Abstract
Objective
To investigate the association between low-dose aspirin use for primary prevention and self-reported kidney stones prevalence in the 40–79 years old population.
Methods
We conducted a cross-sectional study based on the United States population data from the National Health and Nutrition Examination Survey 2011–2018. Baseline demographical and clinical data were collected. The univariate and multivariate regression was performed to identify confounding factors and assess the relationship between aspirin use for primary prevention and the prevalence of self-reported kidney stones. A propensity-score matching was used to identify patients with similar baseline characteristics to adjust for the bias caused by confounding factors.
Results
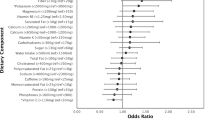
A total of 10,256 low-dose aspirin-use participants were included in this study. 10.4% of participants reported a history of kidney stones, and 18.5% reported a continuous use of low-dose prophylactic aspirin. Multivariate logistic regression analysis showed that low-dose preventive aspirin use had significantly increased the odds of self-reported kidney stones (OR = 1.245; 95% CI: 1.063–1.459; p = 0.007). In subgroup analysis, this finding was primarily limited to males (OR = 1.311), non-hypertensive participants (OR = 1.443), diabetic participants (OR = 1.380), and older (60 ≤ Age < 80) (OR = 1.349). The propensity-score matched analyses supported this result after adjusting for the bias caused by potential confounders (OR = 1.216; 95% CI: 1.011–1.462; p = 0.038).
Conclusion
In this study, there exists a significant relationship between low-dose aspirin for primary prevention and self-reported kidney stones, primarily among males, no hypertensive participants, diabetics, or older adults. Further studies are needed to elucidate the mechanisms underlying these findings in the future.
Similar content being viewed by others

Data availability
The datasets generated during the current study are available in the public database (NHANES) [https://www.cdc.gov/nchs/nhanes/].
References
Moe OW (2006) Kidney stones: pathophysiology and medical management. Lancet (London, England) 367(9507):333–44. https://doi.org/10.1016/s0140-6736(06)68071-9. (Epub 2006/01/3)
Scales CD Jr, Smith AC, Hanley JM, Saigal CS (2012) Prevalence of kidney stones in the United States. Eur Urol 62(1):160–5. https://doi.org/10.1016/j.eururo.2012.03.052. (Epub 2012/04/14)
Abdelaziz HK, Saad M, Pothineni NVK, Megaly M, Potluri R, Saleh M et al (2019) Aspirin for primary prevention of cardiovascular events. J Am Coll Cardiol 73(23):2915–29. https://doi.org/10.1016/j.jacc.2019.03.501. (Epub 2019/06/15)
Zheng SL, Roddick AJ (2019) Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. Jama 321(3):277–87. https://doi.org/10.1001/jama.2018.20578. (Epub 2019/01/23)
Van’t Hof JR, Duval S, Walts A, Kopecky SL, Luepker RV, Hirsch AT (2017) Contemporary primary prevention aspirin use by cardiovascular disease risk: impact of US preventive services task force recommendations, 2007–2015: a serial, cross-sectional study. J Am Heart Assoc 6:10. https://doi.org/10.1161/jaha.117.006328. (Epub 2017/10/05)
Raber I, McCarthy CP, Vaduganathan M, Bhatt DL, Wood DA, Cleland JGF et al (2019) The rise and fall of aspirin in the primary prevention of cardiovascular disease. Lancet (London, England) 393(10186):2155–67. https://doi.org/10.1016/s0140-6736(19)30541-0. (Epub 2019/06/22)
Devarajan A (1979) 2018 Cross-talk between renal lithogenesis and atherosclerosis: an unveiled link between kidney stone formation and cardiovascular diseases. Clin Sci (London, England 1979) 132(6):615–26. https://doi.org/10.1042/cs20171574. (Epub 2018/03/22)
Fan X, Kalim S, Ye W, Zhao S, Ma J, Nigwekar SU et al (2017) Urinary stone disease and cardiovascular disease risk in a rural Chinese population. Kidney Int Rep 2(6):1042–9. https://doi.org/10.1016/j.ekir.2017.06.001. (Epub 2017/12/23)
Bangalore S, Guo Y, Samadashvili Z, Blecker S, Xu J, Hannan EL (2015) Everolimus-eluting stents or bypass surgery for multivessel coronary disease. N Engl J Med 372(13):1213–22. https://doi.org/10.1056/NEJMoa1412168. (Epub 2015/03/17)
