Abstract
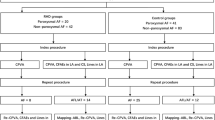
Atrial fibrillation (AF) is a common disease that changes cardiac morphology, especially in the left atrium (LA). It is now known that certain categories of functional mitral regurgitation (MR) are associated with AF; however, the influence of AF on right cardiac morphology is not fully understood. Our aim in this study was to investigate the association between AF and right cardiac morphology. This was a retrospective cohort study of 86 patients with persistent AF without other cardiac disease who underwent catheter ablation (CA). Seventy-one patients had sustained sinus rhythm (SR) (SR Group) and 15 patients had sustained AF (AF Group) during the study period. We compared the changes in the right cardiac dimensions and tricuspid regurgitation (TR) between the groups 12 months after CA. Patients’ baseline echocardiographic assessments revealed that the LA volume index was significantly smaller in the SR group than in the AF group (46.8 ± 11.9 ml/m2 vs 59.3 ± 12.8 ml/m2, respectively; p < 0.01). Comparing baseline data with the 12-month follow-up data, in the SR group, right atrial area (RAA, cm2), tricuspid annular diameter (mm), and tricuspid regurgitant jet area (cm2) were significantly decreased compared with the AF group (19.5 ± 4.5–15.5 ± 3.6 vs 20.7 ± 3.6–19.7 ± 2.3; 30.5 ± 4.9–26.4 ± 3.9 vs 28.7 ± 4.0–28.8 ± 3.1; and 1.4 [interquartile range (IQR) 0.7–2.6]–0.6 [IQR 0.2–1.2] vs 1.2 [IQR 1.1–1.5]–0.9 [IQR 0.4–1.3], respectively). On multivariate analysis, change in RAA correlated with the reduction in tricuspid regurgitant jet area (R = 0.51, p < 0.001). In conclusion, successful CA for persistent AF led to right heart reverse remodeling, and our findings suggested that persistent AF was associated with RAA dilatation and TR.




Similar content being viewed by others
References
Magnani JW, Rienstra M, Lin H, Sinner MF, Lubitz SA, McManus DD, Dupuis J, Ellinor PT, Benjamin EJ (2011) Atrial fibrillation. Circulation 124:1982–1993
Inoue H, Fujiki A, Origasa H, Ogawa S, Okumura K, Kubota I, Aizawa Y, Yamashita T, Atarashi H, Horie M, Ohe T, Doi Y, Shimizu A, Chishaki A, Saikawa T, Yano K, Kitabatake A, Mitamura H, Kodama I, Kamakura S (2009) Prevalence of atrial fibrillation in the general population of Japan: An analysis based on periodic health examination. Int J Cardiol 137:102–107
The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Investigators (2002) A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 347:1825–1833
Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, Said SA, Darmanata JI, Timmermans AJ, Tijssen JG, Crijns HJ (2002) A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med 347:1834–1840
Gertz ZM, Raina A, Saghy L, Zado ES, Callans DJ, Marchlinski FE, Keane MG, Silvestry FE (2011) Evidence of atrial functional mitral regurgitation due to atrial fibrillation reversal with arrhythmia control. J Am Coll Cardiol 58(14):1474–1481
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, Hahn RT, Han Y, Hung J, Lang RM, Little SH, Shah DJ, Shernan S, Thavendiranathan P, Thomas JD, Weissman NJ (2017) Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the american society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J Am Soc Echocardiogr 30(4):303–371
Mutlak D, Lessick J, Reisner SA, Aronson D, Dabbah S, Agmon Y (2007) Echocardiography-based spectrum of severe tricuspid regurgitation: the frequency of apparently idiopathic tricuspid regurgitation. J Am Soc Echocardiogr 20(4):405–408
Ong K, Yu G, Jue J (2014) Prevalence and spectrum of conditions associated with severe tricuspid regurgitation. Echocardiography 31:558–562
