Abstract
Background
To investigate the association between sleep duration and urgency urinary incontinence (UUI) among adult women.
Methods
Cross-sectional data were retrieved from the 2005–2014 National Health and Nutrition Examination Survey. To explore the association between sleep duration and urgency urinary incontinence, multivariable logistic regression and restricted cubic spline (RCS) regression analysis was carried out.
Results
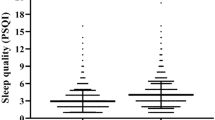
Among 9204 adult women, the weighted urinary incontinence prevalence was 31% for urgency urinary incontinence (UUI). The fully adjusted multivariable model revealed that participants with short (< 7 h) or long (> 9 h) sleep duration were more likely to report UUI compared to participants with normal (7–9 h) sleep duration (OR 1.20, 95% CI 1.03–1.40, p = 0.02, OR 1.40, 95% CI 1.11–1.76, p = 0.005, respectively). Subgroup analysis showed no significant interaction. Furthermore, additional analysis demonstrated a U-shaped correlation between sleep duration and incident UUI.
Conclusion
The non-linear association exists between sleep duration and urgency urinary incontinence. Compared with insufficient or excessive sleep, normal sleep duration is related to lower prevalence of urgency urinary incontinence. Future prospective longitudinal studies should be conducted to further investigate and determine the degree of the association between sleep time and urgent urinary incontinence.

Similar content being viewed by others
Data availability
The datasets analysed during the current study are avaliable from the corresponding author.
References
Rogers RG, Pauls RN, Thakar R, Morin M, Kuhn A, Petri E, Fatton B, Whitmore K, Kinsberg S, Lee J (2018) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the assessment of sexual health of women with pelvic floor dysfunction. Neurourol Urodyn 37(4):1220–1240. https://doi.org/10.1002/nau.23508
Sussman RD, Syan R, Brucker BM (2020) Guideline of guidelines: urinary incontinence in women. BJU Int 125(5):638–655. https://doi.org/10.1111/bju.14927
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29(1):4–20. https://doi.org/10.1002/nau.20798
Minassian VA, Hagan KA, Erekson E, Austin AM, Carmichael D, Bynum JPW, Grodstein F (2020) The natural history of urinary incontinence subtypes in the Nurses’ Health Studies. Am J Obstet Gynecol 222(2):163.e1-163.e8. https://doi.org/10.1016/j.ajog.2019.08.023
Kwon BE, Kim GY, Son YJ, Roh YS, You MA (2010) Quality of life of women with urinary incontinence: a systematic literature review. Int Neurourol J 14(3):133–138. https://doi.org/10.5213/inj.2010.14.3.133
Wood LN, Anger JT (2014) Anger: urinary incontinence in women. BMJ 349:4531. https://doi.org/10.1136/bmj.g4531
Markland AD, Vaughan CP, Okosun IS, Goode PS, Burgio KL, Johnson TM 2nd (2018) Cluster analysis of multiple chronic conditions associated with urinary incontinence among women in the USA. BJU Int 122(6):1041–1048. https://doi.org/10.1111/bju.14246
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L (2017) Urinary incontinence in women: a review. JAMA 318(16):1592–1604. https://doi.org/10.1001/jama.2017.12137
Lecci S, Fernandez LM, Weber FD, Cardis R, Chatton JY, Born J, Lüthi A (2017) Coordinated infraslow neural and cardiac oscillations mark fragility and offline periods in mammalian sleep. Sci Adv 3(2):e1602026. https://doi.org/10.1126/sciadv.1602026
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, Adams Hillard PJ (2015) National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 1(1):40–43. https://doi.org/10.1016/j.sleh.2014.12.010
Bin YS, Marshall NS, Glozier N (2012) Secular trends in adult sleep duration: a systematic review. Sleep Med Rev 16(3):223–230. https://doi.org/10.1016/j.smrv.2011.07.003
Sheehan CM, Frochen SE, Walsemann KM, Ailshire JA (2019) Are U.S. adults reporting less sleep?: findings from sleep duration trends in the National Health Interview Survey, 2004–2017. Sleep. https://doi.org/10.1093/sleep/zsy221
Huang T, Redline S (2019) Cross-sectional and prospective associations of actigraphy-assessed sleep regularity with metabolic abnormalities: the multi-ethnic study of atherosclerosis. Diabetes Care 42(8):1422–1429. https://doi.org/10.2337/dc19-0596
Paksarian D, Rudolph KE, Stapp EK, Dunster GP, He J, Mennitt D, Hattar S, Casey JA, James P, Merikangas KR (2020) Association of outdoor artificial light at night with mental disorders and sleep patterns among US adolescents. JAMA Psychiat 77(12):1266–1275. https://doi.org/10.1001/jamapsychiatry.2020.1935
