Abstract
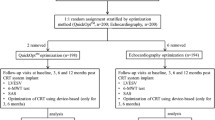
Heart rate modulation therapy using ivabradine reduces mortality and morbidity in patients with systolic heart failure, whereas too reduced heart rate seems to worsen the clinical outcome. The optimal heart rate during heart rate modulation therapy remains unknown. Consecutive patients with left ventricular ejection fraction < 50% who received echocardiographic assessments and simultaneous heart rate measurements were retrospectively investigated. Theoretically ideal heart rate was calculated using a previously proposed formula: 93 − 0.13 × (deceleration time [msec]). Impacts of heart rate on the 1-year echocardiographic left ventricular reverse remodeling were compared among the three groups stratified by the heart rate status: optimal heart rate group (within 10 bpm of ideal heart rate), below-optimal heart rate group (< 10 bpm of ideal heart rate), and above-optimal heart rate group (> 10 bpm of ideal heart rate). A total of 75 patients (70 years old, 60 men) were included. There were no significant differences in the baseline characteristics among the three groups, except for the higher prevalence of tolvaptan use and higher plasma B-type natriuretic peptide level in the below-optimal heart rate group. Left ventricular end-diastolic diameter (from 55 to 54) and left ventricular ejection fraction (from 39 to 46) improved significantly only in the optimal heart rate group at 1-year follow-up (p < 0.05 for both). Optimal heart rate, which was calculated using a formula consisting of deceleration time, was associated with cardiac reverse remodeling in patients with systolic heart failure. Prospective study to investigate the implication of deceleration time-guided aggressive heart rate optimization is the next concern.


Similar content being viewed by others
References
Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L, Investigators SHIFT (2010) Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 376(9744):875–885
Koruth JS, Lala A, Pinney S, Reddy VY, Dukkipati SR (2017) The clinical use of ivabradine. J Am Coll Cardiol 70(14):1777–1784
Fiuzat M, Wojdyla D, Pina I, Adams K, Whellan D, O’Connor CM (2016) Heart rate or beta-blocker dose? Association with outcomes in ambulatory heart failure patients with systolic dysfunction: results from the HF-ACTION trial. JACC Heart Fail 4(2):109–115
Izumida T, Imamura T, Nakamura M, Fukuda N, Kinugawa K (2020) How to consider target heart rate in patients with systolic heart failure. ESC Heart Fail 7(5):3231–3234
Gardin JM, Adams DB, Douglas PS, Feigenbaum H, Forst DH, Fraser AG, Grayburn PA, Katz AS, Keller AM, Kerber RE, Khandheria BK, Klein AL, Lang RM, Pierard LA, Quinones MA, Schnittger I, American Society of Echocardiography (2002) Recommendations for a standardized report for adult transthoracic echocardiography: a report from the American Society of Echocardiography’s Nomenclature and Standards Committee and Task Force for a Standardized Echocardiography Report. J Am Soc Echocardiogr 15(3):275–290
Dandel M, Hetzer R (2021) Ventricular systolic dysfunction with and without altered myocardial contractility: clinical value of echocardiography for diagnosis and therapeutic decision-making. Int J Cardiol 327:236–250
Koitabashi N, Kass DA (2011) Reverse remodeling in heart failure–mechanisms and therapeutic opportunities. Nat Rev Cardiol 9(3):147–157
Maurer MS, Sackner-Bernstein JD, El-Khoury Rumbarger L, Yushak M, King DL, Burkhoff D (2009) Mechanisms underlying improvements in ejection fraction with carvedilol in heart failure. Circ Heart Fail 2(3):189–196
Chung CS, Afonso L (2016) Heart rate is an important consideration for cardiac imaging of diastolic function. JACC Cardiovasc Imaging 9(6):756–758
Chung CS, Kovács SJ (2006) Consequences of increasing heart rate on deceleration time, the velocity-time integral, and E/A. Am J Cardiol 97(1):130–136
Yamanaka T, Onishi K, Tanabe M, Dohi K, Funabiki-Yamanaka K, Fujimoto N, Kurita T, Tanigawa T, Kitamura T, Ito M, Nobori T, Nakano T (2006) Force- and relaxation-frequency relations in patients with diastolic heart failure. Am Heart J 152(5):966.e1–7
Dandel M, Hetzer R (2018) Recovery of failing hearts by mechanical unloading: pathophysiologic insights and clinical relevance. Am Heart J 206:30–50
Fu X, Segiser A, Carrel TP, Tevaearai Stahel HT, Most H (2016) Rat heterotopic heart transplantation model to investigate unloading-induced myocardial remodeling. Front Cardiovasc Med 3:34
Takada T, Sakata Y, Miyata S, Takahashi J, Nochioka K, Miura M, Tadaki S, Shimokawa H, CHART-2 Investigators (2014) Impact of elevated heart rate on clinical outcomes in patients with heart failure with reduced and preserved ejection fraction: a report from the CHART-2 Study. Eur J Heart Fail 16(3):309–316
DeVore AD, Schulte PJ, Mentz RJ, Hardy NC, Kelly JP, Velazquez EJ, Maya JF, Kielhorn A, Patel HK, Reed SD, Hernandez AF (2016) Relation of elevated heart rate in patients with heart failure with reduced ejection fraction to one-year outcomes and costs. Am J Cardiol 117(6):946–951
Li SJ, Sartipy U, Lund LH, Dahlström U, Adiels M, Petzold M, Fu M (2015) Prognostic Significance of resting heart rate and use of beta-blockers in atrial fibrillation and sinus rhythm in patients with heart failure and reduced ejection fraction: findings from the Swedish Heart Failure Registry. Circ Heart Fail 8(5):871–879
Ferrari R, Fox K (2016) Heart rate reduction in coronary artery disease and heart failure. Nat Rev Cardiol 13(8):493–501
Nikolovska Vukadinović A, Vukadinović D, Borer J, Cowie M, Komajda M, Lainscak M, Swedberg K, Böhm M (2017) Heart rate and its reduction in chronic heart failure and beyond. Eur J Heart Fail 19(10):1230–1241
Ibrahim NE, Gaggin HK, Turchin A, Patel HK, Song Y, Trebnick A, Doros G, Maya JF, Cannon CP, Januzzi JL (2019) Heart rate, beta-blocker use, and outcomes of heart failure with reduced ejection fraction. Eur Heart J Cardiovasc Pharmacother 5(1):3–11
Acknowledgements
None.
Funding
TI receives grant support from JSPS KAKENHI: JP20K17143.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Izumida, T., Imamura, T., Ueno, Y. et al. Impact of optimal heart rate on left ventricular reverse remodeling and functional improvement in patients with systolic heart failure. Heart Vessels 36, 1688–1693 (2021). https://doi.org/10.1007/s00380-021-01864-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01864-5