Utsunomiya H, Itabashi Y, Mihara H, Berdejo J, Kobayashi S, Siegel RJ, Shiota T (2017) Functional tricuspid regurgitation caused by chronic atrial fibrillation: a real-time 3-dimensional transesophageal echocardiography study. Circ Cardiovasc Imaging 10:e004897
Shiran A, Najjar R, Adawi S, Aronson D (2014) Risk factors for progression of functional tricuspid regurgitation. Am J Cardiol 113:995–1000
Najib MQ, Vittala SS, Challa S, Raizada A, Tondato FJ, Lee HR, Chaliki HP (2013) Predictors of severe tricuspid regurgitation in patients with permanent pacemaker or automatic implantable cardioverter-defibrillator leads. Texas Hear Inst J 40:529–533
Topilsky Y, Nkomo VT, Vatury O, Michelena HI, Letourneau T, Suri RM, Pislaru S, Park S, Mahoney DW, Biner S, Enriquez-Sarano M (2014) Clinical outcome of isolated tricuspid regurgitation. JACC Cardiovasc Imaging 7:1185–1194
Topilsky Y, Inojosa JM, Benfari G, Vaturi O, Maltais S, Michelena H, Mankad S, Enriquez-Sarano M (2018) Clinical presentation and outcome of tricuspid regurgitation in patients with systolic dysfunction. Eur Heart J 39:3584–3592
Lindman BR, Maniar HS, Jaber WA, Lerakis S, Mack MJ, Suri RM, Thourani VH, Babaliaros V, Kereiakes DJ, Whisenant B, Miller DC, Tuzcu EM, Svensson LG, Xu K, Doshi D, Leon MB, Zajarias A (2015) Effect of tricuspid regurgitation and the right heart on survival after transcatheter aortic valve replacement. Circ Cardiovasc Interv 8:e002073
Chen L, Larsen CM, Le RJ, Connolly HM, Pislaru SV, Murphy JG, McGoon MD, Frantz RP, Kane GC (2018) The prognostic significance of tricuspid valve regurgitation in pulmonary arterial hypertension. Clin Respir J 12:1572–1580
Varadarajan P, Pai RG (2010) Tricuspid regurgitation in patients with severe mitral regurgitation and normal left ventricular ejection fraction: risk factors and prognostic implications in a cohort of 895 patients. J Heart Valve Dis 19:412–419
Nath J, Foster E, Heidenreich PA (2004) Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol 43:405–409
Fender EA, Petrescu I, Ionescu F, Zack CJ, Pislaru SV, Nkomo VT, Cochuyt JJ, Hodge DO, Nishimura RA (2019) prognostic importance and predictors of survival in isolated tricuspid regurgitation: a growing problem. Mayo Clin Proc. https://doi.org/10.1016/j.mayocp.2019.04.036
Lee J-W, Song J-M, Park JP, Lee JW, Kang DH, Song JK (2010) Long-term prognosis of isolated significant tricuspid regurgitation. Circ J 74:375–380
Barbanti M, Binder RK, Dvir D, Tan J, Freeman M, Thompson CR, Cheung A, Wood DA, Leipsic J, Webb JG (2015) Prevalence and impact of preoperative moderate/severe tricuspid regurgitation on patients undergoing transcatheter aortic valve replacement. Catheter Cardiovasc Interv 85:677–684
Topilsky Y, Khanna A, Le Tourneau T, Park S, Michelena H, Suri R, Mahoney DW, Enriquez-Sarano M (2012) Clinical context and mechanism of functional tricuspid regurgitation in patients with and without pulmonary hypertension. Circ Cardiovasc Imaging 5(3):314–323
Koelling TM, Aaronson KD, Cody RJ, Bach DS, Armstrong WF (2002) Prognostic significance of mitral regurgitation and tricuspid regurgitation in patients with left ventricular systolic dysfunction. Am Heart J 144(3):524–529
Izumi C, Miyake M, Takahashi S, Matsutani H, Hashiwada S, Kuwano K, Hayashi H, Nakajima S, Nishiga M, Hanazawa K, Sakamoto J, Kondo H, Tamura T, Kaitani K, Yamanaka K, Nakagawa Y (2011) Progression of isolated tricuspid regurgitation late after left-sided valve surgery. Clinical features and mechanisms. Circ J 75:2902–2907
