Abstract
Purpose
Pinealoblastoma is a highly malignant embryonal tumour of the pineal region affecting children and young adults. We herein intend to report the clinical features and treatment outcome of patients of pinealoblastoma treated at our institute.
Methods
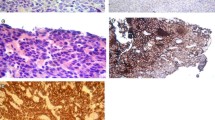
Clinical data was collected by retrospective chart review from 2003–2012. Histopathology slides were reviewed, and relevant immunohistochemistry stains were done. Overall survival (OS) and recurrence-free survival (RFS) were analysed by Kaplan-Meier product-limit method. Univariate and multivariate analyses of prognostic factors were done by log rank test and Cox proportional hazard regression model, respectively.
Results
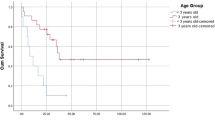
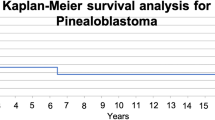
Seventeen patients met the study criterion (male:female = 11:6). Median age at presentation was 14 years (range 4–47 years). Surgical resection was gross total in 6 (35.29 %), near-total in 2 (11.76 %), sub-total in 2 (11.76 %), and limited to biopsy in 7 (41.18 %) patients. At presentation, 4 patients had leptomeningeal dissemination. Radiation therapy was delivered in all patients—craniospinal irradiation in 15 (88.24 %), whole brain irradiation in 1 (5.88 %), and whole ventricular irradiation followed by boost in 1 (5.88 %) patient. Systemic chemotherapy (median 6 cycles) was given in 14 (82.35 %) patients. The most common regimen was a combination of carboplatin and etoposide, used in 10 (58.82 %) patients. After a median follow-up of 30.3 months (mean 32.01 months), death and disease recurrences were noted in 3 (17.65 %) and 7 (41.18 %) patients. Amongst the patients with recurrent disease, 4 had spinal drop metastases and 3 had local recurrence along with spinal drop metastases. Median OS was not reached, and estimated median RFS was noted to be 5.49 years. The actuarial rates of OS and RFS at 2 years were 85.6 and 73.1 %, respectively. On univariate analysis, age more than 8 years (P = 0.0071) and M0 stage (P = 0.0483) were significant predictors of improved RFS. Age retained significance on multivariate analysis of RFS (P = 0.02932).
Conclusion
Maximal safe resection followed by craniospinal irradiation and systemic chemotherapy with 6 cycles of carboplatin-etoposide regimen is a reasonable treatment strategy in patients of pinealoblastoma more than 8 years of age in a developing nation. However, the same strategy is less effective in younger children and innovative study designs of intensification of post-operative treatment must be explored in this age group.







Similar content being viewed by others
References
Fauchon F, Jouvet A, Paquis P, Saint-Pierre G, Mottolese C, Ben Hassel M, Chauveinc L, Sichez JP, Philippon J, Schlienger M, Bouffet E (2000) Parenchymal pineal tumors: a clinicopathological study of 76 cases. Int J Radiat Oncol Biol Phys 46:959–968
Nakazato Y, Jouvet A, Scheithauer BW (2007) Tumours of the pineal region. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) WHO classification of tumours of the central nervous system, 4th edn. International Agency for Research on Cancer, Lyon, pp 121–129
Villá S (2012) Primary pineal tumors: outcome and prognostic factors—a study from the Rare Cancer Network (RCN). Clin Transl Oncol 14:827–834
Macdonald D, Cascino T, Schold SJ, Cairncross J (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8:1277–1280
