Abstract
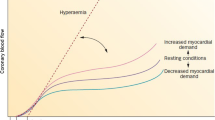
To evaluate the myocardial flow reserve (MFR) and myocardial blood flow (MBF) parameters in patients with heart failure with preserved ejection fraction (HFpEF) and to assess their relationship with the severity of HF and the levels of soluble ST2 (sST2). A total of 59 consecutive patients (median age of 65.0 (58.0; 69.0) years) with non-obstructive coronary artery disease (CAD) and preserved EF were enrolled. Serum levels biomarkers were measured by enzyme immunoassay. MBF and MFR parameters were evaluated by dynamic CZT-SPECT. All patients were divided into two groups: group 1 comprised patients (n = 41) with HFpEF, and group 2 comprised those (n = 18) without HFpEF. In group 1 global MFR (gMFR) values were lower by 27.8% (p = 0.003) than in group 2. The values of gMFR correlated with NT-proBNP (r = − 0.290) and sST2 (r = −0.331) levels. Based on ROC-analysis, gMFR ≤ 2.27 (AUC = 0.746; p < 0.001) were associated with the presence of HFpEF. In patients with HFpEF (n = 41) the values of gMFR were related to NYHA classes (p < 0.001) and the parameters of diastolic dysfunction (p < 0.001). The values of gMFR ≤ 2.27 may be used for the evaluation of microvascular changes in patients with HFpEF and non-obstructive CAD.





Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- CFR:
-
Coronary flow reserve
- CMD:
-
Coronary microvascular dysfunction
- CMRI:
-
Cardiac magnetic resonance imaging
- HFpEF:
-
Heart failure with preserved ejection fraction
- MBF:
-
Myocardial blood flow
- MFR:
-
Myocardial flow reserve
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- PET:
-
Positron emission tomography
- sST2:
-
Soluble suppression of tumorigenicity 2
- TTDE:
-
Transthoracic Doppler echocardiography
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, Meer P (2016) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37(27):2129–2200
Likoff W, Segal BL, Kasparian H (1967) Paradox of normal selective coronary arteriograms in patients considered to have unmistakable coronary heart disease. N Engl J Med 276:1063–1066
Vancheri F, Longo G, Vancheri S, Henein M (2020) Coronary microvascular dysfunction. J Clin Med 9:2880
Taqueti VR, Di Carli MF (2016) Clinical significance of noninvasive coronary flow reserve assessment in patients with ischemic heart disease. Curr Opin Cardiol 31(6):662–669
Ong P, Safdar B, Seitz A, Hubert A, Beltrame JF, Prescott E (2020) Diagnosis of coronary microvascular dysfunction in the clinic. Cardiovasc Res 116(4):841–855
Driessen RS, Raijmakers PG, Stuijfzand WJ, Knaapen P (2017) Myocardial perfusion imaging with PET. Int J Cardiovasc Imaging 33:1021–1031
Rahman H, Scannell CM, Demir OM, Ryan M, McConkey H, Ellis H, Masci PG, Perera D, Chiribiri A (2021) High-resolution cardiac magnetic resonance imaging techniques for the identification of coronary microvascular dysfunction. JACC Cardiovasc Imaging 14(5):978–986
Zavadovsky KV, Mochula AV, Boshchenko AA, Vrublevsky AV, Baev AE, Krylov AL, Gulya MO, Nesterov EA, Liga R, Gimelli A (2021) Absolute myocardial blood flows derived by dynamic CZT scan vs invasive fractional flow reserve: correlation and accuracy. J Nucl Cardiol 28(1):249–259
Agostini D, Roule V, Nganoa C, Roth N, Baavour R, Parienti JJ, Beygui F, Manrique A (2018) First validation of myocardial flow reserve assessed by dynamic 99mTc-sestamibi CZT-SPECT camera: head to head comparison with 15O-water PET and fractional flow reserve in patients with suspected coronary artery disease. The WATERDAY study. Eur J Nucl Med Mol Imaging 45(7):1079–1090
Paulus WJ, Tschöpe C (2013) A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 62(4):263–271
van Heerebeek L, Franssen CPM, Hamdani N, Verheugt FWA, Somsen GA, Paulus WJ (2012) Molecular and cellular basis for diastolic dysfunction. Curr Heart Fail Rep 9(4):293–302
Grakova EV, Kopieva KV, Teplyakov AT, Ogurkova ON, Soldatenko MV, Garganeeva AA (2019) Clinical use of the new biomarker ST2 in patients with chronic heart failure of ischemic genesis: an exercise test. Cardiovasc Ther and Prev 18(4):12–18
Filali Y, Kesäniemi A, Ukkola O (2021) Soluble ST2, a biomarker of fibrosis, is associated with multiple risk factors, chronic diseases and total mortality in the OPERA study. Scand J Clin Lab Invest 81(4):324–331
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 29(4):277–314
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc committee for grading of coronary artery disease, council on cardiovascular surgery. Am Heart Assoc Circ 51:5–40