Stuntz M, Bernstein B (2017) Recent trends in the prevalence of low-dose aspirin use for primary and secondary prevention of cardiovascular disease in the United States. Prev Med Rep 5:183–186. https://doi.org/10.1016/j.pmedr.2016.12.023. (Epub 2017/01/11)
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL et al (2016) European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts)developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 37(29):2315–81. https://doi.org/10.1093/eurheartj/ehw106. (Epub 2016/05/26)
Gaziano JM, Brotons C, Coppolecchia R, Cricelli C, Darius H, Gorelick PB et al (2018) Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet (London, England) 392(10152):1036–46. https://doi.org/10.1016/s0140-6736(18)31924-x. (Epub 2018/08/31)
Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J et al (2018) Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med 379(16):1529–39. https://doi.org/10.1056/NEJMoa1804988. (Epub 2018/08/28)
McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR et al (2018) Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 379(16):1509–18. https://doi.org/10.1056/NEJMoa1805819. (Epub 2018/09/18)
Bamberger JN, Rosen DC, Khusid JA, Kaplan-Marans E, Gallante B, Kapoor A et al (2021) The impact of metabolic syndrome components on urinary parameters and risk of stone formation. World J Urol. https://doi.org/10.1007/s00345-021-03790-7. (Epub 2021/07/16)
Sakhaee K, Capolongo G, Maalouf NM, Pasch A, Moe OW, Poindexter J et al (2012) Metabolic syndrome and the risk of calcium stones. Nephrol Dial Transplant:Off Publ European Dial Transplant Assoc-Eur Ren Assoc 27(8):3201–9. https://doi.org/10.1093/ndt/gfr703. (Epub 2012/01/17)
Davison C (1971) Salicylate metabolism in man. Ann N Y. Acad Sci 179:249–68. https://doi.org/10.1111/j.1749-6632.1971.tb46905.x. (Epub 1971/07/06)
Needs CJ, Brooks PM (1985) Clinical pharmacokinetics of the salicylates. Clin Pharmacokinet 10(2):164–77. https://doi.org/10.2165/00003088-198510020-00004. (Epub 1985/03/01)
Harlin HC, Wiesel L (1954) Modification of urinary surface tension by oral glucuronic acid: its application in prophylaxis of urinary calculi. J Urol 72(6):1046–9. https://doi.org/10.1016/s0022-5347(17)67713-9. (Epub 1954/12/01)
Prien EL, Walker BS (1955) Salicylate therapy of recurrent calcium urolithiasis. N Engl J Med 253(11):446–51. https://doi.org/10.1056/nejm195509152531102. (Epub 1955/09/15)
Abrams M (1957) Unfavorable results of acetylsalicylic acid in the treatment of recurrent urolithiasis. J Urol 77(3):372–6. https://doi.org/10.1016/s0022-5347(17)66572-8. (Epub 1957/03/01)
Caspi D, Lubart E, Graff E, Habot B, Yaron M, Segal R (2000) The effect of mini-dose aspirin on renal function and uric acid handling in elderly patients. Arthritis Rheum 43(1):103–8. https://doi.org/10.1002/1529-0131(200001)43:1%3c103::Aid-anr13%3e3.0.Co;2-c. (Epub 2000/01/22)
Ben Salem C, Slim R, Fathallah N, Hmouda H (2017) Drug-induced hyperuricaemia and gout. Rheumatology (Oxford, England) 56(5):679–88. https://doi.org/10.1093/rheumatology/kew293. (Epub 2016/08/09)
Abou-Elela A (2017) Epidemiology, pathophysiology, and management of uric acid urolithiasis: A narrative review. J Advanced Res 8(5):513–27 (Epub 2017/07/28)
Author information
Authors and Affiliations
Contributions
MY: Conceptualization, Visualization, Methodology, Writing an original draft. YL: Investigation, Resources. YC: Methodology, Software, Formal analysis. FH: Conceptualization, Project administration, Supervision.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
The study involving human participants was reviewed and approved by The Wake Forest School of Medicine Institutional Review Board. The participants provided their written informed consent to participate in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, M., Li, Y., Chen, Y. et al. Association of low-dose aspirin use for primary prevention with self-reported kidney stones prevalence: a cross-sectional study. World J Urol 41, 3753–3758 (2023). https://doi.org/10.1007/s00345-023-04657-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04657-9