Hart MN, Earle KM (1973) Primitive neuroectodermal tumors of the brain in children. Cancer 32:890–897
Chintagumpala M, Hassall T, Palmer S, Ashley D, Wallace D, Kasow K, Merchant TE, Krasin MJ, Dauser R, Boop F, Krance R, Woo S, Cheuk R, Lau C, Gilbertson R, Gajjar A (2009) A pilot study of risk-adapted radiotherapy and chemotherapy in patients with supratentorial PNET. Neurooncol 11:33–40
Gaffney CC, Sloane JP, Bradley NJ, Bloom HJ (1985) Primitive neuroectodermal tumours of the cerebrum. Pathology and treatment. J Neurooncol 3:23–33
Massimino M, Gandola L, Spreafico F, Luksch R, Collini P, Giangaspero F, Simonetti F, Casanova M, Cefalo G, Pignoli E, Ferrari A, Terenziani M, Podda M, Meazza C, Polastri D, Poggi G, Ravagnani F, Fossati-Bellani F (2006) Supratentorial primitive neuroectodermal tumors (SPNET) in children: a prospective experience with adjuvant intensive chemotherapy and hyperfractionated accelerated radiotherapy. Int J Radiat Oncol Biol Phys 64:1031–1037
Inda MM, Perot C, Guillaud-Bataille M, Danglot G, Rey JA, Bello MJ, Fan X, Eberhart C, Zazpe I, Portillo E, Tuñón T, Martínez-Peñuela JM, Bernheim A, Castresana JS (2005) Genetic heterogeneity in supratentorial and infratentorial primitive neuroectodermal tumours of the central nervous system. Histopathology 47:631–637
Pfister S, Remke M, Toedt G, Werft W, Benner A, Mendrzyk F, Wittmann A, Devens F, von Hoff K, Rutkowski S, Kulozik A, Radlwimmer B, Scheurlen W, Lichter P, Korshunov A (2007) Supratentorial primitive neuroectodermal tumors of the central nervous system frequently harbor deletions of the CDKN2A locus and other genomic aberrations distinct from medulloblastomas. Genes Chromosomes Cancer 46:839–851
Rorke LB (1983) The cerebellar medulloblastoma and its relationship to primitive neuroectodermal tumors. J Neuropathol Exp Neurol 42:1–15
Russo C, Pellarin M, Tingby O, Bollen AW, Lamborn KR, Mohapatra G, Collins VP, Feuerstein BG (1999) Comparative genomic hybridization in patients with supratentorial and infratentorial primitive neuroectodermal tumors. Cancer 86:331–339
Picard D, Miller S, Hawkins CE, Bouffet E, Rogers HA, Chan TS, Kim SK, Ra YS, Fangusaro J, Korshunov A, Toledano H, Nakamura H, Hayden JT, Chan J, Lafay-Cousin L, Hu P, Fan X, Muraszko KM, Pomeroy SL, Lau CC, Ng HK, Jones C, Van Meter T, Clifford SC, Eberhart C, Gajjar A, Pfister SM, Grundy RG, Huang A (2012) Markers of survival and metastatic potential in childhood CNS primitive neuro-ectodermal brain tumours: an integrative genomic analysis. Lancet Oncol 13:838–848
Fangusaro J, Finlay J, Sposto R, Ji L, Saly M, Zacharoulis S, Asgharzadeh S, Abromowitch M, Olshefski R, Halpern S, Dubowy R, Comito M, Diez B, Kellie S, Hukin J, Rosenblum M, Dunkel I, Miller DC, Allen J, Gardner S (2008) Intensive chemotherapy followed by consolidative myeloablative chemotherapy with autologous hematopoietic cell rescue (AuHCR) in young children with newly diagnosed supratentorial primitive neuroectodermal tumors (sPNETs): report of the Head Start I and II experience. Pediatr Blood Cancer 50:312–8
Reddy AT, Janss AJ, Phillips PC, Weiss HL, Packer RJ (2000) Outcome for children with supratentorial primitive neuroectodermal tumors treated with surgery, radiation and chemotherapy. Cancer 88:2189–2193
Dirks PB, Harris L, Hoffman HJ, Humphreys RP, Drake JM, Rutka JT (1996) Supratentorial primitive neuroectodermal tumors in children. J Neurooncol 29:75–84
