Abstract
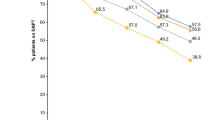
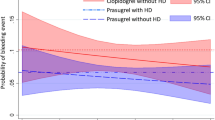
Chronic kidney disease (CKD) increases the risk of adverse outcomes in acute coronary syndrome (ACS). The optimal regimen of dual antiplatelet therapy (DAPT) post-percutaneous coronary intervention (PCI) in CKD poses a challenge due to the increased bleeding and clotting tendencies, particularly since patients with CKD were underrepresented in randomized controlled trials. We examined the practice patterns of DAPT prescription stratified by the presence of CKD. The multicentre prospective Canadian Observational Antiplatelet Study (COAPT) enrolled patients with ACS between December 2011 and May 2013. The present study is a subgroup analysis comparing type and duration of DAPT and associated outcomes among patients with and without CKD (eGFR < 60 ml/min/1.73 m2, calculated by CKD-EPI). Patients with CKD (275/1921, 14.3%) were prescribed prasugrel/ticagrelor less (18.5% vs 25.8%, p = 0.01) and had a shorter duration of DAPT therapy versus patients without CKD (median 382 vs 402 days, p = 0.003). CKD was associated with major adverse cardiovascular events (MACE) at 12 months (p < 0.001) but not bleeding when compared to patients without CKD. CKD was associated with MACE in both patients on prasugrel/ticagrelor (p = 0.017) and those on clopidogrel (p < 0.001) (p for heterogeneity = 0.70). CKD was associated with increased bleeding only among patients receiving prasugrel/ticagrelor (p = 0.007), but not among those receiving clopidogrel (p = 0.64) (p for heterogeneity = 0.036). Patients with CKD had a shorter DAPT duration and were less frequently prescribed potent P2Y12 inhibitors than patients without CKD. Overall, compared with patients without CKD, patients with CKD had higher rates of MACE and similar bleeding rates. However, among those prescribed more potent P2Y12 inhibitors, CKD was associated with more bleeding than those without CKD. Further studies are needed to better define the benefit/risk evaluation, and establish a more tailored and evidence-based DAPT regimen for this high-risk patient group.

Similar content being viewed by others
References
GBD Chronic Kidney Disease Collaboration (2020) Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395(10225):709–733
Dumaine RL, Montalescot G, Steg PG, Ohman EM, Eagle K, Bhatt DL, REACH Registry Investigators (2009) Renal function, atherothrombosis extent, and outcomes in high-risk patients. Am Heart J 158(1):141–148.e1
Baber U, Chandrasekhar J, Sartori S, Aquino M, Kini AS, Kapadia S, Weintraub W, Muhlestein JB, Vogel B, Faggioni M (2017) Associations between chronic kidney disease and outcomes with use of prasugrel versus clopidogrel in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a report from the PROMETHEUS study. JACC Cardiovasc Interv 10(20):2017–2025
Baber U, Mehran R, Kirtane AJ, Gurbel PA, Christodoulidis G, Maehara A, Witzenbichler B, Weisz G, Rinaldi MJ, Metzger DC (2015) Prevalence and impact of high platelet reactivity in chronic kidney disease: results from the assessment of dual antiplatelet therapy with drug-eluting stents registry. Circ Cardiovasc Interv 8(6):e001683
Tomaniak M, Chichareon P, Klimczak-Tomaniak D, Takahashi K, Kogame N, Modolo R, Wang R, Ono M, Hara H, Gao C (2020) Impact of renal function on clinical outcomes after PCI in ACS and stable CAD patients treated with ticagrelor: a prespecified analysis of the GLOBAL LEADERS randomized clinical trial. Clin Res Cardiol 109(7):930–943
Htun P, Fateh-Moghadam S, Bischofs C, Banya W, Müller K, Bigalke B, Stellos K, May AE, Flather M, Gawaz M (2011) Low responsiveness to clopidogrel increases risk among CKD patients undergoing coronary intervention. J Am Soc Nephrol 22(4):627–633
Mehta SR, Bainey KR, Cantor WJ, Lordkipanidzé M, Marquis-Gravel G, Robinson SD, Sibbald M, So DY, Wong GC, Abunassar JG (2018) 2018 Canadian Cardiovascular Society/Canadian association of interventional cardiology focused update of the guidelines for the use of antiplatelet therapy. Can J Cardiol 34(3):214–233
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L (2016) 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 68(10):1082–1115
Sra S, Tan MK, Mehta SR, Fisher HN, Déry J-P, Welsh RC, Eisenberg MJ, Overgaard CB, Rose BF, Della Siega AJ (2016) Ischemic and bleeding events in patients with myocardial infarction undergoing percutaneous coronary intervention who require oral anticoagulation: Insights from the Canadian observational AntiPlatelet sTudy. Am Heart J 180:82–89
Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Fox KA, Dabbous OH, Goldberg RJ, Pieper KS, Eagle KA, Van de Werf F, Avezum Á, Goodman SG, Flather MD, Anderson FA Jr, Granger C (2006) Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 333(7578):1091
Moscucci M, Fox KA, Cannon CP, Klein W, López-Sendón J, Montalescot G, White K, Goldberg RJ (2003) Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 24(20):1815–1823
