Abstract
Aims
The aims of this study were to analyze the clinical features, radiologic findings, bacteriologic spectrum, and management protocols and outcomes in posterior fossa subdural empyemas in children.
Materials and methods
This study is a retrospective analysis of all children (age, <18 years) treated over a ten-year period (1994–2004) at NIMHANS, India. Clinical, bacteriologic, radiologic, and follow-up data were analyzed.
Results
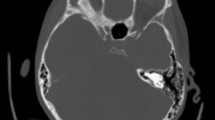
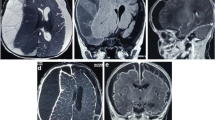
Twenty-seven children with posterior fossa empyemas were treated during this period, making this the largest series to date dealing with this rare entity. Posterior fossa empyemas are seen more commonly in the summer months and in males. Of the patients, 74.1% were in altered sensorium. The clinical features included the triad of fever, headache, and vomiting, which is a nonspecific picture. Cerebellar signs were elicited only in 40%. The most common source was untreated middle ear infection. Pus usually accumulates over the cerebellar convexity and is associated with hydrocephalus in 74% of patients. Cultures of the empyema pus were positive in 74% of cases, and 18.5% had polymicrobial infections. Only 21% of the patients needed a permanent CSF diversion procedure. Craniectomy is the treatment of choice in these cases.
Conclusions
The clinical features are nonspecific. Early surgery can salvage most patients and obviate the need for permanent CSF diversion procedures. Surgery (evacuation of empyema and mastoidectomy), antibiotics, and management of hydrocephalus are the mainstays of treatment.



Similar content being viewed by others
References
Venkatesh MS, Pandey P, Indira Devi B, Khanapure K, Satish S, Sampath S, Chandramouli BA, Sastry KVR (2006) Pediatric infratentorial subdural empyema: analysis of 14 cases. J Neurosurg Ped 105(5):370–377
Nathoo N, Nadvi SS, van Dellen JR (1997) Infratentorial empyema: analysis of 22 cases. Neurosurg 41:1263–1269
Nathoo N, Nadvi SS, Gouws E, van Dellen JR (2001) Craniotomy improves outcomes for cranial subdural empyemas: computed tomography-era experience with 699 patients. Neurosurg 49:872–878
Borovich B, Johnson E, Spagnuolo E (1990) Infratentorial subdural empyema: clinical and CT findings—Report of 3 cases. J Neurosurg 72:299–301
Courville CB (1944) Subdural empyema secondary to purulent frontal sinusitis: a clinicopathological study of 42 cases verified at autopsy. Arch Otolaryngol 39:211–230
Kojima A, Yamaguchi N, Okui S (2004) Supra- and infratentorial subdural empyema secondary to septicemia in a patient with liver abscess—case report. Neurol Med Chir (Tokyo) 44(2):90–93
Morgan DW, Williams B (1985) Posterior fossa subdural empyema. Brain 108:983–992
Pathak A, Sharma BS, Mathuriya SN, Khosla VK, Khandelwal N, Kak VK (1990) Controversies in the management of subdural empyemas: a study of 11 cases with review of the literature. Acta Neurochir (Wien) 102:25–32
Pattisapu JV, Parent AD (1987) Subdural empyemas in the children. Pediatr Neurosci 13:251–254
Polyzoidis KS, Vranos G, Exarchakos G, Argyropoulou MI, Korantzopoulos P, Skevas A (2004) Subdural empyema and cerebellar abscess due to chronic otitis media. Int J Clin Pract 58(2):214–217
Ralib A R M, Ariff A R M, Shuaib I L (2004) Analysis of Pediatric Subdural Empyema Outcome in Relation to computerized tomography brain scan Southeast Asian J Trop Med Public Health 35(2):434–444.
Sahjpaul RL, Lee DH (1999) Infratentorial subdural empyema, pituitary abscess, and septic cavernous sinus thrombophlebitis secondary to paranasal sinusitis: case report. Neurosurg 44(4):864–866
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Madhugiri, V.S., Sastri, B.V.S., Bhagavatula, I.D. et al. Posterior fossa subdural empyema in children—management and outcome. Childs Nerv Syst 27, 137–144 (2011). https://doi.org/10.1007/s00381-010-1169-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1169-z