Zavadovsky KV, Mochula AV, Maltseva AN, Boshchenko AA, Baev AE, Andreev SL, Nesterov EA, Liga R, Gimelli A (2022) The diagnostic value of SPECT CZT quantitative myocardial blood flow in high-risk patients. J Nucl Cardiol 29(3):1051–1063
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS (2006) Quality assurance committee of the American society of nuclear cardiology. stress protocols and tracers. J Nucl Cardiol 13:e80-90
Leppo JA, Meerdink DJ (1989) Comparison of the myocardial uptake of a technetium-labeled isonitrile analog and thallium. Circ Res 65(3):632–639
Zavadovsky KV, Mochula AV, Maltseva AN, Shipulin VV, Sazonova SI, Gulya MO, Liga R, Gimelli A (2021) The current status of CZT SPECT myocardial blood flow and reserve assessment: tips and tricks. J Nucl Cardiol. https://doi.org/10.1007/s12350-021-02620-y
Mochula A, Zavadovsky K, Andreev S, Lishmanov YU (2016) Dynamic single-photon emission computed tomography data analysis: capabilities for determining functional significance of coronary artery atherosclerosis. MATEC Web Conf 79:1–6
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the cardiac imaging. Circulation 105(4):539–542
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Celutkiene J, Chioncel O, Cleland JG, Coats AJ, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CS, Lyon AR, McMurray JJ, Mebazaa A, Mindham R, Muneretto C, Piepoli MF, Price S, Rosano GM, Ruschitzka F, Skibelund AK (2021) 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC) with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J 42(36):3599–3726
Clark KAA, Velazquez EJ (2020) Heart failure with preserved ejection fraction: time for a reset. JAMA 324(15):1506–1508
Groenewegen A, Rutten FH, Mosterd A, Hoes AW (2020) Epidemiology of heart failure. Eur J Heart Fail 22(8):1342–1356
Wintrich J, Kindermann I, Ukena C, Selejan S, Werner C, Maack C, Laufs U, Tschope C, Anker SD, Lam CP, Voors AA, Bohm M (2020) Therapeutic approaches in heart failure with preserved ejection fraction: past, present, and future. Clin Res Cardiol 109:1079–1098
Tona F, Montisci R, Iop L, Civieri G (2021) Role of coronary microvascular dysfunction in heart failure with preserved ejection fraction. Rev Cardiovasc Med 22(1):97–104
Triposkiadis F, Butler J, Abboud FM, Armstrong PW, Adamopoulos S, Atherton JJ, Backs J, Bauersachs BD, Eonow RO, Chopra VK, de Boer RA, de Windt L, Hamdani N, Hasenfuss G, Heymans S, Hulot JS, Konstam M, Lee RT, Linke WA, Lunde IG, Lyon AR, Maack C, Mann DL, Mebazaa A, Mentz RJ, Nihoyannopoulos P, Papp Z, Parissis J, Pedrazzini T, Rosano G, Rouleau J, Seferovic PM, Shah AM, Starling RC, Tocchetti CG, Trochu JN, Thum T, Zannad F, Brutsaert DL, Segers VF, De Keulenaer GW (2019) The continuous heart failure spectrum: moving beyond an ejection fraction classification. Eur Heart J 40(26):2155–2163
Graziani F, Varone F, Crea F, Richeldi L (2018) Treating heart failure with preserved ejection fraction: learning from pulmonary fibrosis. Eur J Heart Fail 20(10):1385–1391
Godo S, Suda A, Takahashi J, Yasuda S, Shimokawa H (2021) Coronary microvascular dysfunction. Arterioscler Thromb Vasc Biol 41:1625–1637
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, Dorbala S, Blankstein R, Rimoldi O, Camici PG, Di Carli MF (2014) Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 129:2518–2527
Borbély A, van der Velden J, Papp Z, Bronzwaer JGF, Edes I, Stienen GJM, Paulus WJ (2005) Cardiomyocyte stiffness in diastolic heart failure. Circulation 111:774–781
Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan R, Beussink-Nelson L, Faxen UL, Fermer ML, Broberg MA, Gan LM, Lund LH (2018) Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J 39:3439–3450
Schroder J, Prescott E (2021) Doppler echocardiography assessment of coronary microvascular function in patients with angina and no obstructive coronary artery disease. Front Cardiovasc Med 8:723542
Knuuti J, Wijns W, Sarate A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ (2020) 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477
Srivaratharajah K, Coutinho T, deKemp R, Liu P, Haddad H, Stadnick E, Davies RA, Chih S, Dwivedi G, Guo A, Wells GA, Bernick J, Beanlands R, Mielniczuk LM (2016) Reduced myocardial flow in heart failure patients with preserved ejection fraction. Circ Heart Fail 9(7):e002562
Schindler TH, Schelbert HR, Quercioli A, Dilsizian V (2010) Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imaging 3(6):623–640