McBride SM, Daganzo SM, Banerjee A, Gupta N, Lamborn KR, Prados MD, Berger MS, Wara WM, Haas-Kogan DA (2008) Radiation is an important component of multimodality therapy for pediatric non-pineal supratentorial primitive neuroectodermal tumors. Int J Radiat Oncol Biol Phys 72:1319–23
Paulino AC, Cha DT, Barker JL Jr, Lo S, Manera RB (2004) Patterns of failure in relation to radiotherapy fields in supratentorial primitive neuroectodermal tumor. Int J Radiat Oncol Biol Phys 58:1171–1176
Tomita T (1998) Neurosurgical perspectives in pediatric neurooncology. Childs NervSyst 14:94–96
Cohen BH, Zeltzer PM, Boyett JM, Geyer JR, Allen JC, Finlay JL, McGuire-Cullen P, Milstein JM, Rorke LB, Stanley P et al (1995) Prognostic factors and treatment results for supratentorial primitive neuroectodermaltumors in children using radiation and chemotherapy: a Childrens Cancer Group randomized trial. J Clin Oncol 13:1687–1696
Albright AL, Wisoff JH, Zeltzer P, Boyett J, Rorke LB, Stanley P, Geyer JR, Milstein JM (1995) Prognostic factors in children with supratentorial (nonpineal) primitive neuroectodermal tumors. A neurosurgical perspective from the Children’s Cancer Group. Pediatr Neurosurg 22:1–7
Jakacki R, Zeltzer PM, Boyett JM, Albright AL, Allen JC, Geyer JR, Rorke LB, Stanley P, Stevens KR, Wisoff J et al (1995) Survival and prognostic factors following radiation and/or chemotherapy for primitive neuroectodermal tumors of the pineal region in infants and children: a report of the Children’s Cancer Group. J Clin Oncol 13:1377–1383
Pizer BL, Weston CL, Robinson KJ, Ellison DW, Ironside J, Saran F, Lashford LS, Tait D, Lucraft H, Walker DA, Bailey CC, Taylor RE (2006) Analysis of patients with supratentorial primitive neuro-ectodermal tumors entered into the SIOP/UKCCSG PNET 3 study. Eur J Cancer 42:1120–1128
Duffner PK, Horowitz ME, Krischer JP, Friedman HS, Burger PC, Cohen ME, Sanford RA, Mulhern RK, James HE, Freeman CR et al (1993) Postoperative chemotherapy and delayed radiation in children less than three years of age with malignant brain tumors. N Engl J Med 328:1725–1731
Geyer JR, Zeltzer PM, Boyett JM, Rorke LB, Stanley P, Albright AL, Wisoff JH, Milstein JM, Allen JC, Finlay JL et al (1994) Survival of infants with primitive neuroectodermal tumors or malignant ependymoma of the CNS treated with eight drugs in 1 day: a report from the Childrens Cancer Group. J Clin Oncol 12:1607–1615
Mason WP, Grovas A, Halpern S, Dunkel IJ, Garvin J, Heller G, Rosenblum M, Gardner S, Lyden D, Sands S, Puccetti D, Lindsley K, Merchant TE, O’Malley B, Bayer L, Petriccione MM, Allen J, Finlay JL (1998) Intensive chemotherapy and bone marrow rescue for young children with newly diagnosed malignant brain tumors. J Clin Oncol 16:210–21
Marec-Berard P, Jouvet A, Thiesse P, Kalifa C, Doz F, Frappaz D (2002) Supratentorial embryonal tumors in children under 5 years of age: an SFOP study of treatment with postoperative chemotherapy alone. Med Pediatr Oncol 38:83–90
Geyer JR, Sposto R, Jennings M, Boyett JM, Axtell RA, Breiger D, Broxson E, Donahue B, Finlay JL, Goldwein JW, Heier LA, Johnson D, Mazewski C, Miller DC, Packer R, Puccetti D, Radcliffe J, Tao ML, Shiminski-Maher T, Children’s Cancer Group (2005) Multiagent chemotherapy and deferred radiotherapy in infants with malignant brain tumors: a report from the Children’s Cancer Group. J Clin Oncol 23:7621–31
