Abstract
Background
Review of children with low-grade cerebellar astrocytoma (LGCA) prior to 1992 showed a 98 % rate of gross total resection (GTR) but a concerning incidence of permanent neurological dysfunction. The purpose of this study was to determine the rate of GTR of LGCA since 1992 and frequency of neurologic injury.
Methods
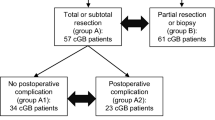
Retrospective review of children with LGCA was performed. CT/MR scans were rereviewed to assess extent of resection. Primary outcomes included incidence of GTR and incidence of permanent new neurological deficits. Other outcomes included late effects severity score (LESS), Bloom score for functional status, and educational assessment.
Results
Of 50 LGCA, GTR was achieved in 38 (76 %) compared to 43 of 44 (98 %) prior to 1992 (p < 0.004). Permanent new neurologic deficits from surgery occurred in 16 % compared to 18 % in the prior era (p = 0.61). For 35 patients operated on by the 2 surgeons in the prior study, 74 % had GTR, with permanent neurological deficits in 8.6 %. At latest follow-up, all patients were alive, 16 % with residual tumor. LESS was two or less (mild or no deficit) in 94 %. Bloom score was one or two (no or mild disability) in 90 %. Eighty-six percent attended normal school.
Conclusions
Less aggressive resection of LGCA in children may reduce postoperative neurologic deficits in the hands of the same surgeons as in the prior study but not overall at our institution. The good long-term outcomes suggest that it may be appropriate to do incomplete resection rather than risk additional neurological deficit.
Similar content being viewed by others
References
Akay KM, Izci Y, Baysefer A, Atabey C, Kismet E, Timurkaynak E (2004) Surgical outcomes of cerebellar tumors in children. Pediatr Neurosurg 40:220–225
Benesch M, Spiegl K, Winter A, Passini A, Lackner H, Moser A, Sovinz P, Schwinger W, Urban C (2009) A scoring system to quantify late effects in children after treatment for medulloblastoma/ependymoma and its correlation with quality of life and neurocognitive functioning. Childs Nerv Syst 25:173–181
Bloom HJ, Wallace EN, Henk JM (1969) The treatment and prognosis of medulloblastoma in children: a study of 82 verified cases. Am J Roentgenol Radium Ther Nucl Med 105:43–62
Bowers DC, Krause TP, Aronson LJ, Barzi A, Burger PC, Carson BS, Weingart JD, Wharam MD, Melhem ER, Cohen KJ (2001) Second surgery for recurrent pilocytic astrocytoma in children. Pediatr Neurosurg 34:229–234
Brossard J, Abish S, Bernstein ML, Baruchel S, Kovacs L, Pollack R (1994) Maternal malignancy involving the products of conception: a report of malignant melanoma and medulloblastoma. Am J Pediatr Hematol Oncol 16:380–383
Cochrane DD, Gustavsson B, Poskitt KP, Steinbok P, Kestle JR (1994) The surgical and natural morbidity of aggressive resection for posterior fossa tumors in childhood. Pediatr Neurosurg 20:19–29
Daszkiewicz P, Maryniak A, Roszkowski M, Barszcz S (2009) Long-term functional outcome of surgical treatment of juvenile pilocytic astrocytoma of the cerebellum in children. Childs Nerv Syst 25:855–860
Desai KI, Nadkarni TD, Muzumdar DP, Goel A (2001) Prognostic factors for cerebellar astrocytomas in children: a study of 102 cases. Pediatr Neurosurg 35:311–317
Dirven CM, Mooij JJ, Molenaar WM (1997) Cerebellar pilocytic astrocytoma: a treatment protocol based upon analysis of 73 cases and a review of the literature. Childs Nerv Syst 13:17–23
Dorward IG, Luo J, Perry A, Gutmann DH, Mansur DB, Rubin JB, Leonard JR (2010) Postoperative imaging surveillance in pediatric pilocytic astrocytomas. Journal of Neurosurgery: Pediatrics 6(4):346–352
Due-Tonnessen BJ, Helseth E, Scheie D, Skullerud K, Aamodt G, Lundar T (2002) Long-term outcome after resection of benign cerebellar astrocytomas in children and young adults (0–19 years): report of 110 consecutive cases. Pediatr Neurosurg 37:71–80
Due-Tonnessen BJ, Lundar T, Egge A, Scheie D (2013) Neurosurgical treatment of low-grade cerebellar astrocytoma in children and adolescents: a single consecutive institutional series of 100 patients. J Neurosurg Pediatr 11:245–249
Fernandez C, Figarella-Branger D, Girard N, Bouvier-Labit C, Gouvernet J, Paz Paredes A, Lena G (2003) Pilocytic astrocytomas in children: prognostic factors—a retrospective study of 80 cases. Neurosurgery 53:544–553, discussion 554–545
Fisher PG, Tihan T, Goldthwaite PT, Wharam MD, Carson BS, Weingart JD, Repka MX, Cohen KJ, Burger PC (2008) Outcome analysis of childhood low-grade astrocytomas. Pediatr Blood Cancer 51:245–250
Gunny RS, Hayward RD, Phipps KP, Harding BN, Saunders DE (2005) Spontaneous regression of residual low-grade cerebellar pilocytic astrocytomas in children. Pediatr Radiol 35:1086–1091
Ogiwara H, Bowman RM, Tomita T (2012) Long-term follow-up of pediatric benign cerebellar astrocytomas. Neurosurgery 70:40–47, discussion 47–48
Palma L, Celli P, Mariottini A (2004) Long-term follow-up of childhood cerebellar astrocytomas after incomplete resection with particular reference to arrested growth or spontaneous tumor regression. Acta Neurochir 146:581–588, discussion 588
Pencalet P, Maixner W, Sainte-Rose C, Lellouch-Tubiana A, Cinalli G, Zerah M, Pierre-Kahn A, Hoppe-Hirsch E, Bourgeois M, Renier D (1999) Benign cerebellar astrocytomas in children. J Neurosurg 90:265–273
Schneider JH Jr, Raffel C, McComb JG (1992) Benign cerebellar astrocytomas of childhood. Neurosurgery 30:58–62, discussion 62–53
Steinbok P, Cochrane DD, Perrin R, Price A (2003) Mutism after posterior fossa tumor resection in children: incomplete recovery on long-term follow-up. Pediatr Neurosurg 39:179–183
Sutton LN, Cnaan A, Klatt L, Zhao H, Zimmerman R, Needle M, Molloy P, Phillips P (1996) Postoperative surveillance imaging in children with cerebellar astrocytomas. J Neurosurg 84:721–725
Vassilyadi M, Shamji MF, Tataryn Z, Keene D, Ventureyra E (2009) Postoperative surveillance magnetic resonance imaging for cerebellar astrocytoma. Can J Neurol Sci 36:707–712
Viano JC, Herrera EJ, Suarez JC (2001) Cerebellar astrocytomas: a 24-year experience. Childs Nerv Syst 17:607–610, discussion 611
Villarejo F, de Diego JM, de la Riva AG (2008) Prognosis of cerebellar astrocytomas in children. Childs Nerv Syst 24:203–210
Conflict of interest
The authors would like to declare that no conflict of interest exists with respect to this study
Financial disclosure
No financial relationships exist with respect to this study. This is an unfunded research project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steinbok, P., Mangat, J.S., Kerr, J.M. et al. Neurological morbidity of surgical resection of pediatric cerebellar astrocytomas. Childs Nerv Syst 29, 1269–1275 (2013). https://doi.org/10.1007/s00381-013-2171-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2171-z