Abstract
Purpose
The incidence of ventriculoperitoneal (VP) shunt infection accounts for about 5–15 %, but it can rise up to 70 % in specific high-risk subgroups. Antibiotic-impregnated catheters (AICs) have been designed to reduce shunt infections, but reports on their efficacy are discordant, especially in young children. The aim of this study is to assess, for the first time, the efficacy of AICs in newborns and infants at very high risk for shunt infection.
Methods
We reviewed the medical records of newborns and infants treated with a VP shunt for newly diagnosed hydrocephalus. Patients were divided in two groups: Group A was composed by children who received AICs, whereas Group B included children implanted with standard silicone catheters (non-AICs). We compared the shunt infection rate in both groups, and analyzed differences in specific high-risk subgroups (preterm newborns, children with posthemorrhagic or postinfective hydrocephalus, and children with a previous external ventricular drainage).
Results
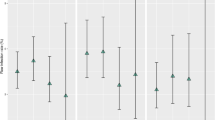
Forty eight children younger than 1 year old were included in our study. Twenty two patients were implanted with an AIC, whereas 26 patients received a standard silicone catheter. The follow-up was at least 1 year (mean 8 ± 3 years). The overall infection rate decreased from 34 % in non-AIC group to 9 % in the AIC group. Moreover, AICs showed to have a protective effect against shunt infections in all the specific high-risk subgroups analyzed.
Conclusions
This study demonstrates for the first time that AICs are effective in reducing VP shunt infection in high-risk pediatric patients younger than 1 year old.






Similar content being viewed by others
References
Chi JH, Fullerton HJ, Gupta N (2005) Time trends and demographics of deaths from congenital hydrocephalus in children in the United States: National Center for Health Statistics data, 1979 to 1998. J Neurosurg 103(2 Suppl):113–118. doi:10.3171/ped.2005.103.2.0113
Vinchon M, Dhellemmes P (2006) Cerebrospinal fluid shunt infection: risk factors and long-term follow-up. Childs Nerv Syst 22(7):692–697. doi:10.1007/s00381-005-0037-8
Walters BC, Hoffman HJ, Hendrick EB, Humphreys RP (1984) Cerebrospinal fluid shunt infection. Influences on initial management and subsequent outcome. J Neurosurg 60(5):1014–1021. doi:10.3171/jns.1984.60.5.1014
Eymann R, Chehab S, Strowitzki M, Steudel WI, Kiefer M (2008) Clinical and economic consequences of antibiotic-impregnated cerebrospinal fluid shunt catheters. J Neurosurg Pediatr 1(6):444–450. doi:10.3171/PED/2008/1/6/444
Choux M, Genitori L, Lang D, Lena G (1992) Shunt implantation: reducing the incidence of shunt infection. J Neurosurg 77(6):875–880. doi:10.3171/jns.1992.77.6.0875
Dallacasa P, Dappozzo A, Galassi E, Sandri F, Cocchi G, Masi M (1995) Cerebrospinal fluid shunt infections in infants. Childs Nerv Syst 11(11):643–648, discussion 649
Gardner P, Leipzig T, Phillips P (1985) Infections of central nervous system shunts. Med Clin North Am 69(2):297–314
Klimo P Jr, Thompson CJ, Ragel BT, Boop FA (2011) Antibiotic-impregnated shunt systems versus standard shunt systems: a meta- and cost-savings analysis. J Neurosurg Pediatr 8(6):600–612. doi:10.3171/2011.8.PEDS11346
Kontny U, Hofling B, Gutjahr P, Voth D, Schwarz M, Schmitt HJ (1993) CSF shunt infections in children. Infection 21(2):89–92
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis: Off Publ Infect Dis Soc Am 36(7):858–862. doi:10.1086/368191
Quigley MR, Reigel DH, Kortyna R (1989) Cerebrospinal fluid shunt infections. Report of 41 cases and a critical review of the literature. Pediatr Neurosci 15(3):111–120
Younger JJ, Simmons JC, Barrett FF (1987) Operative related infection rates for ventriculoperitoneal shunt procedures in a children’s hospital. Infect Control: IC 8(2):67–70
