Abstract
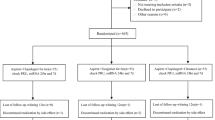
Platelet functions are thought to contribute to clinical outcomes after heart surgery. This study was conducted to assess the pivotal roles of vascular endothelial growth factor-A (VEGF-A) and microRNA-126 (miR-126) during coronary artery bypass grafting (CABG). Whole blood was collected for platelet isolation from 67 patients who underwent CABG surgery between July 2013 and March 2014. VEGF-A and miR-126 levels in serum, plasma, and platelets were measured at various time points and compared with clinical characteristics. The platelet count was decreased at 3 days after CABG. This dynamic change in platelet count was larger after conventional coronary artery bypass (CCAB) than off-pump coronary artery bypass (OPCAB). VEGF-A in the same number of platelets (IP-VEGF-A) was increased at 3 days after CABG, followed by an increase of VEGF-A in serum (S-VEGF-A) at 7 days after surgery. The miR-126-3p level in serum (S-miR-126-3p) increased rapidly after CABG and then decreased below preoperative levels. The IP-VEGF-A level on day 7 after CABG in patients with peripheral artery disease (PAD), who suffered from endothelial dysfunction, was higher compared with patients without PAD. Conversely, S-miR-126-3p on day 7 after surgery was lower in patients with PAD than in patients without PAD. Low levels of S-miR-126-3p due to endothelial dysfunction may lead to high IP-VEGF-A, which is closely related to complications after CABG.







Similar content being viewed by others
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- VEGF-A:
-
Vascular endothelial growth factor-A
- IP-VEGF-A:
-
Intra-platelet vascular endothelial growth factor-A
- S-VEGF-A:
-
Serum vascular endothelial growth factor-A
- IP-miR-126:
-
Intra-platelet miR-126
- IL-6:
-
Interleukin-6
- TPO:
-
Thrombopoietin
References
Piccolo R, Giustino G, Mehran R, Windecker S (2015) Stable coronary artery disease: revascularisation and invasive strategies. Lancet 386(9994):702–713
Gukop P, Gutman N, Bilkhu R, Karapanagiotidis GT (2014) Who might benefit from early aspirin after coronary artery surgery? Interact Cardiovasc Thorac Surg 19(3):505–511
Gross L, Sibbing D (2017) Current role of platelet function testing in percutaneous coronary intervention and coronary artery bypass grafting. Interv Cardiol Clin 6(1):151–166
Furie B, Furie BC (2008) Mechanisms of thrombus formation. N Engl J Med 359(9):938–949
Lowenstein CJ, Morrell CN, Yamakuchi M (2005) Regulation of Weibel-Palade body exocytosis. Trends Cardiovasc Med 15(8):302–308
Morrell CN, Matsushita K, Chiles K, Scharpf RB, Yamakuchi M, Mason RJ, Bergmeier W, Mankowski JL, Baldwin WM 3rd, Faraday N, Lowenstein CJ (2005) Regulation of platelet granule exocytosis by S-nitrosylation. Proc Natl Acad Sci USA 102(10):3782–3787
Arisato T, Hashiguchi T, Sarker KP, Arimura K, Asano M, Matsuo K, Osame M, Maruyama I (2003) Highly accumulated platelet vascular endothelial growth factor in coagulant thrombotic region. J Thromb Haemost 1(12):2589–2593
Ferrara N (2009) Vascular endothelial growth factor. Arterioscler Thromb Vasc Biol 29(6):789–791
Hashiguchi T, Arimura K, Matsumuro K, Otsuka R, Watanabe O, Jonosono M, Maruyama Y, Maruyama I, Osame M (2000) Highly concentrated vascular endothelial growth factor in platelets in Crow-Fukase syndrome. Muscle Nerve 23(7):1051–1056
Aryal B, Shimizu T, Kadono J, Furoi A, Komokata T, Inoue M, Ikeda S, Fukukura Y, Nakamura M, Yamakuchi M, Hashiguchi T, Imoto Y (2016) A switch in the dynamics of intra-platelet vegf-a from cancer to the later phase of liver regeneration after partial hepatectomy in humans. PLoS ONE 11(3):e0150446
Ambros V (2004) The functions of animal microRNAs. Nature 431(7006):350–355
Small EM, Frost RJ, Olson EN (2010) MicroRNAs add a new dimension to cardiovascular disease. Circulation 121(8):1022–1032
Harris TA, Yamakuchi M, Ferlito M, Mendell JT, Lowenstein CJ (2008) MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc Natl Acad Sci USA 105(5):1516–1521
