Abstract
Purpose
The purpose of the study was to analyze the surgical outcomes in children (≤18 years) with brachial plexus injury operated between April 2008 and March 2012 at our center.
Methods
All children <18 years of age admitted to our center and surgically treated with a diagnosis of posttraumatic brachial plexus injury were included in the study. The demographic details of these patients were retrieved from the computerized database of our hospital. The results were analyzed in terms of the mode of injury, type of injury, surgical procedure performed, and motor recovery after the surgery (MRC Grading). Motor recovery with MRC >3/5 was termed as good outcome.
Observations
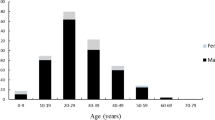
A total of 33 patients were surgically treated. The mean age at presentation was 15.1 (range 4–18) years. Boys constituted 79 % (n = 26) of our patient population. High-velocity injury was the commonest mode of injury. Panbrachial injury was the commonest seen in 82 % (n = 27) of patients. Mean duration between injury and surgical intervention was 6 (range 2–13, SD ± 2.6) months. Majority of patients underwent neurotization procedure. Mean follow-up was 32 (range 6–51) months.
Conclusions
High-velocity trauma is the most common mode on injury. Global palsy involving all the plexal elements was present in 82 % of the children. Neurotization was the most commonly performed surgical procedure. Good motor outcome (MRC grade ≥3/5) was seen in 62 % of patients.





Similar content being viewed by others
References
Alnot JY (1977) Traumatic paralysis of the brachial plexus in the adult. I. Lesions and their mechanism. Rev Chir Orthop Reparatrice Appar Mot 63:39–43
Boome R (2000) Traumatic brachial plexus injuries in children. In: Gupta A, Kay SPJ, Scheker LR (eds) The growing hand: diagnosis management of the upper extremity in children. Mosby, London, pp 653–657
Chuang DC, Lee GW, Hashem F, Wei FC (1995) Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg 96:122–128
D’Aubigne M, Deburge A (1967) Etiology, development and prognosis of traumatic paralysis of the brachial plexus. Rev Chir Orthop Reparatrice Appar Mot 53:23–42
Dumontier C, Gilbert A (1990) Traumatic brachial plexus palsy in children. Ann Chir Main Memb Super 9:351–357
El-Gammal TA, El-Sayed A, Kotb MM (2003) Surgical treatment of brachial plexus traction injuries in children, excluding obstetric palsy. Microsurgery 23:14–17
Narakas A (1982) Neurotization or nerve transfer for brachial plexus lesions. Ann Chir Main 1:101–118
Plutarch (1914) Parallel Lives, I: Lycurgus. Loeb Classical library
Rigault P (1969) Traumatic paralysis of the brachial plexus in children (a study of 7 cases). Rev Chir Orthop Reparatrice Appar Mot 55:125–130
Seddon HJ (1947) The use of autogenous grafts for the repair of large gaps in peripheral nerves. Br J Surg 35:151–167
Sedel L (1977) Palliative treatment of a series of 103 cases of paralysis from elongation of the brachial plexus. Spontaneous changes and results. Rev Chir Orthop Reparatrice Appar Mot 63:651–665
Sever JW (1925) Obstetrical paralysis: report of eleven hundred cases. JAMA 85:1962–1970
Shenaq SM, Bullocks JM, Dhillon G, Lee RT, Laurent JP (2005) Management of infant brachial plexus injuries. Clin Plast Surg 32:79–98, ix
Terzis JK, Kostopoulos VK (2007) The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg 119:73e–92e
Thorburn W (1900) A clinical lecture on secondary suture of the brachial plexus. Br Med J 1:1073–1075
Zheng MX, Qiu YQ, Xu WD, Xu JG (2012) Long-term observation of respiratory function after unilateral phrenic nerve and multiple intercostal nerve transfer for avulsed brachial plexus injury. Neurosurgery 70:796–801, discussion 801
Conflict of interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article. The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
A portion of this work was presented as proceedings at the 40th International Society of Pediatric Neurosurgery Conference 2012, Sydney, Australia, on September 12, 2012.
Rights and permissions
About this article
Cite this article
Garg, K., Sinha, S., Mahapatra, A.K. et al. Microsurgical outcome in posttraumatic brachial plexus injuries in children. Childs Nerv Syst 30, 919–923 (2014). https://doi.org/10.1007/s00381-013-2325-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2325-z