Abstract
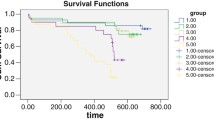
Kidney dysfunction (KD) is closely associated with poor clinical outcome in patients with heart failure (HF). KD is classified as intrinsic and pre-renal KD. However, the impact of each KD on the clinical outcome in patients with HF has not yet been fully elucidated. We measured the urinary to serum creatinine (UC/SC) ratio, a marker for intrinsic and pre-renal KD, in 1009 consecutive patients with HF at admission. There were 314 cardio-renal events including HF and advanced end-stage renal dysfunction during the median follow-up period of 1154 days. There were 63 (6%) patients with intrinsic KD (UC/SC ratio < 20), 118 (12%) patients with intermediate KD (UC/SC ratio 20–40), 607 (60%) patients with pre-renal KD (UC/SC ratio > 40), and 221 (22%) patients with no KD. Multivariate Cox’s proportional hazard regression analysis demonstrated that intrinsic and intermediate KDs were significantly associated with poor clinical outcome. The prediction model for cardio-renal events was significantly improved by the addition of UC/SC ratio to the confounding risk factors. Subgroup analysis in patients with HF with severely reduced glomerular filtration rates showed that the prevalence rates of intrinsic, intermediate, and pre-renal KDs were 23%, 30%, and 47%, respectively. The cardio-renal event rate was the highest in the intrinsic KD group compared with that in the other groups. Intrinsic KD was closely associated with extremely poor clinical outcome in patients with HF. The UC/SC ratio could provide important clinical information for the treatment and management of KD in patients with HF.





Similar content being viewed by others
References
Bui AL, Horwich TB, Fonarow GC (2011) Epidemiology and risk profile of heart failure. Nat Rev Cardiol 8(1):30–41
Goh CY, Vizzi G, De Cal M, Ronco C (2011) Cardiorenal syndrome: a complex series of combined heart/kidney disorders. Contrib Nephrol 174:33–45
Giamouzis G, Kalogeropoulos AP, Butler J, Karayannis G, Georgiopoulou VV, Skoularigis J, Triposkiadis F (2013) Epidemiology and importance of renal dysfunction in heart failure patients. Curr Heart Fail Rep 10(4):411–420
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R (2008) Cardiorenal syndrome. J Am Coll Cardiol 52(19):1527–1539
Eckardt KU, Berns JS, Rocco MV, Kasiske BL (2009) Definition and classification of CKD: the debate should be about patient prognosis—a position statement from KDOQI and KDIGO. Am J Kidney Dis 53(6):915–920
Damman K, Van Veldhuisen DJ, Navis G, Vaidya VS, Smilde TD, Westenbrink BD, Bonventre JV, Voors AA, Hillege HL (2010) Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate. Heart 96(16):1297–1302
Otaki Y, Watanabe T, Shishido T, Takahashi H, Funayama A, Narumi T, Kadowaki S, Hasegawa H, Honda S, Netsu S, Ishino M, Arimoto T, Miyashita T, Miyamoto T, Konta T, Kubota I (2013) The impact of renal tubular damage, as assessed by urinary β2–microglobulin–creatinine ratio, on cardiac prognosis in patients with chronic heart failure. Circ Heart Fail 6(4):662–668
Damman K, Valente MA, Voors AA, O'Connor CM, van Veldhuisen DJ, Hillege HL (2014) Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J 35(7):455–469
McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285(26):1441–1446
Brisco MA, Coca SG, Chen J, Owens AT, McCauley BD, Kimmel SE, Testani JM (2013) Blood urea nitrogen/creatinine ratio identifies a high-risk but potentially reversible form of renal dysfunction in patients with decompensated heart failure. Circ Heart Fail 6(2):233–239
Larsson A, Malm J, Grubb A, Hansson LO (2004) Calculation of glomerular filtration rate expressed in mL/min from plasma cystatin C values in mg/L. Scand J Clin Lab Investig 64(1):25–30
Laterza OF, Price CP, Scott MG (2002) Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem 48(5):699–707
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53(6):982–992
Esson ML, Schrier RW (2002) Diagnosis and treatment of acute tubular necrosis. Ann Intern Med 137(9):744–752
Sood MM, Saeed M, Lim V, Cordova F, Komenda P, Malik A, Rigatto C, Shafer LA, Tangri N, Tappia PS, Zieroth S (2015) The urea-to-creatinine ratio is predictive of worsening kidney function in ambulatory heart failure patients. J Card Fail 21(5):412–418