Benfari G, Antoine C, Miller WL, Thapa P, Topilsky Y, Rossi A, Michelena HI, Pislaru S, Enriquez-Sarano M (2019) Excess mortality associated with functional tricuspid regurgitation complicating heart failure with reduced ejection fraction. Circulation 140(3):196–206
Bar N, Schwartz LA, Biner S, Aviram G, Ingbir M, Nachmany I, Margolis G, Sadeh B, Barashi R, Keren G, Topilsky Y (2018) Clinical outcome of isolated tricuspid regurgitation in patients with preserved left ventricular ejection fraction and pulmonary hypertension. J Am Soc Echocardiogr 31:34–41
Dahou A, Magne J, Clavel MA, Capoulade R, Bartko PE, Bergler-Klein J, Sénéchal M, Mundigler G, Burwash I, Ribeiro HB, O'Connor K, Mathieu P, Baumgartner H, Dumesnil JG, Rosenhek R, Larose E, Rodés-Cabau J, Pibarot P (2015) Tricuspid regurgitation is associated with increased risk of mortality in patients with low-flow low-gradient aortic stenosis and reduced ejection fraction: results of the multicenter TOPAS study (True or Pseudo-Severe Aortic Stenosis). JACC Cardiovasc Interv 8:588–596
Abe Y, Akamatsu K, Ito K, Matsumura Y, Shimeno K, Naruko T, Takahashi Y, Shibata T, Yoshiyama M (2018) Prevalence and prognostic significance of functional mitral and tricuspid regurgitation despite preserved left ventricular ejection fraction in atrial fibrillation patients. Circ J 82:1451–1458
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, American College of Cardiology/American Heart Association Task Force on Practice Guidelines (2014) 2014 AHA / ACC guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol 63(22):e57–185
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL, ESC Scientific Document Group (2017) 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 38(36):2739–2791
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging 16:233–270
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American society of echocardiography: endorsed by the European association of echocardiography, a registered branch of the European society of cardiology, and the canadian society of echocardiography. J Am Soc Echocardiogr 23:685–713
Shin SH, Park MY, Oh WJ, Hong SJ, Pak HN, Song WH, Lim DS, Kim YH, Shim WJ (2008) Left atrial volume is a predictor of atrial fibrillation recurrence after catheter ablation. J Am Soc Echocardiogr 21:697–702
Mont L, Bisbal F, Hernández-Madrid A, Pérez-Castellano N, Viñolas X, Arenal A, Arribas F, Fernández-Lozano I, Bodegas A, Cobos A, Matía R, Pérez-Villacastín J, Guerra JM, Ávila P, López-Gil M, Castro V, Arana JI, Brugada J (2014) Catheter ablation vs. antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study). Eur Heart J 35:501–507
Torii Y, Kusunose K, Yamada H, Nishio S, Hirata Y, Amano R, Yamao M, Bando M, Hayashi S, Sata M (2016) Comparison of tricuspid annular plane systolic excursion in patients with atrial fibrillation versus sinus rhythm. Am J Cardiol 117:226–232
Zhou X, Otsuji Y, Yoshifuku S, Yuasa T, Zhang H, Takasaki K, Matsukida K, Kisanuki A, Minagoe S, Tei C (2002) Impact of atrial fibrillation on tricuspid and mitral annular dilatation and valvular regurgitation. Circ J 66:913–916
Acknowledgements
We thank Jane Charbonneau, DVM, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kiho Itakura declares that she has no conflict of interest. Takayuki Hidaka declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Itakura, K., Hidaka, T., Nakano, Y. et al. Successful catheter ablation of persistent atrial fibrillation is associated with improvement in functional tricuspid regurgitation and right heart reverse remodeling. Heart Vessels 35, 842–851 (2020). https://doi.org/10.1007/s00380-019-01546-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01546-3