Wang S, Aurora AB, Johnson BA, Qi X, McAnally J, Hill JA, Richardson JA, Bassel-Duby R, Olson EN (2008) The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell 15(2):261–271
Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, Ivey KN, Bruneau BG, Stainier DY, Srivastava D (2008) miR-126 regulates angiogenic signaling and vascular integrity. Dev Cell 15(2):272–284
Qu M, Pan J, Wang L, Zhou P, Song Y, Wang S, Jiang L, Geng J, Zhang Z, Wang Y, Tang Y, Yang GY (2019) MicroRNA-126 regulates angiogenesis and neurogenesis in a mouse model of focal cerebral ischemia. Mol Ther Nucleic Acids 16:15–25
Pereira-da-Silva T, Coutinho Cruz M, Carrusca C, Cruz Ferreira R, Napoleao P, Mota Carmo M (2018) Circulating microRNA profiles in different arterial territories of stable atherosclerotic disease: a systematic review. Am J Cardiovasc Dis 8(1):1–13
He Y, Zhong J, Huang S, Shui X, Kong D, Chen C, Lei W (2017) Elevated circulating miR-126-3p expression in patients with acute myocardial infarction: its diagnostic value. Int J Clin Exp Pathol 10(11):11051–11056
Yamakuchi M (2012) MicroRNAs in Vascular Biology. Int J Vasc Med 2012:794898
Avci E, Kiris T, Celik A, Varis E, Esin FK, Koprulu D, Kadi H (2018) Prognostic value of rising mean platelet volume during hospitalization in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. BMC Cardiovasc Disord 18(1):226
Etulain J, Fondevila C, Negrotto S, Schattner M (2013) Platelet-mediated angiogenesis is independent of VEGF and fully inhibited by aspirin. Br J Pharmacol 170(2):255–265
Mangano DT, Multicenter Study of Perioperative Ischemia Research G (2002) Aspirin and mortality from coronary bypass surgery. N Engl J Med 347(17):1309–1317
Podemska-Jedrzejczak Z, Malinska A, Sujka-Kordowska P, Nowicki M, Puslecki M, Jemielity M, Perek B (2018) Vascular restenosis in coronary artery bypass grafting might be associated with VEGF-C/VEGFR-3 signaling pathway. Heart Vessels 33(9):1106–1120
Kusumanto YH, Tio RA, Loef BG, Sluiter WJ, Mulder NH, Hospers GA (2006) Systemic VEGF levels after coronary artery bypass graft surgery reflects the extent of inflammatory response. Acute Card Care 8(1):41–45
Namino F, Yamakuchi M, Iriki Y, Okui H, Ichiki H, Maenosono R, Oketani N, Masamoto I, Miyata M, Horiuchi M, Hashiguchi T, Ohishi M, Maruyama I (2019) Dynamics of soluble thrombomodulin and circulating miRNAs in patients with atrial fibrillation undergoing radiofrequency catheter ablation. Clin Appl Thromb Hemost 25:1076029619851570
Wang Z, Li X, Shen J, Tian D, Ji Q, Xia L, Lv Q (2018) Plasma microRNAs reflecting cardiac and inflammatory injury in coronary artery bypass grafting surgery. J Surg Res 224:58–63
Yuan Y, Shen C, Zhao SL, Hu YJ, Song Y, Zhong QJ (2019) MicroRNA-126 affects cell apoptosis, proliferation, cell cycle and modulates VEGF/TGF-beta levels in pulmonary artery endothelial cells. Eur Rev Med Pharmacol Sci 23(7):3058–3069
Acknowledgements
We thank Dr. Toshiaki Shimizu for useful discussions and Ms. Nobue Uto for technical assistance. We thank Mitchell Arico from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript.
Funding
This study was supported by Challenging Research (Exploratory) (18K19523) (MY), Grants-in-Aid for Scientific Research (18H02734) (MY), (16H05229) (TH), (19K09274) (YI), (20K09130) (HK), and (20K07852) (YO), and Grants-in Aid for Early career scientists (20K16553) (KT) and (20K16527) (TK).
Author information
Authors and Affiliations
Contributions
KM, MY and HK designed and performed all the experiments, analyzed data, and wrote the manuscript. YS, KA, KM, KT, YO and TK partially performed the experiments. TH and YI supervised all the experiments. All authors discussed the design and the results.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mukaihara, K., Yamakuchi, M., Kanda, H. et al. Evaluation of VEGF-A in platelet and microRNA-126 in serum after coronary artery bypass grafting. Heart Vessels 36, 1635–1645 (2021). https://doi.org/10.1007/s00380-021-01855-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01855-6