Timmermann B, Kortmann RD, Kühl J, Rutkowski S, Meisner C, Pietsch T, Deinlein F, Urban C, Warmuth-Metz M, Bamberg M (2006) Role of radiotherapy in supratentorial primitive neuroectodermal tumor in young children: results of the German HIT-SKK87 and HIT-SKK92 trials. J Clin Oncol 24:1554–60
Friedrich C, von Bueren AO, von Hoff K, Gerber NU, Ottensmeier H, Deinlein F, Benesch M, Kwiecien R, Pietsch T, Warmuth-Metz M, Faldum A, Kuehl J, Kortmann RD, Rutkowski S (2013) Treatment of young children with CNS-primitive neuroectodermal tumors/pineoblastomas in the prospective multicenter trial HIT 2000 using different chemotherapy regimens and radiotherapy. Neuro Oncology 15:224–34
Gururangan S, McLaughlin C, Quinn J, Rich J, Reardon D, Halperin EC, Herndon J 2nd, Fuchs H, George T, Provenzale J, Watral M, McLendon RE, Friedman A, Friedman HS, Kurtzberg J, Vredenbergh J, Martin PL (2003) High-dose chemotherapy with autologous stem-cell rescue in children and adults with newly diagnosed pineoblastomas. J Clin Oncol 21:2187–91
Allen J, Donahue B, Mehta M, Miller DC, Rorke LB, Jakacki R, Robertson P, Sposto R, Holmes E, Vezina G, Muraszko K, Puccetti D, Prados M, Chan KW (2009) A phase II study of preradiotherapy chemotherapy followed by hyperfractionated radiotherapy for newly diagnosed high-risk medulloblastoma/primitive neuroectodermal tumor: a report from the Children’s Oncology Group (CCG 9931). Int J Radiat Oncol Biol Phys 74:1006-11
Gerber NU, von Hoff K, Resch A, Ottensmeier H, Kwiecien R, Faldum A, Matuschek C, Hornung D, Bremer M, Benesch M, Pietsch T, Warmuth-Metz M, Kuehl J, Rutkowski S, Kortmann RD (2014) Treatment of children with central nervous system primitive neuroectodermal tumors/pinealoblastomas in the prospective multicentric trial HIT 2000 using hyperfractionated radiation therapy followed by maintenance chemotherapy. Int J Radiat Oncol Biol Phys 89:863–71
Johnston DL, Keene DL, Lafay-Cousin L, Steinbok P, Sung L, Carret AS, Crooks B, Strother D, Wilson B, Odame I, Eisenstat DD, Mpofu C, Zelcer S, Huang A, Bouffet E (2007) Supratentorial primitive neuroectodermal tumors: a Canadian pediatric brain tumor consortium report. J Neuro-Oncol 86:101–108
White L, Johnston H, Jones R, Mameghan H, Nayanar V, McWhirter W, Kellie S, Waters K, Toogood I (1993) Postoperative chemotherapy without radiation in young children with malignant non-astrocytic brain tumours: a report from the Australia and New Zealand Childhood Cancer Study Group (ANZCCSG). Cancer Chemother Pharmacol 32:403–406
Taylor RE, Donachie P, Weston C, Robinson K, Lucraft H, Saran F, Ellison DW, Ironside J, Walker DA, Pizer BL (2009) Impact of radiotherapy parameters on outcome for patients with supratentorial primitive neuro-ectodermal tumours entered into the SIOP/UKCCSG PNET 3 study. Radiother Oncol 92:83–88
Conflict of interest
The authors declare that they have no competing interests.
Source of funding
Nil
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biswas, A., Mallick, S., Purkait, S. et al. Treatment outcome and patterns of failure in patients of pinealoblastoma: review of literature and clinical experience from a regional cancer centre in north India. Childs Nerv Syst 31, 1291–1304 (2015). https://doi.org/10.1007/s00381-015-2751-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2751-1