Kulkarni AV, Drake JM, Lamberti-Pasculli M (2001) Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg 94(2):195–201. doi:10.3171/jns.2001.94.2.0195
Pople IK, Bayston R, Hayward RD (1992) Infection of cerebrospinal fluid shunts in infants: a study of etiological factors. J Neurosurg 77(1):29–36. doi:10.3171/jns.1992.77.1.0029
Renier D, Lacombe J, Pierre-Kahn A, Sainte-Rose C, Hirsch JF (1984) Factors causing acute shunt infection. Computer analysis of 1174 operations. J Neurosurg 61(6):1072–1078. doi:10.3171/jns.1984.61.6.1072
Lee JK, Seok JY, Lee JH, Choi EH, Phi JH, Kim SK, Wang KC, Lee HJ (2012) Incidence and risk factors of ventriculoperitoneal shunt infections in children: a study of 333 consecutive shunts in 6 years. J Korean Med Sci 27(12):1563–1568. doi:10.3346/jkms.2012.27.12.1563
Parker SL, Anderson WN, Lilienfeld S, Megerian JT, McGirt MJ (2011) Cerebrospinal shunt infection in patients receiving antibiotic-impregnated versus standard shunts. J Neurosurg Pediatr 8(3):259–265. doi:10.3171/2011.6.PEDS11257
Hayhurst C, Cooke R, Williams D, Kandasamy J, O’Brien DF, Mallucci CL (2008) The impact of antibiotic-impregnated catheters on shunt infection in children and neonates. Childs Nerv Syst 24(5):557–562. doi:10.1007/s00381-007-0521-4
Aryan HE, Meltzer HS, Park MS, Bennett RL, Jandial R, Levy ML (2005) Initial experience with antibiotic-impregnated silicone catheters for shunting of cerebrospinal fluid in children. Childs Nerv Syst 21(1):56–61. doi:10.1007/s00381-004-1052-x
Borgbjerg BM, Gjerris F, Albeck MJ, Borgesen SE (1995) Risk of infection after cerebrospinal fluid shunt: an analysis of 884 first-time shunts. Acta Neurochir 136(1–2):1–7
Boynton BR, Boynton CA, Merritt TA, Vaucher YE, James HE, Bejar RF (1986) Ventriculoperitoneal shunts in low birth weight infants with intracranial hemorrhage: neurodevelopmental outcome. Neurosurgery 18(2):141–145
Chapman PH, Borges LF (1985) Shunt infections: prevention and treatment. Clin Neurosurg 32:652–664
Cochrane DD, Kestle JR (2003) The influence of surgical operative experience on the duration of first ventriculoperitoneal shunt function and infection. Pediatr Neurosurg 38(6):295–301. doi:10.1159/000070413
Ersahin Y, Mutluer S, Guzelbag E (1994) Cerebrospinal fluid shunt infections. J Neurosurg Sci 38(3):161–165
Faillace WJ (1995) A no-touch technique protocol to diminish cerebrospinal fluid shunt infection. Surg Neurol 43(4):344–350
Kanev PM, Sheehan JM (2003) Reflections on shunt infection. Pediatr Neurosurg 39(6):285–290. doi:10.1159/000075255
Mancao M, Miller C, Cochrane B, Hoff C, Sauter K, Weber E (1998) Cerebrospinal fluid shunt infections in infants and children in Mobile, Alabama. Acta Paediatr 87(6):667–670
O’Kane MC, Richards H, Winfield P, Pickard JD (1997) The United Kingdom Shunt Registry. Eur J Pediatr Surg: Off J Austrian Assoc Pediatr Surg [et al] = Zeitschrift fur Kinderchirurgie 7(Suppl 1):56
Rehman AU, Rehman TU, Bashir HH, Gupta V (2010) A simple method to reduce infection of ventriculoperitoneal shunts. J Neurosurg Pediatr 5(6):569–572. doi:10.3171/2010.2.PEDS09151
Schoenbaum SC, Gardner P, Shillito J (1975) Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis 131(5):543–552
Gray ED, Peters G, Verstegen M, Regelmann WE (1984) Effect of extracellular slime substance from Staphylococcus epidermidis on the human cellular immune response. Lancet 1(8373):365–367
Peters G, Locci R, Pulverer G (1982) Adherence and growth of coagulase-negative staphylococci on surfaces of intravenous catheters. J Infect Dis 146(4):479–482
Bayston R, Lambert E (1997) Duration of protective activity of cerebrospinal fluid shunt catheters impregnated with antimicrobial agents to prevent bacterial catheter-related infection. J Neurosurg 87(2):247–251. doi:10.3171/jns.1997.87.2.0247
Pattavilakom A, Kotasnas D, Korman TM, Xenos C, Danks A (2006) Duration of in vivo antimicrobial activity of antibiotic-impregnated cerebrospinal fluid catheters. Neurosurgery 58(5):930–935. doi:10.1227/01.NEU.0000210155.65102.E7, discussion 930–935
