Abstract
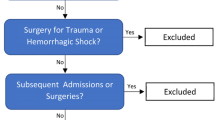
Although intraoperative intravenous fluids are commonly administered to reverse intraoperative hypotension during cardiac surgery, the appropriate volume remains unclear. This study aimed to evaluate the relationship between the intraoperative fluid balance and sequential organ failure assessment (SOFA) score in patients undergoing cardiac surgery to determine the impact of intraoperative intravenous fluids on their organs. This was a post hoc analysis using data from a multicenter, retrospective, observational study across 14 intensive care units (ICUs) in Japan. Adult patients admitted to ICUs after elective coronary artery bypass grafting or valve surgery from January 1 to December 31, 2018 were enrolled. We compared patients with intraoperative fluid balance < 20 ml/kg to those with fluid balance ≥ 20 ml/kg and conducted a multiple regression analysis for the SOFA score within 24 h of ICU admission. Of the 1567 included patients, 870 met the eligibility criteria. A total of 725 patients (83%) had an intraoperative fluid balance of ≥ 20 ml/kg. In the univariate analysis, the SOFA score (interquartile range) was 7 (6–8) and 7 (6–9) in the intraoperative fluid balance < 20 ml/kg and ≥ 20 ml/kg groups, respectively (p = 0.017). Multiple regression analysis showed a positive association between intraoperative fluid balance and SOFA score within 24 h of ICU admission [standardized coefficient 0.0065 (95% confidence interval 0.0036–0.0095), p < 0.001]. Intraoperative fluid balance in patients undergoing cardiac surgery was significantly associated with higher SOFA scores within 24 h of ICU admission.

Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author, TK, upon reasonable request.
References
Jozwiak M, Monnet X, Teboul JL (2018) Prediction of fluid responsiveness in ventilated patients. Ann Transl Med 6:352
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Andrews B, Semler MW, Muchemwa L, Kelly P, Lakhi S, Heimburger DC, Mabula C, Bwalya M, Bernard GR (2017) Effect of an early resuscitation protocol on in-hospital mortality among adults with sepsis and hypotension: a randomized clinical trial. JAMA 318:1233–1240
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettilä V, Aaen A, Lodahl D, Berthelsen RE, Christensen H, Madsen MB, Winkel P, Wetterslev J, Perner A, CLASSIC Trial Group; Scandinavian Critical Care Trials Group (2016) Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med 42:1695–1705
Raimundo M, Crichton S, Martin JR, Syed Y, Varrier M, Wyncoll D, Ostermann M (2015) Increased fluid administration after early acute kidney injury is associated with less renal recovery. Shock 44:431–437
Tritapepe L (2013) Hypotension during surgery for high risk patients: cause or consequence of pathology? Minerva Anestesiol 79:978–990
Hogue CW, Gottesman RF, Stearns J (2008) Mechanisms of cerebral injury from cardiac surgery. Crit Care Clin 24:83–98
Boer F, Ros P, Bovill JG, van Brummelen P, van der Krogt J (1990) Effect of propofol on peripheral vascular resistance during cardiopulmonary bypass. Br Anaesth 65:184–189
Brienza N, Giglio MT, Marucci M, Fiore T (2009) Does perioperative hemodynamic optimization protect renal function in surgical patients? A meta-analytic study. Crit Care Med 37:2079–2090
Kouz K, Hoppe P, Briesenick L, Saugel B (2020) Intraoperative hypotension: pathophysiology, clinical relevance, and therapeutic approaches. Indian J Anaesth 64:90–96
Wu NH, Hsieh TH, Chang CY, Shih PC, Kao MC, Lin HY (2023) Validation of cardiac output estimation using the fourth-generation FloTrac/EV1000™ system in patients undergoing robotic-assisted off-pump coronary artery bypass surgery. Heart Vessels 38:341–347
Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL, Program to Improve Care in Acute Renal Disease (PICARD) Study Group (2009) Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int 76:422–427
Claure-Del Granado R, Mehta RL (2016) Fluid overload in the ICU: evaluation and management. BMC Nephrol 17:109
Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM, Sepsis Occurrence in Acutely Ill Patients Investigators (2005) High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest 128:3098–3108
