Abstract
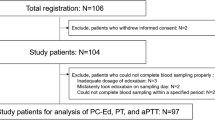
Whether trough-phase rivaroxaban concentrations provide sufficient anticoagulation needs more study. We evaluated levels of coagulation activation markers in the trough concentration phase in nonvalvular atrial fibrillation (NVAF) patients, and the correlation between these markers and rivaroxaban concentration. Fifty-five Japanese NVAF patients received 24-week rivaroxaban treatment of either 15 or 10 mg once-daily in the morning. Of these, 26 patients had no history of anticoagulant therapy (naive group) and 29 had switched from warfarin (warfarin group). D-dimer and prothrombin fragment 1 + 2 (F1 + 2) levels, and protein C activities were measured at 0 (baseline), 12 and 24 weeks of rivaroxaban treatment just before the patient’s regular dosing time (trough phase). For 49 patients, D-dimer, F1 + 2, and rivaroxaban concentrations were also measured twice between 28 and 32 weeks of rivaroxaban treatment at non-trough times to achieve a range of drug concentrations for correlation analysis. For the naive group, D-dimer and F1 + 2 levels were significantly reduced (p < 0.01) from baseline at 12 and 24 weeks. For the warfarin group, these values were unchanged for D-dimer but significantly increased (p < 0.01) for F1 + 2. Protein C activity was unchanged in the naive group and was increased (p < 0.01) in the warfarin group. Prothrombin time (r = 0.92, p < 0.0001) and activated partial thromboplastin time (r = 0.54, p < 0.0001) correlated with rivaroxaban concentration, but not D-dimer and F1 + 2 levels. In conclusion, rivaroxaban in the trough phase is comparable to warfarin in reducing D-dimer levels. Although trough level rivaroxaban suppresses F1 + 2 less than warfarin, the higher activities of protein C with rivaroxaban treatment compared to warfarin treatment may counterbalance this. Lack of correlation between rivaroxaban concentration and D-dimer and F1 + 2 levels suggests that trough concentrations of rivaroxaban reduce their concentrations as effectively as higher levels do.





Similar content being viewed by others
References
Hori M, Matsumoto M, Tanahashi N, Momomura S, Uchiyama S, Goto S, Izumi T, Koretsune Y, Kajikawa M, Kato M, Ueda H, Iwamoto K, Tajiri M (2012) Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation—the J-ROCKET AF study. Circ J 76:2104–2111
Tagaya M, Yoshikawa D, Sugishita Y, Yamauchi F, Ito T, Kameda T, Yoshinaga M, Mukaide D, Fujiwara W, Yokoi H, Hayashi M, Watanabe E, Ishii J, Ozaki Y, Izawa H (2016) Prescription patterns of oral anticoagulants for patients with non-valvular atrial fibrillation: experience at a Japanese single institution. Heart Vessels 31:957–962
Miyamoto K, Aiba T, Arihiro S, Watanabe M, Kokubo Y, Ishibashi K, Hirose S, Wada M, Nakajima I, Okamura H, Noda T, Nagatsuka K, Noguchi T, Anzai T, Yasuda S, Ogawa H, Kamakura S, Shimizu W, Miyamoto Y, Toyoda K, Kusano K (2015) Impact of renal function deterioration on adverse events during anticoagulation therapy using non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Heart Vessels. doi:10.1007/s00380-015-0725-6
Trujillo T, Dobesh PP (2014) Clinical use of rivaroxaban: pharmacokinetic and pharmacodynamic rationale for dosing regimens in different indications. Drugs 74:1587–1603
Yasaka M, Lip GYH (2014) Stroke prevention in Asian patients with atrial fibrillation. Stroke 45:1608–1609
Rühl H, Berens C, Winterhagen A, Müller J, Oldenburg J, Pötzsch B (2015) Label-free kinetic studies of hemostasis-related biomarkers including D-dimer using autologous serum transfusion. PLoS One 10(12):e0145012
Tanigawa T, Kaneko M, Hashizume K, Kajikawa M, Ueda H, Tajiri M, Paolini JF, Mueck W (2013) Model-based dose selection for phase III rivaroxaban study in Japanese patients with non-valvular atrial fibrillation. Drug Metab Pharmacokinet 28:59–70
Kaneko M, Tanigawa T, Hashizume K, Kajikawa M, Tajiri M, Mueck W (2013) Confirmation of model-based dose selection for a Japanese phase III study of rivaroxaban in non-valvular atrial fibrillation patients. Drug Metab Pharmacokinet 28:321–331
Kuhn J, Gripp T, Flieder T, Dittrich M, Hendig D, Busse J, Knabbe C, Birschmann I (2015) UPLC-MRM mass spectrometry method for measurement of the coagulation inhibitors dabigatran and rivaroxaban in human plasma and its comparison with functional assays. PLoS One 10(12):e0145478
Ikeda K, Tachibana H (2016) Clinical implication of monitoring rivaroxaban and apixaban by using anti-factor Xa assay in patients with non-valvular atrial fibrillation. J Arrhythm 32:42–50
Nakano Y, Kondo T, Osanai H, Murase Y, Nakashima Y, Asano H, Ajioka M, Sakai K, Inden Y, Murohara T (2015) Clinical usefulness of measuring prothrombin time and soluble fibrin levels in Japanese patients with atrial fibrillation receiving rivaroxaban. J Cardiol 65:185–190
Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G (2012) Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e44S–e88S
