Abstract
Background and importance
The decompressive hemicraniectomy (DCH) after malignant middle cerebral artery infarction in children is a rare procedure, and the indication is discussed as being controversial. Etiological Moyamoya disease has some additional challenges concerning the therapeutic strategy that have not mentioned in the recent literature, as it is dependent on special pathophysiology.
Clinical presentation
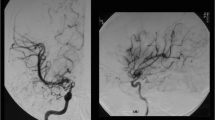
We report a case of a four-year-old patient with a decompressive hemicraniectomy after malignant middle cerebral artery infarction on the right hemisphere based on a Moyamoya syndrome with proximal MCA occlusions on both sides. After the decompression there was a good restitution of the hemiparesis, aphasia, and consciousness loss on admission. The bone flap replacement is usually done after three month in our department to ensure brain swelling has subsided. In this patient the cranioplasty was not arranged because of the development of collateral vessels to the right motor region through the craniotomy defect, to protect the supply of the eloquent cortex.
Conclusion
We conclude that the indication of DCH and postoperative treatment should be discussed individually, especially when neovascularisation developments can occur like in Moyamoya disease. An important point is the right timing for bone flap replacement, which should be directly after cerebral edema has subsided prior to the evolution of collaterals through the craniotomy defect. Additionally, leaving the opportunity for neovascularization through smaller defects has to be taken into account.




Similar content being viewed by others
References
Fullerton HJ, Wu YW, Sidney S, Johnston SC (2007) Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerebrovascular imaging. Pediatrics 119(3):495–501. doi:10.1542/peds.2006-2791
Agrawal N, Johnston SC, Wu YW, Sidney S, Fullerton HJ (2009) Imaging data reveal a higher pediatric stroke incidence than prior US estimates. Stroke J Cereb Circ 40(11):3415–3421. doi:10.1161/STROKEAHA.109.564633
Sträter R, Kurnik K, Heller C, Schobess R, Luigs P, Nowak-Göttl U (2001) Aspirin versus low-dose low-molecular-weight heparin: antithrombotic therapy in pediatric ischemic stroke patients: a prospective follow-up study. Stroke J Cereb Circ 32(11):2554–2558
Giroud M, Lemesle M, Gouyon JB, Nivelon JL, Milan C, Dumas R (1995) Cerebrovascular disease in children under 16 years of age in the city of Dijon, France: a study of incidence and clinical features from 1985 to 1993. J Clin Epidemiol 48(11):1343–1348
Schoenberg BS, Mellinger JF, Schoenberg DG (1978) Cerebrovascular disease in infants and children: a study of incidence, clinical features, and survival. Neurology 28(8):763–768
Mackay MT, Wiznitzer M, Benedict SL et al (2011) Arterial ischemic stroke risk factors: the International Pediatric Stroke Study. Ann Neurol 69(1):130–140. doi:10.1002/ana.22224
Hofmeijer J, van der Worp HB, Kappelle LJ (2003) Treatment of space-occupying cerebral infarction. Crit Care Med 31(2):617–625. doi:10.1097/01.CCM.0000050446.16158.80
Vahedi K, Hofmeijer J, Juettler E et al (2007) Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol 6(3):215–222. doi:10.1016/S1474-4422(07)70036-4
Ramaswamy V, Mehta V, Bauman M, Richer L, Massicotte P, Yager JY (2008) Decompressive hemicraniectomy in children with severe ischemic stroke and life-threatening cerebral edema. J Child Neurol 23(8):889–894. doi:10.1177/0883073808314960
Smith SE, Kirkham FJ, Deveber G et al (2011) Outcome following decompressive craniectomy for malignant middle cerebral artery infarction in children. Dev Med Child Neurol 53(1):29–33. doi:10.1111/j.1469-8749.2010.03775.x
Omay SB, Carrión-Grant GM, Kuzmik GA et al (2013) Decompressive hemicraniectomy for ischemic stroke in the pediatric population. Neurosurg Rev 36(1):21–24. doi:10.1007/s10143-012-0411-4, discussion 24–25
