical junction, in which early bone regeneration with sufficient cervical stability is expected after chemotherapy.
Conclusions
In cases of pediatric osteolytic lesions, when they initially presented with apparent cervical instability, craniocervical fusion may possibly become unnecessary after a series of treatments. Thus, the effort to maximally preserve the musculoskeletal structure should be made until its histological diagnosis is finally confirmed.




Similar content being viewed by others
References
D’Ambrosio N, Soohoo S, Warshall C, Johnson A, Karimi S (2008) Craniofacial and intracranial manifestations of Langerhans cell histiocytosis: report of findings in 100 patients. AJR Am J Roentgenol 191:589–597
Hurley ME, O’Meara A, Fogarty E, Hayes R (2004) Langerhans’ cell histiocytosis of the clivus case report and literature review. Pediatr Radiol 34:267–270
Krishna H, O’Meara A, Fagarty E, Hayes R (2004) Langerhans cell histiocytosis of the clivus and sphenoid sinus with parasellar and petrous extensions: case report and review of literature. Surg Neurol 62:447–454
Lee SK, Jung TY, Jung S, Han DK, Lee JK, Baek HJ (2013) Solitary Langerhans cell histiocytosis of skull and spine in pediatric and adult patients. Childs Nerv Syst.
Lederman CR, Lederman ME (1998) Unifocal Langerhans’ cell histiocytosis in the clivus of a child with abducens palsy and diplopia. J AAPOS 2:378–379
Thomas C, Donnadieu J, Emile JF, Brousse N (1996) Langerhans cell histiocytosis. Arch Pediatr 3:63–69
Azouz EM, Saigal G, Rodriguez MM, Podda A (2005) Langerhans’ cell histiocytosis: pathology, imaging and treatment of skeletal involvement. Pediatr Radiol 35:103–115
Beschorner R, Koerbel A, Schittenhelm J, Kaminsky J, Loewenheim H, Bueltmann E et al (2008) 47-year-old woman with a clival mass. Brain Pathol 18:100–102
Binning MJ, Brockmeyer DL (2008) Novel multidisciplinary approach for treatment of Langerhans cell histiocytosis of the skull base. Skull Base 18:53–58
Boston M, Derkay CS (2002) Langerhans’ cell histiocytosis of the temporal bone and skull base. Am J Otolaryngol 23:246–248
Brisman JL, Feldstein NA, Tarbell NJ, Cohen D, Cargan AL, Haddad J Jr et al (1997) Eosinophilic granuloma of the clivus: case report, follow-up of two previously reported cases, and review of the literature on cranial base eosinophilic granuloma. Neurosurgery 41:273–278
Kilborn TN, The J, Goodman TR (2003) Paediatric manifestations of Langerhans cell histiocytosis: a review of the clinical and radiological findings. Clin Radiol 58:269–278
Menezes AH (2012) Craniocervical fusions in children. J Neurosurg Pediatr 9:573–585
Ahmed M, Sureka J, Koshy CG, Chacko BR, Chacko G (2012) Langerhans cell histiocytosis of the clivus: an unusual cause of a destructive central skull base mass in a child. Neurol India 60:346–348
Rosenfeld JV, Wallace D, Klug GL, Danks A (1992) Transnasal stereotactic biopsy of a clivus tumor: technical note. J Neurosurg 76:878–879
Sampson JH, Rossitch E Jr, Young JN, Lane KL, Friedman AH (1992) Solitary eosinophilic granuloma invading the clivus of an adult: case report. Neurosurgery 31:755–757
Mut CO, Bakar B, Cila A, Akalan N (2004) Eosinophilic granuloma of the skull associated with epidural haematoma: a case report and review of the literature. Childs Nerv Syst 20:765–769
Okamoto K, Ito J, Furusawa T, Sakai K, Tokiguchi S (1999) Imaging of calvarial eosinophil granuloma. Neuroradiology 41:723–728
Mosiewicz A, Rola R, Jarosz B, Trojanowska A, Trojanowski T (2010) Langerhans cell histiocytosis of the parietal bone with epidural and extracranial expansion—case report and a review of the literature. Neurol Neurochir Pol 44:196–203
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used or the findings specified in this paper.
Author contributions
Y. Teranishi provided conception and design, surgical treatment, postoperative patient, management, acquisition of data, and drafting of the article.
M. Shin provided conception and design, surgical treatment, drafting of the article, and critical revision of the article.
M. Yoshino performed surgical planning, technical support in surgery, and preparation of figures.
N. Saito provided the critical revision of the article, organization of the treatment team, and supervision of the overall treatment project.
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors have reviewed and approved the final version of this manuscript.
Rights and permissions
About this article
Cite this article
Teranishi, Y., Shin, M., Yoshino, M. et al. Solitary Langerhans cell histiocytosis of the occipital condyle: a case report and review of the literature. Childs Nerv Syst 32, 399–404 (2016). https://doi.org/10.1007/s00381-015-2850-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2850-z