Kato S, Saito N, Kirigaya H, Gyotoku D, Iinuma N, Kusakawa Y, Iguchi K, Nakachi T, Fukui K, Futaki M, Iwasawa T, Kimura K, Umemura S (2016) Impairment of coronary flow reserve evaluated by phase contrast cine magnetic resonance imaging in patients with heart failure with preserved ejection fraction. J Am Heart Assoc 5(2):e002649
Löffler AI, Pan JA, Balfour PC, Shaw PW, Yang Y, Nasir M, Auger DA, Epstein FH, Kramer CM, Gan LM, Salerno MS (2019) Frequency of coronary microvascular dysfunction and diffuse myocardial fibrosis (measured by cardiovascular magnetic resonance) in patients with heart failure and preserved left ventricular ejection fraction. Am J Cardiol 124(10):1584–1589
Wells RG, Timmins R, Klein R, Lockwood J, Marvin B, deKemp RA, Wei L, Ruddy TD (2014) Dynamic SPECT measurement of absolute myocardial blood flow in a porcine model. J Nucl Med 55:1685–1691
Dryer K, Gajjar M, Narang N, Lee M, Paul J, Shah AP, Nathan S, Butler J, Davidson CJ, Fearon WF, Shan SJ, Blair JA (2018) Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am J Physiol Heart Circ Physiol 314(5):H1033-1042
Ahmad A, Corban MT, Toya T, Verbrugge FH, Sara JD, Lerman LO, Borlaug BA, Lerman A (2021) Coronary microvascular dysfunction is associated with exertional haemodynamic abnormalities in patients with heart failure with preserved ejection fraction. Eur J Heart Fail 23(5):765–772
Galderisi M, Cicala S, Caso P, De Simone L, D’Errico A, Petrocelli A, de Divitiis O (2002) Coronary flow reserve and myocardial diastolic dysfunction in arterial hypertension. Am J Cardiol 90(8):860–864
Kim IC, Hwang J, Lee CH, Cho YK, Park HS, Chung JW, Yoon HJ, Kim H, Han S, Hur SH, Koo BK, Doh JH, Shin ES, Lee JM, Nam CW (2020) Correlation of coronary microvascular function and diastolic dysfunction. Eur Heart J. https://doi.org/10.1093/ehjci/ehaa946.0903
Snoer M, Monk-Hansen T, Olsen RH, Pedersen LR, Nielsen OW, RasmusenH DF, Prescott E (2013) Coronary flow reserve as a link between diastolic and systolic function and exercise capacity in heart failure. Eur Heart J Cardiovasc Imaging 14(7):677–683
Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, Hainer J, Bibbo CF, Dorbala S, Blankstein R, Di Carli MF (2018) Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J 39(10):840–849
Mohammed SF, Hussain S, Mirzoyev SA, Edwards WD, Maleszewski JJ, Redfield MM (2015) Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation 131(6):550–559
Crea F, Bairey Merz CN, Beltrame JF, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Camici PG (2017) Coronary vasomotion disorders international study group (COVADIS). The parallel tales of microvascular angina and heart failure with preserved ejection fraction: a paradigm shift. Eur Heart J 38(7):473–477
Zhang X, Karunathilaka N, Senanayake S, Subramaniam VN, Chan W, Kostner K, Fraser J, Atherton JJ, Punyadeera C (2019) The potential prognostic utility of salivary galectin-3 concentrations in heart failure. Clin Res Cardiol 109(6):685–692
Lam CSP, Voors AA, de Boer RA, Solomon SD, van Veldhuisen DJ (2018) Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur Heart J 39(30):2780–2792
Zile MR, Baicu CF, Ikonomidis JS, Stroud RE, Nietert PJ, Bradshaw AD, Slater R, Palmer BM, Van Buren P, Meyer M, Redfield MM, Bull DA, Granzier HL, LeWinter MM (2015) Myocardial stiffness in patients with heart failure and a preserved ejection fraction: contributions of collagen and titin. Circulation 131(14):1247–1259
Garbern JC, Williams J, Kristl AC, Malick A, Rachmin I, Gaeta B, Ahmed N, Vujic A, Libby P, Lee RT (2019) Dysregulation of IL-33/ST2 signaling and myocardial periarteriolar fibrosis. J Mol Cell Cardiol 128:179–186
Aslan G, Polat V, Bozcali E, Opan S, Çetin N, Ural D (2019) Evaluation of serum sST2 and sCD40L values in patients with microvascular angina. Microvasc Res 122:85–93
Funding
Grant of the President of the Russian Federation MK-4257.2022.3 and Fundamental Scientific Research No. 122020300044–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no apparent or potential conflicts of interest related to the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mochula, A.V., Kopeva, K.V., Maltseva, A.N. et al. The myocardial flow reserve in patients with heart failure with preserved ejection fraction. Heart Vessels 38, 348–360 (2023). https://doi.org/10.1007/s00380-022-02161-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02161-5