Rezaie AR (2010) Regulation of the protein C anticoagulant and antiinflammatory pathways. Curr Med Chem 17(19):2059–2069
Tajiri K, Sato A, Harunari T, Shimojo N, Yamaguchi I, Aonuma K (2015) Impact of rivaroxaban compared with warfarin on the coagulation status in Japanese patients with non-valvular atrial fibrillation: a preliminary analysis of the prothrombin fragment 1 + 2 levels. J Cardiol 65:191–196
Nakatani Y, Mizumaki K, Nishida K, Hirai T, Sakabe M, Oda Y, Joho S, Fujiki A, Nozawa T, Inoue H (2012) Anticoagulation control quality affects the D-dimer levels of atrial fibrillation patients. Circ J 76:317–321
Lip GYH, Lowe GDO, Rumley A, Dunn FG (1995) Increased markers of thrombogenesis in chronic atrial fibrillation: effects of warfarin treatment. Br Heart J 73:527–533
Somlói M, Tomcsányi J, Nagy E, Bodó I, Bezzegh A (2003) D-dimer determination as a screening tool to exclude atrial thrombi in atrial fibrillation. Am J Cardiol 92:85–87
Sadanaga T, Sadanaga M, Ogawa S (2010) Evidence that D-dimer levels predict subsequent thromboembolic and cardiovascular events in patients with atrial fibrillation during oral anticoagulant therapy. J Am Coll Cardiol 55:2225–2231
Christersson C, Wallentin L, Andersson U, Alexander JH, Ansell J, De Caterina R, Gersh BJ, Granger CB, Hanna M, Horowitz JD, Huber K, Husted S, Hylek EM, Lopes RD, Siegbahn A (2014) D-dimer and risk of thromboembolic and bleeding events in patients with atrial fibrillation–observations from the ARISTOTLE trial. J Thromb Haemost 12:1401–1412
Bounameaux H, Reber G (2010) New oral antithrombotics: a need for laboratory monitoring. Against J Thromb Haemost 8:627–630
Garcia D, Barrett YC, Ramacciotti E, Weitz JI (2013) Laboratory assessment of the anticoagulant effects of the next generation of oral anticoagulants. J Thromb Haemost 11:245–252
Samama MM, Contant G, Spiro TE, Perzborn E, Le Flem L, Guinet C, Gourmelin Y, Rohde G, Martinoli JL (2013) Laboratory assessment of rivaroxaban: a review. Thromb J 11(1):11
Kitchen S, Gray E, Mackie I, Baglin T, Makris M, BCSH Committee (2014) Measurement of non-coumarin anticoagulants and their effects on tests of haemostasis: guidance from the British Committee for Standards in Haematology. Br J Haematol 166:830–841
Cuker A, Siegal DM, Crowther MA, Garcia DA (2014) Laboratory measurement of the anticoagulant activity of the non-vitamin K oral anticoagulants. J Am Coll Cardiol 64:1128–1139
Baglin T, Keeling D, Kitchen S (2012) Effects on routine coagulation screens and assessment of anticoagulant intensity in patients taking oral dabigatran or rivaroxaban: guidance from the British Committee for Standards in Haematology. Br J Haematol 159:427–429
Gosselin R, Grant RP, Adcock DM (2016) Comparison of the effect of the anti-Xa direct oral anticoagulants apixaban, edoxaban, and rivaroxaban on coagulation assays. Int J Lab Hematol. doi:10.1111/ijlh.12528
Douxfils J, Tamigniau A, Chatelain B, Chatelain C, Wallemacq P, Dogné JM, Mullier F (2013) Comparison of calibrated chromogenic anti-Xa assay and PT tests with LC-MS/MS for the therapeutic monitoring of patients treated with rivaroxaban. Thromb Haemost 110:723–731
Al-Aieshy F, Malmström RE, Antovic J, Pohanka A, Rönquist-Nii Y, Berndtsson M, Al-Khalili F, Skeppholm M (2016) Clinical evaluation of laboratory methods to monitor exposure of rivaroxaban at trough and peak in patients with atrial fibrillation. Eur J Clin Pharmacol 72:671–679
Mani H, Hesse C, Stratmann G, Lindhohh-Last E (2013) Ex vivo effects of low-dose rivaroxaban on specific coagulation assays and coagulation factor activities in patients under real life conditions. Thromb Haemost 109:127–136
Acknowledgements
The authors thank Dr. Yoshiaki Ishiguro, Dr. Hiroyuki Matsuyama, Dr. Kazuo Kato, Dr. Akihisa Uemura, Dr. Satoshi Yoshida, Dr. Atsushi Kani, Dr. Kazuo Hasegawa, Dr. Mamoru Tokuda, Dr. Fumio Matsubara, Dr. Uchiyama Tatsushi, and Dr. Kazuma Mori for their cooperation with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The corresponding author (Junnichi Ishii) received research funding for this study from Bayer Yakuhin, Ltd. Japan, the manufacturer of rivaroxaban. However, the funder had no role in study design, data collection, and analysis, or preparation of the manuscript. The other authors have no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
380_2016_912_MOESM1_ESM.pdf
Supplementary file 1 Post-rivaroxaban treatment changes in trough levels of activated partial thromboplastin time (APTT) in A naive and B warfarin groups (PDF 114 kb)
Rights and permissions
About this article
Cite this article
Kitagawa, F., Ishii, J., Hiramitsu, S. et al. Assessment of trough rivaroxaban concentrations on markers of coagulation activation in nonvalvular atrial fibrillation population. Heart Vessels 32, 609–617 (2017). https://doi.org/10.1007/s00380-016-0912-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0912-0