Abstract
Purpose
Brain abscess (BA) and subdural empyema (SDE) are uncommon but clinically important conditions in childhood. Treatment involves surgery and prolonged courses of antibiotics. There is no consensus on the optimal approach. The objective was to review management and outcome of BA and SDE in a single UK center.
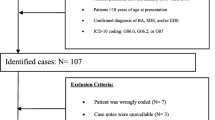
Methods
This retrospective case notes review of children with brain abscess or subdural empyema admitted to a tertiary pediatric infectious diseases and neurosurgical center from 2001 to 2009.
Results
Forty-two children were included in the study; 17 children were with BA, 23 with SDE, and two both with BA and SDE. The causative factors found in 88 % of the patients were most commonly sinusitis and meningitis with congenital heart disease and immunocompromise unusual. Streptococcus anginosus group organisms were most common; 10 % of the children had a resistant pathogen and 86 % had surgical intervention. Fifteen patients with BA underwent surgery; nine of these patients underwent burrhole aspiration, three had craniotomy, two had stereotactic surgery, and one had endoscopic aspiration. Remaining 19 patients with SDE underwent surgery: seven had burrhole aspiration, 11 underwent craniotomy, and one had aspiration via the anterior fontanel. The most common antibiotic regime was cefotaxime, metronidazole, and amoxicillin. Mean duration of treatment was 14.4 weeks. Mean time until normalization of C reactive protein was 23 days. Survival was 95 % and 20 % had ongoing neurological sequelae.
Conclusions
BA and SDE remain important childhood infections in the UK. Antibiotics are essential in the management of these cases. Empiric antibiotic choices require knowledge of likely pathogens and local resistance. Selected infections can be treated without surgical intervention. Long courses of antibiotics were administered. Outcome is good, and neurological sequelae were less common than found in previous series.
Similar content being viewed by others
References
Bockova J, Rigamonti D (2000) Intracranial empyema. The Pediatric Infectious Diseases Journal 19:735–737
Yogev R, Bar-Meir M (2004) Management of brain abscesses in children. The Pediatric Infectious Diseases Journal 23:157–159
Carpenter J, Stapleton S, Holliman R (2007) Retrospective analysis of 49 cases of brain abscess and review of the literature. Eur J Clin Microbiol Infect Dis 26:1–11
Kombogiorgas D, Seth R, Athwal R, Modha J, Singh J (2007) Suppurative intracranial complications of sinusitis in adolescence. Single institute experience and review of literature. British Journal of Neurosurgery 21(6):603–609
Infection in Neurosurgery Working Party of the British Society for Antimicrobial Chemotherapy (2000) The rational use of antibiotics in the treatment of brain abscess. Br J Neurosurg 14(6):525–530
Greenlee JE (2003) Subdural empyema. Current Treatment Options in Neurology 5:13–22
Sharma R, Mohandas K, Cooke RPD (2009) Intracranial abscesses: changes in epidemiology and management over five decades in Merseyside. Infection 37(1):39–43
Leotta N, Chaseling R, Duncan G, Isaacs D (2005) Intracranial suppuration. Journal of Paediatrics and Child Health 41:508–512
Sheehan JP, Jane JA Jr, Ray DK, Goodkin HP (2008) Brain abscess in children. Neurosurgery Focus 24:1–5
Goodkin HP, Harper MB, Pomeroy SL (2004) Intracerebral abscess in children: historical trends at Children's Hospital in Boston. Pediatrics 113(6):1765–1770
Legrand M, Roujeau T, Meyer P, Carli P, Orliaguet G, Blanot S (2009) Paediatric intracranial empyema: differences according to age. Eur J Pediatr 168:1235–1241
Jansson AK, Enblad P, Sjolin J (2004) Efficacy and safety of cefotaxime in combination with metronidazole for empirical treatment of brain abscesses in clinical practice: a retrospective study of 66 consecutive cases. Eur J Clin Microbiol Infect Dis 23:7–14
Bernardini GL (2004) Diagnosis and management of brain abscess and subdural empyema. Current Neurology and Neuroscience Reports 4:448–456
Saez-Llorens X (2003) Brain abscess in children. Semin Pediatr Infect Dis 14(2):108–114
Skoutelis AT, Gogos CA, Maraziotis TE, Bassaris HP (2000) Management of brain abscesses with sequential intravenous/oral antibiotic therapy. Eur J Clin Microbiol Infect Dis 19:332–335
World Health Organization (2007) ICD version 2007. http://apps.who.int/classifications/apps/icd/icd10online/. Accessed 27 Apr 2010
Newcastle Upon Tyne Hospitals NHS Foundation Trust (2009) Antibiotic guidelines. In: A & E handbook of emergency medicine. Newcastle Upon Tyne Hospitals Trust NHS Foundation Trust, Newcastle UK
Tobiansky R, Lui K, Dalton DM, Shaw P, Martin H, Isaacs D (1997) Complications of central venous access devices in children with and without cancer. Journal of Paediatrics & Child Health 33(6):509–514
Conflicts of interest
The authors have no conflicts of interest or funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cole, T.S., Clark, M.E., Jenkins, A.J. et al. Pediatric focal intracranial suppuration: a UK single-center experience. Childs Nerv Syst 28, 2109–2114 (2012). https://doi.org/10.1007/s00381-012-1877-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1877-7