Lee JA, Johns TS, Melamed ML, Tellechea L, Laudano M, Stern JM, Abraham NE (2020) Associations between socioeconomic status and urge urinary incontinence: an analysis of NHANES 2005 to 2016. J Urol 203(2):379–384. https://doi.org/10.1097/ju.0000000000000542
Yi X, Jin K, Qiu S, Xiong X, Zhang T, Peng G, Liao D, Zheng X, Xu H, Li H, Yang L, Wei Q, Ai J (2022) Phthalate exposure enhances incidence of urinary incontinence: US NHANES, 2003–2004 and 2005–2006. Environ Sci Pollut Res Int 29(43):64692–64703. https://doi.org/10.1007/s11356-022-20307-w
Branche BL, Howard LE, Moreira DM, Roehrborn C, Castro-Santamaria R, Andriole GL, Hopp ML, Freedland SJ (2018) Sleep problems are associated with development and progression of lower urinary tract symptoms: results from REDUCE. J Urol 199(2):536–542. https://doi.org/10.1016/j.juro.2017.08.108
Fantus RJ, Packiam VT, Wang CH, Erickson BA, Helfand BT (2018) The relationship between sleep disorders and lower urinary tract symptoms: results from the NHANES. J Urol 200(1):161–166. https://doi.org/10.1016/j.juro.2018.01.083
Fukunaga A, Kawaguchi T, Funada S, Yoshino T, Tabara Y, Matsuda F, Yoshimura K, Ogawa O, Negoro H (2019) Sleep disturbance worsens lower urinary tract symptoms: the nagahama study. J Urol 202(2):354. https://doi.org/10.1097/ju.0000000000000212
Araujo AB, Yaggi HK, Yang M, McVary KT, Fang SC, Bliwise DL (2014) Sleep related problems and urological symptoms: testing the hypothesis of bidirectionality in a longitudinal, population based study. J Urol 191(1):100–106. https://doi.org/10.1016/j.juro.2013.07.011
Koolhaas CM, Kocevska D, Te Lindert BHW, Erler NS, Franco OH, Luik AI, Tiemeier H (2019) Objectively measured sleep and body mass index: a prospective bidirectional study in middle-aged and older adults. Sleep Med 57:43–50. https://doi.org/10.1016/j.sleep.2019.01.034
Mishra GD, Hardy R, Cardozo L, Kuh D (2008) Body weight through adult life and risk of urinary incontinence in middle-aged women: results from a British prospective cohort. Int J Obes (Lond) 32(9):1415–1422. https://doi.org/10.1038/ijo.2008.107
Hannestad YS, Rortveit G, Daltveit AK, Hunskaar S (2003) Are smoking and other lifestyle factors associated with female urinary incontinence? The Norwegian EPINCONT study. BJOG 110(3):247–254
Danforth KN, Townsend MK, Lifford K, Curhan GC, Resnick NM, Grodstein F (2006) Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol 194(2):339–345. https://doi.org/10.1016/j.ajog.2005.07.051
Melville JL, Katon W, Delaney K, Newton K (2005) Urinary incontinence in US women: a population-based study. Arch Intern Med 165(5):537–542. https://doi.org/10.1001/archinte.165.5.537
Kupelian V, McVary KT, Kaplan SA, Hall SA, Link CL, Aiyer LP, Mollon P, Tamimi N, Rosen RC, McKinlay JB (2009) Association of lower urinary tract symptoms and the metabolic syndrome: results from the Boston Area Community Health Survey. J Urol 182(2):616–24. https://doi.org/10.1016/j.juro.2009.04.025. (Discussion 624–5)
Youngstedt SD, Kripke DF (2004) Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev 8(3):159–174. https://doi.org/10.1016/j.smrv.2003.10.002
Bennett LS, Barbour C, Langford B, Stradling JR, Davies RJ (1999) Health status in obstructive sleep apnea: relationship with sleep fragmentation and daytine sleepiness, and effects of continuous positive airway pressure treatment. Am J Respir Crit Care Med 159(6):1884–1890. https://doi.org/10.1164/ajrccm.159.6.9808107
Griffiths D, Clarkson B, Tadic SD, Resnick NM (2015) Brain mechanisms underlying urge incontinence and its response to pelvic floor muscle training. J Urol 194(3):708–715. https://doi.org/10.1016/j.juro.2015.03.102
Park GR, Park S, Kim J (2022) Urinary incontinence and depressive symptoms: the mediating role of physical activity and social engagement. J Gerontol B Psychol Sci Soc Sci 77(7):1250–1258. https://doi.org/10.1093/geronb/gbab212
Acknowledgements
This study was supported by the National Natural Science Foundation of China (Grant Nos. 81560419).
Author information
Authors and Affiliations
Contributions
CT: paper design and data processing. ZXP: data collection. XSC: draft of manuscript. FB: revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflict of interest.
Research involving human participants and animals
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, T., Zhan, X., Xiao, S. et al. U-shaped association between sleep duration and urgency urinary incontinence in women: a cross-sectional study. World J Urol 41, 2429–2435 (2023). https://doi.org/10.1007/s00345-023-04537-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04537-2