Abstract
Introduction
The current SIOP (International Society for Paediatric Oncology)-LGG (low grade glioma) study protocol allows chiasmatic tumours identified as LGG on the basis of neuroradiological characteristics to be treated without histological verification. As some tumours do not respond well to treatment, the search for molecular tissue markers will gain importance for future studies. Anecdotal observations of infarctions after surgery for chiasmatic tumours during central reviewing initiated this study.
Materials and methods
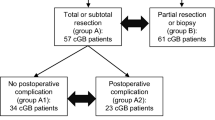
In 84 patients, histology was obtained during 102 interventions in the years 1992–2009 by 33 biopsies, 67 partial/subtotal and 2 total resections. Median age at the time of operation was 5 years (mean 5 years 11 months). We could identify 17 infarctions following partial resection of chiasmatic LGG. Biopsies were not complicated by infarction. Children developing infarction were considerably younger (median 3 years; mean 4 years 5 months) than the patients without infarction (median 5 years 4 months; mean 6 years 2 months). A total of 51 patients with cerebellar LGG (median 7 years; mean 7 years 4 months) served as a control group, with 65 surgical procedures (2 biopsies, 22 partial/subtotal resections and 41 total resections) performed in the years 2004–2009. Only one total resection (1.5%) in this group was followed by infarction.
Conclusion
Partial/subtotal resections of chiasmatic LGG in our study population bear a considerable risk for infarction especially in young children. As there is currently no evidence for a better outcome after tumour resection, we suggest that the sampling of tumour tissue should be performed via biopsies whenever possible.


Similar content being viewed by others
References
Ahn Y, Cho BK, Kim SK, Chung YN, Lee CS, Kim IH et al (2006) Optic pathway glioma: outcome and prognostic factors in a surgical series. Childs Nerv Syst 22:1136–1142
Binning MJ, Liu JK, Kestle JR, Brockmeyer DL, Walker ML (2007) Optic pathway gliomas: a review. Neurosurg Focus 23:E2
Czyzyk E, Jóźwiak S, Roszkowski M, Schwartz RA (2003) Optic pathway gliomas in children with and without neurofibromatosis 1. J Child Neurol 18:471–478
Dodge HW, Love JG, Craig WM, Dockerty MB, Kearns TP, Holman CB et al (1958) Gliomas of the optic nerves. AMA Arch Neurol Psychiatry 79:607–621
Giannini C, Scheithauer BW, Burger PC, Christensen MR, Wollan PC, Sebo TJ et al (1999) Cellular proliferation in pilocytic and diffuse astrocytomas. J Neuropathol Exp Neurol 58:46–53
Jost SC, Ackerman JW, Garbow JR, Manwaring LP, Gutmann DH, McKinstry RC (2008) Diffusion-weighted and dynamic contrast-enhanced imaging as markers of clinical behavior in children with optic pathway glioma. Pediatr Radiol 38:1293–1299
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) WHO classification of tumours of the central nervous system, 4th edn. IARC Press, Lyon
Nicolin G, Parkin P, Mabbott D, Hargrave D, Bartels U, Tabori U et al (2009) Natural history and outcome of optic pathway gliomas in children. Pediatr Blood Cancer 53:1231–1237
Nishio S, Takeshita I, Fujiwara S, Fukui M (1993) Optico-hypothalamic glioma: an analysis of 16 cases. Childs Nerv Syst 9:334–338
Perilongo G, Moras P, Carollo C, Battistella A, Clementi M, Laverda A et al (1999) Spontaneous partial regression of low-grade glioma in children with neurofibromatosis-1: a real possibility. J Child Neurol 14:352–356
Piccirilli M, Lenzi J, Delfinis C, Trasimeni G, Salvati M, Raco A (2006) Spontaneous regression of optic pathways gliomas in three patients with neurofibromatosis type I and critical review of the literature. Childs Nerv Syst 22:1332–1337
Sawamura Y, Kamada K, Kamoshima Y, Yamaguchi S, Tajima T, Tsubaki J et al (2008) Role of surgery for optic pathway/hypothalamic astrocytomas in children. Neurooncology 10:725–733
Sievert AJ, Fisher MJ (2009) Pediatric low-grade gliomas. J Child Neurol 24:1397–1408
Singh R, Trobe JD, Hayman JA, Deveikis JP (2004) Ophthalmic artery occlusion secondary to radiation-induced vasculopathy. J Neuroophthalmol 24:206–210
Steinbok P, Hentschel S, Almqvist P, Cochrane DD, Poskitt K (2002) Management of optic chiasmatic/hypothalamic astrocytomas in children. Can J Neurol Sci 29:132–138
Sutton LN, Molloy PT, Sernyak H, Goldwein J, Phillips PL, Rorke LB et al (1995) Long-term outcome of hypothalamic/chiasmatic astrocytomas in children treated with conservative surgery. J Neurosurg 83:583–589
Valdueza JM, Lohmann F, Dammann O, Hagel C, Eckert B, Freckmann N (1994) Analysis of 20 primarily surgically treated chiasmatic/hypothalamic pilocytic astrocytomas. Acta Neurochir (Wien) 126:44–50
Warmuth-Metz M, Gnekow AK, Müller H, Solymosi L (2004) Differential diagnosis of suprasellar tumors in children. Klin Padiatr 216:323–330
Wisoff JH, Abbott R, Epstein F (1990) Surgical management of exophytic chiasmatic-hypothalamic tumors of childhood. J Neurosurg 73:661–667
Acknowledgements
This work was supported by the German Childhood Cancer Foundation (Deutsche Kinderkrebsstiftung).
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Parts of the content were presented
- in a lecture at the 14th International Symposium on Paediatric Neurooncology, Vienna, Austria, June 20–23, 2010
- in a lecture at the XIX Symposium Neuroradiologicum, Bologna, Italy, October 4–9, 2010
- in a poster at the annual meeting of the German Society of Neuroradiology, Cologne, Germany, October 7, 2010.
Rights and permissions
About this article
Cite this article
Hupp, M., Falkenstein, F., Bison, B. et al. Infarction following chiasmatic low grade glioma resection. Childs Nerv Syst 28, 391–398 (2012). https://doi.org/10.1007/s00381-011-1605-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-011-1605-8