Nangaku M (2006) Chronic hypoxia and tubulointerstitial injury: a final common pathway to end-stage renal failure. J Am Soc Nephrol 17(1):17–25
Damman K, Masson S, Hillege HL, Voors AA, van Veldhuisen DJ, Rossignol P, Proietti G, Barbuzzi S, Nicolosi GL, Tavazzi L, Maggioni AP, Latini R (2013) Tubular damage and worsening renal function in chronic heart failure. JACC Heart Fail 1(5):417–424
Miller TR, Anderson RJ, Linas SL, Henrich WL, Berns AS, Gabow PA, Schrier RW (1978) Urinary diagnostic indices in acute renal failure: a prospective study. Ann Intern Med 89(1):47–50
Sinkeler SJ, Damman K, van Veldhuisen DJ, Hillege H, Navis G (2012) A re-appraisal of volume status and renal function impairment in chronic heart failure: combined effects of pre-renal failure and venous congestion on renal function. Heart Fail Rev 17(2):263–270
Guazzi M, Gatto P, Giusti G, Pizzamiglio F, Previtali I, Vignati C, Arena R (2013) Pathophysiology of cardiorenal syndrome in decompensated heart failure: role of lung-right heart-kidney interaction. Int J Cardiol 169(6):379–384
Martinez-Santos P, Vilacosta I (2011) Cardiorenal syndrome: an unsolved clinical problem. Int J Nephrol 2011:913029
McAlister FA, Ezekowitz J, Tonelli M, Armstrong PW (2004) Renal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort study. Circulation 109(8):1004–1009
Mahon NG, Blackstone EH, Francis GS, Starling RC 3rd, Young JB, Lauer MS (2002) The prognostic value of estimated creatinine clearance alongside functional capacity in ambulatory patients with chronic congestive heart failure. J Am Coll Cardiol 40(6):1106–1113
Ter JM, Maaten, Damman K, Hillege HL, Bakker SJ, Anker SD, Navis G, Voors AA (2014) Creatinine excretion rate, a marker of muscle mass, is related to clinical outcome in patients with chronic systolic heart failure. Clin Res Cardiol 103(12):976–983
Wilson FP, Xie D, Anderson AH, Leonard MB, Reese PP, Delafontaine P, Horwitz E, Kallem R, Navaneethan S, Ojo A, Porter AC, Sondheimer JH, Sweeney HL, Townsend RR, Feldman HI (2014) Urinary creatinine excretion, bioelectrical impedance analysis, and clinical outcomes in patients with CKD: the CRIC study. Clin J Am Soc Nephrol 9(12):2095–2103
Shiba N, Nochioka K, Miura M, Kohno H, Shimokawa H (2011) Trend of westernization of etiology and clinical characteristics of heart failure patients in Japan—first report from the CHART-2 study. Circ J 75(4):823–833
von Scheidt W, Zugck C, Pauschinger M, Hambrecht R, Bruder O, Hartmann A, Rauchhaus M, Zahn R, Brachmann J, Tebbe U, Neumann T, Strasser RH, Bohm M, Stork S, Hochadel M, Heidemann P, Senges J (2014) Characteristics, management modalities and outcome in chronic systolic heart failure patients treated in tertiary care centers: results from the EVIdence based TreAtment in Heart Failure (EVITA-HF) registry. Clin Res Cardiol 103(12):1006–1014
Smith GL, Lichtman JH, Bracken MB, Shlipak MG, Phillips CO, DiCapua P, Krumholz HM (2006) Renal impairment and outcomes in heart failure: systematic review and meta-analysis. J Am Coll Cardiol 47(10):1987–1996
Acknowledgements
This study was supported, in part, by a Grant-in-aid for Scientific Research (nos. 16K09490 and 18K15838) from the Ministry of Education Culture, Sport, Science, and Technology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
380_2019_1472_MOESM1_ESM.tif
The association of KD category with clinical outcomes such as heart failure re-hospitalization, ESRD, cardiac deaths, and all-cause deaths. KD, kidney dysfunction. ESRD, end-stage renal disease. (TIFF 132 kb)
380_2019_1472_MOESM2_ESM.tif
Receiver operating characteristic curve of urinary to serum creatinine ratio, urinary creatinine and serum creatinine for cardio-renal events in patients with advanced chronic kidney disease. (TIFF 92 kb)
Rights and permissions
About this article
Cite this article
Otaki, Y., Watanabe, T., Konta, T. et al. The impact of kidney dysfunction categorized by urinary to serum creatinine ratio on clinical outcomes in patients with heart failure. Heart Vessels 35, 187–196 (2020). https://doi.org/10.1007/s00380-019-01472-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01472-4