Abstract
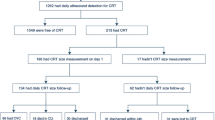
Central venous catheters (CVCs) and pulmonary artery catheters (PACs) are widely used in intensive care and perioperative management. The detection and prevention of catheter-related thrombosis (CRT) are important because CRT is a complication of catheter use and can cause pulmonary embolism and bloodstream infection. Currently, there is no evidence for CRT in patients using both CVC and PAC. We conducted a single-center, prospective, observational study to identify the incidence, timing, and risk factors for CRT in patients undergoing cardiovascular surgery and using a combination of CVC and PAC through the right internal jugular vein (RIJV). Out of 50 patients, CRT was observed using ultrasonography in 39 patients (78%), and the median time of CRT formation was 1 day (interquartile range: 1–1.5) after catheter insertion. The mean duration of PAC placement was 3 days (interquartile range: 2–5), and the maximum diameter of CRT was 12 mm (interquartile range: 10–15). In short-axis images, CRT occupied more than half of the cross-sectional area of the RIJV in five patients (10%), and CRT completely occluded the RIJV in one patient (2%). Platelet count, duration of PAC placement, and intraoperative bleeding amount were found to be high-risk indicators of CRT. In conclusion, patients who underwent cardiovascular surgery and using both CVC and PAC had a high incidence of CRT. Avoiding unnecessary PAC placement and early removal of catheters in patients at high risk of developing CRT may prevent the development of CRT.


Similar content being viewed by others
References
Timsit JF, Farkas JC, Boyer JM, Martin JB, Misset B, Renaud B, Carlet J (1998) Central vein catheter-related thrombosis in intensive care patients: incidence, risks factors, and relationship with catheter-related sepsis. Chest 114:207–213
Trerotola SO, Stavropoulos SW, Mondschein JI, Patel AA, Fishman N, Fuchs B, Kolansky DM, Kasner S, Pryor J, Chittams J (2010) Triple-lumen peripherally inserted central catheter in patients in the critical care unit: prospective evaluation. Radiology 256:312–320
Oh CS, Rhee KY, Yoon TG, Kim SH (2016) Assessment of thrombosis in right internal jugular vein after percutaneous superior vena cava catheter insertion during cardiovascular surgery with cardiopulmonary bypass. J Thorac Cardiovasc Surg 152:1592–1599
Chen PT, Chang KC, Hu KL, Ting CK, Chan KH, Chang WK (2017) Catheter-related right internal jugular vein thrombosis after chest surgery. Br J Anaesth 119:192–199
Geerts W (2014) Central venous catheter-related thrombosis. Hematology Am Soc Hematol Educ Program 2014:306–311
Judge O, Ji F, Fleming N, Liu H (2015) Current use of the pulmonary artery catheter in cardiac surgery: a survey study. J Cardiothorac Vasc Anesth 29:69–75
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, Davila-Roman VG, Gerhard-Herman MD, Holly TA, Kane GC, Marine JE, Nelson MT, Spencer CC, Thompson A, Ting HH, Uretsky BF, Wijeysundera DN (2014) 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130:2215–2245
Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, DiSesa VJ, Hiratzka LF, Hutter AM Jr, Jessen ME, Keeley EC, Lahey SJ, LangeRA LMJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD, Jacobs AK, Anderson JL, Albert N, Creager MA, Ettinger SM, Guyton RA, Halperin JL, Hochman JS, Kushner FG, Ohman EM, Stevenson W, Yancy CW, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines (2012) 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 143:4–34
Bossert T, Gummert JF, Bittner HB, Barten M, Walther T, Falk V, Mohr FW (2006) Swan-Ganz catheter-induced severe complications in cardiac surgery: right ventricular perforation, knotting, and rupture of a pulmonary artery. J Card Surg 21:292–295
Sato D, Ikeda S, Koga S, Yamagata Y, Eguchi M, Yonekura T, Tsuneto A, Yoshimuta T, Koide Y, Kawano H, Maemura K (2019) Effectiveness and safety of oral direct factor Xa inhibitors for the treatment of venous thromboembolism in patients with cancer and/or older age. Heart Vessels 34:678–687
Keller K, Hobohm L, Engelhardt M (2019) Risk of venous thromboembolism after endoprosthetic surgeries: lower versus upper extremity endoprosthetic surgeries. Heart Vessels 34:815–823
Schwann NM, Hillel Z, Hoeft A, Barash P, Möhnle P, Miao Y, Mangano DT (2011) Lack of effectiveness of the pulmonary artery catheter in cardiac surgery. Anesth Analg 113:994–1002
Barone JE, Tucker JB, Rassias D, Corvo PR (2001) Routine perioperative pulmonary artery catheterization has no effect on rate of complications in vascular surgery: a meta-analysis. Am Surg 67:674–679
Shah MR, Hasselblad V, Stevenson LW, Binanay C, O’Connor CM, Sopko G, Califf RM (2005) Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA 294:1664–1670
Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K, PAC-Man study collaboration (2005) Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC Man): a randomised controlled trial. Lancet 366:472–477
Acknowledgements
We sincerely thank the medical staff at the ICU of the Tokyo Women’s Medical University Hospital for data collection and their helpful advice. We would like to thank Editage (www.editage.com) for support of statistical analysis and English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Idei, M., Seino, Y., Sato, N. et al. Catheter-related thrombosis after cardiac surgery in patients with both central venous and pulmonary artery catheters inserted into the right internal jugular vein: a single-center, prospective, observational study. Heart Vessels 37, 691–696 (2022). https://doi.org/10.1007/s00380-021-01955-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01955-3