Shah S, Murthy SB, Whitehead WE, Jea A, Nassif LM (2013) Decompressive hemicraniectomy in pediatric patients with malignant middle cerebral artery infarction: case series and review of the literature. World Neurosurg 80(1–2):126–133. doi:10.1016/j.wneu.2013.06.001
Vahedi K, Vicaut E, Mateo J et al (2007) Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke J Cereb Circ 38(9):2506–2517. doi:10.1161/STROKEAHA.107.485235
Takeuchi K, Shimizu K (1957) Hypoplasia of the bilateral internal carotid arteries. Brain Nerve 9:37–43
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20(3):288–299
Kuriyama S, Kusaka Y, Fujimura M et al (2008) Prevalence and clinicoepidemiological features of moyamoya disease in Japan: findings from a nationwide epidemiological survey. Stroke J Cereb Circ 39(1):42–47. doi:10.1161/STROKEAHA.107.490714
Baba T, Houkin K, Kuroda S (2008) Novel epidemiological features of moyamoya disease. J Neurol Neurosurg Psychiatry 79(8):900–904. doi:10.1136/jnnp.2007.130666
Uchino K, Johnston SC, Becker KJ, Tirschwell DL (2005) Moyamoya disease in Washington State and California. Neurology 65(6):956–958. doi:10.1212/01.wnl.0000176066.33797.82
Smith ER, Scott RM (2012) Spontaneous occlusion of the circle of Willis in children: pediatric moyamoya summary with proposed evidence-based practice guidelines. A review. J Neurosurg Pediatr 9(4):353–360. doi:10.3171/2011.12.PEDS1172
Smith JL (2009) Understanding and treating moyamoya disease in children. Neurosurg Focus 26(4), E4. doi:10.3171/2000.01.FOCUS08306
Yamashita M, Oka K, Tanaka K (1983) Histopathology of the brain vascular network in moyamoya disease. Stroke J Cereb Circ 14(1):50–58
Achrol AS, Guzman R, Lee M, Steinberg GK (2009) Pathophysiology and genetic factors in moyamoya disease. Neurosurg Focus 26(4), E4. doi:10.3171/2009.1.FOCUS08302
Yadla S, Campbell PG, Chitale R, Maltenfort MG, Jabbour P, Sharan AD (2011) Effect of early surgery, material, and method of flap preservation on cranioplasty infections: a systematic review. Neurosurgery 68(4):1124–1129. doi:10.1227/NEU.0b013e31820a5470, discussion 1130
Beauchamp KM, Kashuk J, Moore EE et al (2010) Cranioplasty after postinjury decompressive craniectomy: is timing of the essence? J Trauma 69(2):270–274. doi:10.1097/TA.0b013e3181e491c2
Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D (2010) Outcomes of cranial repair after craniectomy. J Neurosurg 112(5):1120–1124. doi:10.3171/2009.6.JNS09133
Archavlis E, Carvi Y, Nievas M (2012) The impact of timing of cranioplasty in patients with large cranial defects after decompressive hemicraniectomy. Acta Neurochir (Wien) 154(6):1055–1062. doi:10.1007/s00701-012-1333-1
Schuss P, Vatter H, Marquardt G et al (2012) Cranioplasty after decompressive craniectomy: the effect of timing on postoperative complications. J Neurotrauma 29(6):1090–1095. doi:10.1089/neu.2011.2176
Schuss P, Vatter H, Oszvald A et al (2013) Bone flap resorption: risk factors for the development of a long-term complication following cranioplasty after decompressive craniectomy. J Neurotrauma 30(2):91–95. doi:10.1089/neu.2012.2542
Author information
Authors and Affiliations
Corresponding author
Additional information
There are no financial affiliations for each of the authors.
Rights and permissions
About this article
Cite this article
Hohenhaus, M., Shah, M.J., Eckenweiler, M. et al. Decompressive hemicraniectomy in the management of acute stroke in children with Moyamoya disease: the difficult balance between the spontaneous postoperative revascularization process and the need for cranial reconstruction. Childs Nerv Syst 31, 2369–2373 (2015). https://doi.org/10.1007/s00381-015-2802-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2802-7