Abstract
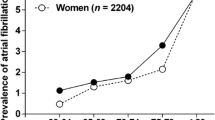
ECG screening can detect people at risk of developing atrial fibrillation (AF). Recent literature indicated that QRS transitional zone rotations could predict several cardiovascular events. Herein, we investigated the association between QRS transitional zone rotations and the future risk of AF. This prospective cohort study included 6794 participants (3178 men and 3616 women), aged 30–84 years, from the urban Japanese city of Suita. QRS transitional zone rotations were diagnosed by ECG during baseline, while AF was diagnosed by ECG, hospital records, and checkups during follow-up. The Cox regression was used to compute the sex-specified hazard ratios (HRs) and 95% confidence intervals (CIs) of incident AF for participants with counterclockwise and clockwise QRS transitional zone rotations compared to those with normal rotation. Within a median follow-up period of 14.6 years, 311 participants (206 men and 105 women) developed AF. Counterclockwise rotation was associated with the reduced risk of AF among men, but not women, in the age-adjusted model: HR (95% CI) = 0.66 (0.44, 0.98) and the multivariable-adjusted model: HR (95% CI) = 0.65 (0.43, 0.97). Clockwise rotation was not associated with AF risk in either sex. To the best of our knowledge, this is the first study to indicate that counterclockwise rotation could be associated with the reduced risk of AF in men. More studies are needed to confirm our findings and elucidate possible mechanisms.
Similar content being viewed by others
Data availability
Available upon a reasonable request.
References
Kornej J, Börschel CS, Benjamin EJ, Schnabel RB (2020) Epidemiology of atrial fibrillation in the 21st century: novel methods and new insights. Circ Res 127:4–20
Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S (2014) Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol 6:213–220
Fujisawa T, Kimura T, Kohsaka S, Ikemura N, Katsumata Y, Miyama H, Nakajima K, Nishiyama T, Aizawa Y, Kanki H, Nagami K, Fukuda K, Takatsuki S (2021) Symptom burden and treatment perception in patients with atrial fibrillation, with and without a family history of atrial fibrillation. Heart Vessel 36(2):267–276
Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M, Odutayo AA (2016) Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ 532:h7013
Ruddox V, Sandven I, Munkhaugen J, Skattebu J, Edvardsen T, Otterstad JE (2017) Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: a systematic review and meta-analysis. Eur J Prev Cardiol 24:1555–1566
He W, Chu Y (2017) Atrial fibrillation as a prognostic indicator of myocardial infarction and cardiovascular death: a systematic review and meta-analysis. Sci Rep 7:3360
Nakamura H, Niwano S, Fukaya H, Kishihara J, Satoh A, Oikawa J, Yoshizawa T, Ishizue N, Igarashi T, Fujiishi T, Nishinarita R, Horiguchi A, Ako J (2021) Fibrillation cycle length predicts cardiovascular events in patients with long-standing persistent atrial fibrillation. Heart Vessel. https://doi.org/10.1007/s00380-021-01993-x
Du X, Dong J, Ma C (2017) Is atrial fibrillation a preventable disease? J Am Coll Cardiol 69:1968–1982
Charron P, Dubourg O, Desnos M, Isnard R, Hagege A, Millaire A, Carrier L, Bonne G, Tesson F, Richard P, Bouhour JB, Schwartz K, Komajda M (1997) Diagnostic value of electrocardiography and echocardiography for familial hypertrophic cardiomyopathy in a genotyped adult population. Circulation 96:214–219
Nakai M, Watanabe M, Kokubo Y, Nishimura K, Higashiyama A, Takegami M, Nakao YM, Okamura T, Miyamoto Y (2020) Development of a cardiovascular disease risk prediction model using the Suita Study, a population-based prospective cohort study in Japan. J Atheroscler Thromb 27:1160–1175
Pinto-Filho MM, Brant LC, Dos Reis RP, Giatti L, Duncan BB, Lotufo PA, da Fonseca MJM, Mill JG, de Almeida MDCC, MacFarlane P, Barreto SM, Ribeiro ALP (2021) Prognostic value of electrocardiographic abnormalities in adults from the Brazilian longitudinal study of adults’ health. Heart 107:1560–1566
Butler HH (1973) How to read an ECG. RN 36:35–45
Rajala S, Haavisto M, Kaltiala K, Mattila K (1987) Electrocardiographic findings and 5-year cardiovascular mortality in very old people. Ann Clin Res 19:324–327
Nakamura Y, Okamura T, Higashiyama A, Watanabe M, Kadota A, Ohkubo T, Miura K, Kasagi F, Kodama K, Okayama A, Ueshima H, NIPPON DATA80 Research Group (2012) Prognostic values of clockwise and counterclockwise rotation for cardiovascular mortality in Japanese subjects: a 24-year follow-up of the national integrated project for prospective observation of noncommunicable disease and its trends in the aged, 1980-2004 (NIPPON DATA80). Circulation 125:1226–1233
Patel S, Kwak L, Agarwal SK, Tereshchenko LG, Coresh J, Soliman EZ, Matsushita K (2017) Counterclockwise and clockwise rotation of QRS transitional zone: prospective correlates of change and time-varying associations with cardiovascular outcomes. J Am Heart Assoc 6:e006281