van Mourik N, Metske HA, Hofstra JJ, Binnekade JM, Geerts BF, Schultz MJ, Vlaar APJ (2019) Cumulative fluid balance predicts mortality and increases time on mechanical ventilation in ARDS patients: an observational cohort study. PLoS One 14:e0224563
Chen X, Xu J, Li Y, Shen B, Jiang W, Luo Z, Wang C, Teng J, Ding X, Lv W (2021) The effect of postoperative fluid balance on the occurrence and progression of acute kidney injury after cardiac surgery. J Cardiothorac Vasc Anesth 35:2700–2706
Stein A, de Souza LV, Belettini CR, Menegazzo WR, Viégas JR, Costa Pereira EM, Eick R, Araújo L, Consolim-Colombo F, Irigoyen MC (2012) Fluid overload and changes in serum creatinine after cardiac surgery: predictors of mortality and longer intensive care stay. A prospective cohort study. Crit Care 16:R99
Shahidi Delshad E, Sanadgol H, Bakhshandeh H, Saberian M, Alavi SM (2020) Fluid balance has effects on the length of hospital stay after coronary artery bypass grafting surgery. Iran J Kidney Dis 14:36–43
Dass B, Shimada M, Kambhampati G, Ejaz NI, Arif AA, Ejaz AA (2012) Fluid balance as an early indicator of acute kidney injury in CV surgery. Clin Nephrol 77:438–444
Shen Y, Zhang W, Cheng X, Ying M (2018) Association between postoperative fluid balance and acute kidney injury in patients after cardiac surgery: a retrospective cohort study. J Crit care 44:273–277
Mailhot T, Cossette S, Lambert J, Beaubien-Souligny W, Cournoyer A, O’Meara E, Maheu-Cadotte MA, Fontaine G, Bouchard J, Lamarche Y, Benkreira A, Rochon A, Denault A (2019) Delirium after cardiac surgery and cumulative fluid balance: a case-control cohort study. J Cardiothorac Vasc Anesth 33:93–101
Kotani Y, Yoshida T, Kumasawa J, Kamei J, Taguchi A, Kido K, Yamaguchi N, Kariya T, Nakasone M, Mikami N, Koga T, Nakayama I, Shibata M, Yoshida T, Nashiki H, Karatsu S, Nogi K, Tokuhira N, Izawa J (2021) The impact of relative hypotension on acute kidney injury progression after cardiac surgery: a multicenter retrospective cohort study. Ann Intensive Care 11:178
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med 22:707–710
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Caruso D, De Santis D, Rivosecchi F, Zerunian M, Panvini N, Montesano M, Biondi T, Bellini D, Rengo M, Laghi A (2018) Lean body weight-tailored iodinated contrast injection in obese patient: Boer versus James formula. Biomed Res Int 2018:8521893
Smith BB, Mauermann WJ, Yalamuri SM, Frank RD, Gurrieri C, Arghami A, Smith MM (2020) Intraoperative fluid balance and perioperative outcomes after aortic valve surgery. Ann Thorac Surg 110:1286–1293
Semler MW, Rice TW, Shaw AD, Siew ED, Self WH, Kumar AB, Byrne DW, Ehrenfeld JM, Wanderer JP (2016) Identification of major adverse kidney events within the electronic health record. J Med Syst 40:167
Leballo G, Moutlana HJ, Muteba MK, Chakane PM (2021) Factors associated with acute kidney injury and mortality during cardiac surgery. Cardiovasc J Afr 32:308–313
Amini S, Najafi MN, Karrari SP, Mashhadi ME, Mirzaei S, Tashnizi MA, Moeinipour AA, Hoseinikhah H, Aazami MH, Jafari M (2019) Risk factors and outcome of acute kidney injury after isolated CABG surgery: a prospective cohort study. Braz J Cardiovasc Surg 34:70–75
Yi Q, Li K, Jian Z, Xiao YB, Chen L, Zhang Y, Ma RY (2016) Risk Factors for acute kidney injury after cardiovascular surgery: evidence from 2157 cases and 49,777 controls—a meta-analysis. Cardiorenal Med 6:237–250
Najjar M, Yerebakan H, Sorabella RA, Donovan DJ, Kossar AP, Sreekanth S, Kurlansky P, Borger MA, Argenziano M, Smith CR, George I (2015) Acute kidney injury following surgical aortic valve replacement. J Card Surg 30:631–639
Kogan A, Preisman S, Levin S, Raanani E, Sternik L (2014) Adult respiratory distress syndrome following cardiac surgery. J Card Surg 29:41–46
Christenson JT, Aeberhard JM, Badel P, Pepcak F, Maurice J, Simonet F, Velebit V, Schmuziger M (1996) Adult respiratory distress syndrome after cardiac surgery. Cardiovasc Surg 4:15–21
Kaul TK, Fields BL, Riggins LS, Wyatt DA, Jones CR, Nagle D (1998) Adult respiratory distress syndrome following cardiopulmonary bypass: incidence, prophylaxis and management. J Cardiovasc Surg (Torino) 39:777–781
