Abstract
Nitroglycerin is commonly used as an antispasmodic for treating spasm of coronary artery bypass grafts. This study investigated whether the presence of renal failure affects reactivity to nitroglycerin in internal thoracic arteries obtained from patients undergoing coronary bypass surgery. The patients were divided into three groups according to estimated glomerular filtration rate (eGFR, mL/min/1.73 m2): without renal failure (60 ≤ eGFR, n = 13), with moderate renal failure (30 ≤ eGFR < 60, n = 10), and with severe renal failure (eGFR < 30, n = 10). Organ chamber technique was used to evaluate concentration-related responses of isolated internal thoracic arteries to vasodilators. Nitroglycerin induced a concentration-dependent relaxation, which was significantly augmented in patients with severe but not moderate renal failure than in those without renal failure. In addition, there was a negative correlation between eGFR and the relaxant efficacy of nitroglycerin (P = 0.016). On the other hand, relaxant responses to BAY 60-2770 (which enhances cGMP generation as with nitroglycerin) were similar among three grades of renal function. An inverse relationship of eGFR to the relaxant efficacy of BAY 60-2770 was not observed, either (P = 0.314). These findings suggest that severe renal failure specifically potentiates nitroglycerin-induced relaxation in internal thoracic artery grafts.


Similar content being viewed by others
References
Sivalingam S, Levine A, Dunning J (2005) What is the optimal vasodilator for preventing spasm in the left internal mammary artery during coronary arterial bypass grafting? Interact Cardiovasc Thorac Surg 4:365–371
Torfgård KE, Ahlner J (1994) Mechanisms of action of nitrates. Cardiovasc Drugs Ther 8:701–717
Huraux C, Makita T, Kurz S, Yamaguchi K, Szlam F, Tarpey MM, Wilcox JN, Harrison DG, Levy JH (1999) Superoxide production, risk factors, and endothelium-dependent relaxations in human internal mammary arteries. Circulation 99:53–59
Tawa M, Kinoshita T, Asai T, Suzuki T, Imamura T, Okamura T (2015) Influence of smoking on vascular reactivity to cGMP generators in human internal thoracic arteries. BMC Pharmacol Toxicol 16(Suppl 1):A93
Tawa M, Kinoshita T, Asai T, Suzuki T, Imamura T, Okamura T (2017) Impact of type 2 diabetes on vascular reactivity to cGMP generators in human internal thoracic arteries. Vascul Pharmacol 91:36–41
Smilowitz NR, Gupta N, Guo Y, Mauricio R, Bangalore S (2017) Management and outcomes of acute myocardial infarction in patients with chronic kidney disease. Int J Cardiol 227:1–7
Schiffrin EL, Lipman ML, Mann JF (2007) Chronic kidney disease: effects on the cardiovascular system. Circulation 116:85–97
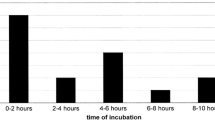
Kleszczewski T, Buzun L, Lisowska A, Modzelewska B (2016) Potassium induced contraction of the internal thoracic artery in vitro is time related: the potential consequences in the analysis of the mechanism of the spasm after coronary artery bypass grafting and in the analysis of the results of in vitro studies. Heart Vessels 31:616–621
Kinoshita T, Tawa M, Suzuki T, Aimi Y, Asai T, Okamura T (2017) Endothelial dysfunction of internal thoracic artery graft in patients with chronic kidney disease. J Thorac Cardiovasc Surg 153:317–324
Rhodin JAG (1980) Architecture of the vessel wall. In: Bohr DF, Somlyo AP, Sparks HV (eds) Handbook of physiology, vol 2. American Physiological Society, Bethesda, pp 1–31
Knorr A, Hirth-Dietrich C, Alonso-Alija C, Härter M, Hahn M, Keim Y, Wunder F, Stasch JP (2008) Nitric oxide-independent activation of soluble guanylate cyclase by BAY 60-2770 in experimental liver fibrosis. Arzneimittelforschung 58:71–80
Kurata N, Nakamura S, Mizumura J, Sumi M, Nishimura Y, Yamamoto T, Yasuhara H (1999) Enhancement of nitroglycerin induced blood vessel relaxation in chronic renal failure model rats. Res Commun Mol Pathol Pharmacol 106:23–36
Sorrentino R, Sorrentino L, Pinto A (1993) Effect of some products of protein catabolism on the endothelium-dependent and -independent relaxation of rabbit thoracic aorta rings. J Pharmacol Exp Ther 266:626–633
van der Harst P, Smilde TD, Buikema H, Voors AA, Navis G, van Veldhuisen DJ, van Gilst WH (2006) Vascular function and mild renal impairment in stable coronary artery disease. Arterioscler Thromb Vasc Biol 26:379–384
Sindhu RK, Ehdaie A, Vaziri ND, Roberts CK (2004) Effects of chronic renal failure on caveolin-1, guanylate cyclase and AKT protein expression. Biochim Biophys Acta 1690:231–237
Neubauer R, Wölkart G, Opelt M, Schwarzenegger C, Hofinger M, Neubauer A, Kollau A, Schmidt K, Schrammel A, Mayer B (2015) Aldehyde dehydrogenase-independent bioactivation of nitroglycerin in porcine and bovine blood vessels. Biochem Pharmacol 93:440–448