Bradford N, Shah AJ, Usoro A, Haisty WK Jr, Soliman EZ (2015) Abnormal electrocardiographic QRS transition zone and risk of mortality in individuals free of cardiovascular disease. Europace 17:131–136
Aro AL, Eranti A, Anttonen O, Kerola T, Rissanen HA, Knekt P, Porthan K, Tikkanen JT, Junttila MJ, Huikuri HV (2014) Delayed QRS transition in the precordial leads of an electrocardiogram as a predictor of sudden cardiac death in the general population. Heart Rhythm 11:2254–2260
Arafa A, Kokubo Y, Sheerah HA, Sakai Y, Watanabe E, Li J, Honda-Kohmo K, Teramoto M, Kashima R, Koga M (2021) Weight change since age 20 and the risk of cardiovascular disease mortality: a prospective cohort study. J Atheroscler Thromb. https://doi.org/10.5551/jat.63191
Arafa A, Kokubo Y, Sheerah HA, Sakai Y, Watanabe E, Li J, Honda-Kohmo K, Teramoto M, Kashima R, Nakao YM, Koga M (2021) Developing a stroke risk prediction model using cardiovascular risk factors: the Suita Study. Cerebrovasc Dis 29:1–8. https://doi.org/10.1159/000520100
Kokubo Y, Watanabe M, Higashiyama A, Nakao YM, Kusano K, Miyamoto Y (2017) Development of a basic risk score for incident atrial fibrillation in a Japanese general population- the Suita Study. Circ J 81:1580–1588
Arafa A, Kokubo Y, Shimamoto K, Kashima R, Watanabe E, Sakai Y, Li J, Teramoto M, Sheerah HA, Kusano K (2022) Stair climbing and incident atrial fibrillation: a prospective cohort study. Environ Health Prev Med 27:10
Arafa A, Kokubo Y, Shimamoto K, Kashima R, Watanabe E, Sakai Y, Li J, Teramoto M, Sheerah HA, Kusano K (2022) Sleep duration and atrial fibrillation risk in the context of predictive, preventive, and personalized medicine: the Suita Study and meta-analysis of prospective cohort studies. EPMA J 13(1):77–86
Yanagisawa N (1981) Counterclockwise rotation of the heart; correlation of electrocardiography and chest radiography and their clinical significance. J Electrocardiol 14:233–238
Prineas RJ, Zhang ZM, Stevens CE, Soliman EZ (2018) Distribution and determinants of QRS rotation of black and white persons in the general population. J Electrocardiol 51:316–322
Seko Y, Kato T, Haruna T, Izumi T, Miyamoto S, Nakane E, Inoko M (2018) Association between atrial fibrillation, atrial enlargement, and left ventricular geometric remodeling. Sci Rep 8(1):6366
Kavousi M (2020) Differences in epidemiology and risk factors for atrial fibrillation between women and men. Front Cardiovasc Med 7:3
Magnussen C, Niiranen TJ, Ojeda FM, Gianfagna F, Blankenberg S, Njølstad I, Vartiainen E, Sans S, Pasterkamp G, Hughes M, Costanzo S, Donati MB, Jousilahti P, Linneberg A, Palosaari T, de Gaetano G, Bobak M, den Ruijter HM, Mathiesen E, Jørgensen T, Söderberg S, Kuulasmaa K, Zeller T, Iacoviello L, Salomaa V, Schnabel RB, BiomarCaRE Consortium (2017) Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts: results from the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment in Europe). Circulation 136:1588–1597
De Bacquer D, De Backer G, Kornitzer M (2000) Prevalences of ECG findings in large population based samples of men and women. Heart 84:625–633
Bolijn R, Ter Haar CC, Harskamp RE, Tan HL, Kors JA, Postema PG, Snijder MB, Peters RJG, Kunst AE, van Valkengoed IGM (2020) Do sex differences in the prevalence of ECG abnormalities vary across ethnic groups living in the Netherlands? a cross-sectional analysis of the population-based HELIUS study. BMJ Open 10:e039091
Tahara Y, Mizuno H, Ono A, Ishikawa K (1991) Evaluation of the electrocardiographic transitional zone by cardiac computed tomography. J Electrocardiol 24:239–245
Acknowledgements
We would like to thank Drs. Kawanishi and Misaki, the former and current presidents of the Suita Medical Association, respectively, and the members of Suita City Health Center. We would like to express our special gratitude to Professor Hiroyasu Iso from Osaka University, Dr. Alshimaa Mostafa from Kyoto University, and all cohort members. We also thank all researchers and staff of Preventive Cardiology and Preventive Healthcare Departments for performing medical examinations and follow-ups. This study was supported by the Intramural Research Fund (20-4-9) for the cardiovascular diseases of the National Cerebral and Cardiovascular Center, the JST Grant Number JPMJPF2018, and the Meiji Yasuda Research Institute, Inc.
Author information
Authors and Affiliations
Contributions
AA and YK (conceptualization), YK (resources), YK (funding acquisition), all authors (visualization), AA and YK (review literature), AA (draft writing), AA (data analysis), YK (supervision), and all authors (critical revision and editing).
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arafa, A., Kokubo, Y., Kobayashi, T. et al. QRS transitional zone rotations and the risk of atrial fibrillation: the Suita Study. Heart Vessels 37, 1914–1920 (2022). https://doi.org/10.1007/s00380-022-02101-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02101-3