Marx N, Noels H, Jankowski J, Floege J, Fliser D, Böhm M (2018) Mechanisms of cardiovascular complications in chronic kidney disease: research focus of the Transregional Research Consortium SFB TRR219 of the University Hospital Aachen (RWTH) and the Saarland University. Clin Res Cardiol 107(2):120–126
Bonello L, Angiolillo DJ, Aradi D, Sibbing D (2018) P2Y12-ADP receptor blockade in chronic kidney disease patients with acute coronary syndromes: review of the current evidence. Circulation 138(15):1582–1596
Angiolillo DJ, Bernardo E, Capodanno D, Vivas D, Sabaté M, Ferreiro JL, Ueno M, Jimenez-Quevedo P, Alfonso F, Bass TA (2010) Impact of chronic kidney disease on platelet function profiles in diabetes mellitus patients with coronary artery disease taking dual antiplatelet therapy. J Am Coll Cardiol 55(11):1139–1146
Morel O, El Ghannudi S, Jesel L, Radulescu B, Meyer N, Wiesel M-L, Caillard S, Campia U, Moulin B, Gachet C (2011) Cardiovascular mortality in chronic kidney disease patients undergoing percutaneous coronary intervention is mainly related to impaired P2Y12 inhibition by clopidogrel. J Am Coll Cardiol 57(4):399–408
Stone GW, Witzenbichler B, Weisz G, Rinaldi MJ, Neumann F-J, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri E (2013) Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet 382(9892):614–623
Baber U, Mehran R, Giustino G, Cohen DJ, Henry TD, Sartori S, Ariti C, Litherland C, Dangas G, Gibson CM (2016) Coronary thrombosis and major bleeding after PCI with drug-eluting stents: risk scores from PARIS. J Am Coll Cardiol 67(19):2224–2234
Palmer SC, Di Micco L, Razavian M, Craig JC, Perkovic V, Pellegrini F, Copetti M, Graziano G, Tognoni G, Jardine M (2012) Effects of antiplatelet therapy on mortality and cardiovascular and bleeding outcomes in persons with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med 156(6):445–459
Rymer JA, Kaltenbach LA, Doll JA, Messenger JC, Peterson ED, Wang TY (2019) Safety of dual‐antiplatelet therapy after myocardial infarction among patients with chronic kidney disease. J Am Heart Assoc 8(10):e012236
Baber U, Li SX, Pinnelas R, Pocock SJ, Krucoff MW, Ariti C, Gibson CM, Steg PG, Weisz G, Witzenbichler B (2018) Incidence, patterns, and impact of dual antiplatelet therapy cessation among patients with and without chronic kidney disease undergoing percutaneous coronary intervention: results from the PARIS Registry (Patterns of Non-Adherence to Anti-Platelet Regimens in Stented Patients). Circ: Cardiovasc Interv 11(3):e006144
Ocak G, Rookmaaker M, Algra A, De Borst G, Doevendans P, Kappelle L, Verhaar M, Visseren F, Group SS, van der Graaf Y (2018) Chronic kidney disease and bleeding risk in patients at high cardiovascular risk: a cohort study. J Thromb Haemost 16(1):65-73
Costa F, van Klaveren D, James S, Heg D, Räber L, Feres F, Pilgrim T, Hong M-K, Kim H-S, Colombo A (2017) Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 389(10073):1025–1034
Yeh RW, Secemsky EA, Kereiakes DJ, Normand S-LT, Gershlick AH, Cohen DJ, Spertus JA, Steg PG, Cutlip DE, Rinaldi MJ (2016) Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention. JAMA 315(16):1735–1749
Mavrakanas TA, Chatzizisis YS, Gariani K, Kereiakes DJ, Gargiulo G, Helft G, Gilard M, Feres F, Costa RA, Morice M-C (2019) Duration of dual antiplatelet therapy in patients with CKD and drug-eluting stents: a meta-analysis. J Am Soc Nephrol 14(6):810–822
Hwang D, Park KW, Lee JM, Rhee T-M, Hong M-K, Jang Y, Valgimigli M, Colombo A, Gilard M, Palmerini T (2018) Efficacy and safety of dual antiplatelet therapy after coronary stenting in patients with chronic kidney disease. Am Heart J 197:103–112
Montalescot G, Brieger D, Dalby AJ, Park S-J, Mehran R (2015) Duration of dual antiplatelet therapy after coronary stenting: a review of the evidence. J Am Coll Cardiol 66(7):832–847
O’Donoghue ML, Murphy SA, Sabatine MS (2020) The safety and efficacy of aspirin discontinuation on a background of a P2Y12 inhibitor in patients after percutaneous coronary intervention: a systematic review and meta-analysis. Circulation 142(6):538–545
Yan AT, Yan RT, Tan M, Huynh T, Soghrati K, Brunner LJ, DeYoung P, Fitchett DH, Langer A, Goodman SG (2007) Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1-year outcome. Am Heart J 154(6):1108–1115
Laine M, Lemesle G, Burley S, Cayla G, Range G, Quaino G, Canault M, Pankert M, Paganelli F, Puymirat E, Bonello L (2020) TicagRelor or Clopidogrel in severe or terminal chronic kidney patients undergoing PERcutaneous coronary intervention for acute coronary syndrome: the TROUPER trial. Am Heart J 225:19–26
Acknowledgements
The authors acknowledge editorial assistance by Sue Francis.
Funding
The COAPT study was sponsored by Eli Lilly and Daiichi Sankyo.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Graham, C.A., Tan, M.K., Chew, D.P. et al. Use and outcomes of dual antiplatelet therapy for acute coronary syndrome in patients with chronic kidney disease: insights from the Canadian Observational Antiplatelet Study (COAPT). Heart Vessels 37, 1291–1298 (2022). https://doi.org/10.1007/s00380-022-02029-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02029-8