Chen SW, Chang CH, Chu PH, Chen TH, Wu VC, Huang YK, Liao CH, Wang SY, Lin PJ, Tsai FC (2016) Risk factor analysis of postoperative acute respiratory distress syndrome in valvular heart surgery. J Crit Care 31:139–143
Asimakopoulos G, Taylor KM, Smith PL, Ratnatunga CP (1999) Prevalence of acute respiratory distress syndrome after cardiac surgery. J Thorac Cardiovasc Surg 117:620–621
Palomba H, Treml RE, Caldonazo T, Katayama HT, Gomes BC, Malbouisson LMS, Silva Junior JM (2022) Intraoperative fluid balance and cardiac surgery-associated acute kidney injury: a multicenter prospective study. Braz J Anesthesiol 72:688–694
Pradeep A, Rajagopalam S, Kolli HK, Patel N, Venuto R, Lohr J, Nader ND (2010) High volumes of intravenous fluid during cardiac surgery are associated with increased mortality. HSR Proc Intensive Care Cardiovasc Anesth 2:287–296
Wrzosek A, Jakowicka-Wordliczek J, Zajaczkowska R, Serednicki WT, Jankowski M, Bala MM, Swierz MJ, Polak M, Wordliczek J (2019) Perioperative restrictive versus goal-directed fluid therapy for adults undergoing major non-cardiac surgery. Cochrane Database Syst Rev 12:C012767
Lobo SM, Ronchi LS, Oliveira NE, Brandão PG, Froes A, Cunrath GS, Nishiyama KG, Netinho JG, Lobo FR (2011) Restrictive strategy of intraoperative fluid maintenance during optimization of oxygen delivery decreases major complications after high-risk surgery. Crit Care 15:R226
Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, Christophi C, Leslie K, McGuinness S, Parke R, Serpell J, Chan MTV, Painter T, McCluskey S, Minto G, Wallace S, Australian and New Zealand College of Anaesthetists Clinical Trials Network and the Australian and New Zealand Intensive Care Society Clinical Trials Group (2018) Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med 378:2263–2274
Acknowledgements
We would like to thank the following colleagues from the participating hospitals associated with the BROTHER study, who performed the extensive data entry, namely: Jikei University School of Medicine: Takuo Yoshida; Kameda Medical Center: Yuki Kotani; Okinawa Chubu Hospital: Izumi Nakayama; Tottori University Faculty of Medicine: Masato Nakasone; Wakayama Medical University: Mami Shibata; Hokkaido University Hospital: Tomonao Yoshida; Kobe City Medical Center General Hospital: Akihisa Taguchi, Daisuke Kawakami; Hirosaki University Graduate School of Medicine: Noriko Mikami, Junichi Saito, Mirei Kubota, Tsubasa Oyama; Kurashiki Central Hospital: Jun Kamei; Yokohama City Minato Red Cross Hospital: Isao Nagata, Shinsuke Karatsu; Tokyo Bay Urayasu Ichikawa Medical Center: Naoki Yamaguchi; Yokohama City University Hospital: Takayuki Kariya; Iwate Prefectural Central Hospital: Hiroshi Nashiki; and Hiroshima Citizens Hospital: Koji Kido, Hiroki Omiya.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
TK had full access to all data in the study and takes responsibility for the integrity of the data. Study concept and design: TK, TY, and YK. Acquisition of data: TK, TY and YK. Analysis and interpretation of data: TK, TY, and YK. Drafting of the manuscript: TK. Critical revision of the manuscript for important intellectual content: TK, TY, and YK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The ethics committee of The Kameda Medical Center (No. 19-013) and the ethics committees of all other participating hospitals approved the opt-out method of informed consent. As this was a retrospective cohort study, we applied the opt-out method to obtain informed consent for participation.
Consent for publication
As this was a retrospective cohort study, we applied the opt-out method of informed consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the BROTHER study group are presented in Acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koga, T., Yoshida, T., Kotani, Y. et al. Association between the intraoperative fluid balance during cardiac surgery and postoperative sequential organ failure assessment score: a post hoc analysis of the BROTHER study, a retrospective multicenter cohort study. Heart Vessels 39, 57–64 (2024). https://doi.org/10.1007/s00380-023-02306-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-023-02306-0