Demetriades AK, Bassi S (2011) Antibiotic resistant infections with antibiotic-impregnated Bactiseal catheters for ventriculoperitoneal shunts. Br J Neurosurg 25(6):671–673. doi:10.3109/02688697.2011.575478
Govender ST, Nathoo N, van Dellen JR (2003) Evaluation of an antibiotic-impregnated shunt system for the treatment of hydrocephalus. J Neurosurg 99(5):831–839. doi:10.3171/jns.2003.99.5.0831
Gutierrez-Gonzalez R, Boto GR, Fernandez-Perez C, del Prado N (2010) Protective effect of rifampicin and clindamycin impregnated devices against Staphylococcus spp. infection after cerebrospinal fluid diversion procedures. BMC Neurol 10:93. doi:10.1186/1471-2377-10-93
Kan P, Kestle J (2007) Lack of efficacy of antibiotic-impregnated shunt systems in preventing shunt infections in children. Child’s Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 23(7):773–777. doi:10.1007/s00381-007-0296-7
Pattavilakom A, Xenos C, Bradfield O, Danks RA (2007) Reduction in shunt infection using antibiotic impregnated CSF shunt catheters: an Australian prospective study. J Clin Neurosci: Off J Neurosurg Soc Australasia 14(6):526–531. doi:10.1016/j.jocn.2006.11.003
Richards HK, Seeley HM, Pickard JD (2009) Efficacy of antibiotic-impregnated shunt catheters in reducing shunt infection: data from the United Kingdom Shunt Registry. J Neurosurg Pediatr 4(4):389–393. doi:10.3171/2009.4.PEDS09210
Ritz R, Roser F, Morgalla M, Dietz K, Tatagiba M, Will BE (2007) Do antibiotic-impregnated shunts in hydrocephalus therapy reduce the risk of infection? An observational study in 258 patients. BMC Infect Dis 7:38. doi:10.1186/1471-2334-7-38
Steinbok P, Milner R, Agrawal D, Farace E, Leung GK, Ng I, Tomita T, Wang E, Wang N, Wong GK, Zhou LF (2010) A multicenter multinational registry for assessing ventriculoperitoneal shunt infections for hydrocephalus. Neurosurgery 67(5):1303–1310. doi:10.1227/NEU.0b013e3181f07e76
Parker SL, Attenello FJ, Sciubba DM, Garces-Ambrossi GL, Ahn E, Weingart J, Carson B, Jallo GI (2009) Comparison of shunt infection incidence in high-risk subgroups receiving antibiotic-impregnated versus standard shunts. Child’s Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 25(1):77–83. doi:10.1007/s00381-008-0743-0, discussion 85
D’Angio CT, McGowan KL, Baumgart S, St Geme J, Harris MC (1989) Surface colonization with coagulase-negative staphylococci in premature neonates. J Pediatr 114(6):1029–1034
Lamprecht D, Schoeman J, Donald P, Hartzenberg H (2001) Ventriculoperitoneal shunting in childhood tuberculous meningitis. Br J Neurosurg 15(2):119–125
Sil K, Chatterjee S (2008) Shunting in tuberculous meningitis: a neurosurgeon’s nightmare. Child’s Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 24(9):1029–1032. doi:10.1007/s00381-008-0620-x
Bayston R, Ashraf W, Bhundia C (2004) Mode of action of an antimicrobial biomaterial for use in hydrocephalus shunts. J Antimicrob Chemother 53(5):778–782. doi:10.1093/jac/dkh183
Bayston R, Lari J (1974) A study of the sources of infection in colonised shunts. Dev Med Child Neurol 16(6 Suppl 32):16–22
Baird C, O’Connor D, Pittman T (1999) Late shunt infections. Pediatr Neurosurg 31(5):269–273. doi:10.1159/000028874
George R, Leibrock L, Epstein M (1979) Long-term analysis of cerebrospinal fluid shunt infections. A 25-year experience. J Neurosurg 51(6):804–811. doi:10.3171/jns.1979.51.6.0804
Owen R, Pittman T (2004) Delayed external ventriculoperitoneal shunt infection. J Kentucky Med Assoc 102(8):349–352
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raffa, G., Marseglia, L., Gitto, E. et al. Antibiotic-impregnated catheters reduce ventriculoperitoneal shunt infection rate in high-risk newborns and infants. Childs Nerv Syst 31, 1129–1138 (2015). https://doi.org/10.1007/s00381-015-2685-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2685-7