Mezzetti A, Lapenna D, Calafiore AM, Proietti-Franceschilli G, Porreca E, De Cesare D, Neri M, Di Ilio C, Cuccurullo F (1992) Glutathione-related enzyme activities and lipoperoxide levels in human internal mammary artery and ascending aorta. Relations with serum lipids. Arterioscler Thromb 12:92–98
Hink U, Daiber A, Kayhan N, Trischler J, Kraatz C, Oelze M, Mollnau H, Wenzel P, Vahl CF, Ho KK, Weiner H, Munzel T (2007) Oxidative inhibition of the mitochondrial aldehyde dehydrogenase promotes nitroglycerin tolerance in human blood vessels. J Am Coll Cardiol 50:2226–2232
Archer SL, Gragasin FS, Wu X, Wang S, McMurtry S, Kim DH, Platonov M, Koshal A, Hashimoto K, Campbell WB, Falck JR, Michelakis ED (2003) Endothelium-derived hyperpolarizing factor in human internal mammary artery is 11,12-epoxyeicosatrienoic acid and causes relaxation by activating smooth muscle BK(Ca) channels. Circulation 107:769–776
Seto SW, Au AL, Poon CC, Zhang Q, Li RW, Yeung JH, Kong SK, Ngai SM, Wan S, Ho HP, Lee SM, Hoi MP, Chan SW, Leung GP, Kwan YW (2013) Acute simvastatin inhibits K ATP channels of porcine coronary artery myocytes. PLoS One 8:e66404
Dessì M, Noce A, Dawood KF, Galli F, Taccone-Gallucci M, Fabrini R, Bocedi A, Massoud R, Fucci G, Pastore A, Manca di Villahermosa S, Zingaretti V, Federici G, Ricci G (2012) Erythrocyte glutathione transferase: a potential new biomarker in chronic kidney diseases which correlates with plasma homocysteine. Amino Acids 43:347–354
El-Rashidy FH, Al-Turk WA, Stohs SJ (1984) Glutathione, glutathione reductase and glutathione S-transferase activities in erythrocytes and lymphocytes in chronic renal disease. Res Commun Chem Pathol Pharmacol 44:423–430
Mimic-Oka J, Simic T, Djukanovic L, Stefanovski J, Ramic Z (1992) Glutathione and its associated enzymes in peripheral blood cells in different stages of chronic renal insufficiency. Amino Acids 2:215–224
Galli F, Rovidati S, Benedetti S, Buoncristiani U, Covarelli C, Floridi A, Canestrari F (1999) Overexpression of erythrocyte glutathione S-transferase in uremia and dialysis. Clin Chem 45:1781–1788
Kugiyama K, Yasue H, Okumura K, Ogawa H, Fujimoto K, Nakao K, Yoshimura M, Motoyama T, Inobe Y, Kawano H (1996) Nitric oxide activity is deficient in spasm arteries of patients with coronary spastic angina. Circulation 94:266–271
Motoyama T, Kawano H, Kugiyama K, Okumura K, Ohgushi M, Yoshimura M, Hirashima O, Yasue H (1997) Flow-mediated, endothelium-dependent dilatation of the brachial arteries is impaired in patients with coronary spastic angina. Am Heart J 133:263–267
Gruhn N, Boesgaard S, Eiberg J, Bang L, Thiis J, Schroeder TV, Aldershvile J (2002) Effects of large conductance Ca(2+)-activated K(+) channels on nitroglycerin-mediated vasorelaxation in humans. Eur J Pharmacol 446:145–150
Wei JY, Reid PR (1979) Quantitative determination of trinitroglycerin in human plasma. Circulation 59:588–592
Sarabu MR, McClung JA, Fass A, Reed GE (1987) Early postoperative spasm in left internal mammary artery bypass grafts. Ann Thorac Surg 44:199–200
Vogt PR, Hess O, Turina MI (1996) Internal mammary artery spasm immediately after grafting to the left anterior descending artery: diagnosis and treatment. Eur Heart J 17:804
He GW, Fan KY, Chiu SW, Chow WH (2000) Injection of vasodilators into arterial grafts through cardiac catheter to relieve spasm. Ann Thorac Surg 69:625–628
He GW (2013) Arterial grafts: clinical classification and pharmacological management. Ann Cardiothorac Surg 2:507–518
Fukuda S, Nakamura Y, Egi K, Fujioka S, Nagasaka S, Minh PN, Toguchi K, Wada T, Izumi-Nakaseko H, Ando K, Mizoue T, Takazawa K, Hosaka S, Sugiyama A (2016) Comparison of direct effects of clinically available vasodilators; nitroglycerin, nifedipine, cilnidipine and diltiazem, on human skeletonized internal mammary harvested with ultrasonic scalpel. Heart Vessels 31:1681–1684
He GW, Taggart DP (2016) Spasm in arterial grafts in coronary artery bypass grafting surgery. Ann Thorac Surg 101:1222–1229
Acknowledgements
This work was supported in part by the Smoking Research Foundation and by the Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan (Grant Number 17K15579). The authors wish to thank Dr. Johannes-Peter Stasch (Institute of Cardiovascular Research, Pharma Research Centre, Bayer AG) for the gift of BAY 60-2770.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Tawa, M., Kinoshita, T., Asai, T. et al. Responsiveness of internal thoracic arteries to nitroglycerin in patients with renal failure. Heart Vessels 33, 682–687 (2018). https://doi.org/10.1007/s00380-017-1105-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-1105-1