Abstract
Purpose
To report the 12-month results of a novel urethroplasty technique relying on a spiral preputial graft for panurethral stricture disease.
Materials and methods
Twenty consecutive patients were treated between May and October 2021 at our center. A spiral preputial mucocutaneous graft is a foreskin-based graft, developed from a 5-cm-wide preputial skin, which is harvested using a helicoidal shape and can reach up to 20 cm in length. Stricture characteristics were assessed through preoperative retrograde and voiding cystourethrogram and maximum uroflowmetry data (Qmax). Complications were collected up to 30 days after surgery and graded using the Clavien–Dindo (C–D) classification. The patients were followed up to 12 months.
Results
Preoperative median Qmax was 6.5 ml/s [interquartile range (IQR): 4.0–8.7]. After a median follow-up of 12 months (IQR 12–13), six patients experienced at least one complication. Of them, two patients had grade 2 C–D complications, while only one developed a grade 3a C–D complication. The median postoperative Qmax was 16 ml/s (IQR: 13–18). Only one patient had early urethral stricture recurrence treated with dilatation after catheter removal. At one-year follow-up, no other patients had urethral stricture recurrence with an overall median Qmax of 15.1 ml/s (IQR 13.5–16.4).
Conclusions
Our novel single-stage spiral preputial graft urethroplasty for panurethral stricture treatment appears to be safe and could be used as a valid alternative to two-stage procedures or even to single-stage buccal mucosa graft augmentation.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Campos-Juanatey F, Osman NI, Greenwell T, Martins FE, Riechardt S, Waterloos M et al (2021) European association of urology guidelines on urethral stricture disease (Part 2): diagnosis, perioperative management, and follow-up in males. Eur Urol 80:201–212. https://doi.org/10.1016/J.EURURO.2021.05.032
Lumen N, Campos-Juanatey F, Greenwell T, Martins FE, Osman NI, Riechardt S et al (2021) European association of urology guidelines on urethral stricture disease (Part 1): management of male urethral stricture disease. Eur Urol 80:190–200. https://doi.org/10.1016/J.EURURO.2021.05.022
Kulkarni S, Kulkarni J, Surana S, Joshi PM (2017) Management of panurethral stricture. Urol Clin North Am 44:67–75. https://doi.org/10.1016/J.UCL.2016.08.011
Kulkarni SB, Joshi PM, Venkatesan K (2012) Management of panurethral stricture disease in India. J Urol 188:824–830. https://doi.org/10.1016/J.JURO.2012.05.020
Basile G, Karakiewicz PI, Tian Z, Djinović R, Montorsi F, Barbagli G et al (2023) The impact of surgical volume on perioperative safety after urethroplasty: a population-based study. Min Urol Nephrol. https://doi.org/10.23736/S2724-6051.22.04893-5
McAninch JW (1993) Reconstruction of extensive urethral strictures: circular fasciocutaneous penile flap. J Urol 149:488–491. https://doi.org/10.1016/S0022-5347(17)36125-6
Quartey JKM (1983) One-stage penile/preputial cutaneous island flap urethroplasty for urethral stricture: a preliminary report. J Urol 129:284–287. https://doi.org/10.1016/S0022-5347(17)52051-0
Jaffar DJ, Sewell GR, Schwaarz FW (1956) Johanson urethroplasty for repair of urethral strictures. J Mich State Med Soc 55:299–302
Kulkarni S, Barbagli G, Sansalone S, Lazzeri M (2009) One-sided anterior urethroplasty: a new dorsal onlay graft technique. BJU Int 104:1150–1155. https://doi.org/10.1111/J.1464-410X.2009.08590.X
Zumrutbas AE, Ozlulerden Y, Celen S, Kucuker K, Aybek Z (2020) The outcomes of Kulkarni’s one-stage oral mucosa graft urethroplasty in patients with panurethral stricture: a single centre experience. World J Urol 38:175–181. https://doi.org/10.1007/S00345-019-02758-Y
Bandini M, Barbagli G, Leni R, Cirulli GO, Basile G, Balò S et al (2021) Assessing in-hospital morbidity after urethroplasty using the European Association of Urology Quality Criteria for standardized reporting. World J Urol 39:3921–3930. https://doi.org/10.1007/S00345-021-03692-8
Bandini M, Basile G, Lazzeri M, Montorsi F, Valli B, Balò S et al (2022) Optimizing decision-making after ventral onlay buccal mucosa graft urethroplasty failure. BJU Int. https://doi.org/10.1111/BJU.15895
Martin RCG, Brennan MF, Jaques DP (2002) Quality of complication reporting in the surgical literature. Ann Surg 235:803–813. https://doi.org/10.1097/00000658-200206000-00007
Mitropoulos D, Artibani W, Graefen M, Remzi M, Rouprêt M, Truss M (2012) Reporting and grading of complications after urologic surgical procedures: an ad hoc EAU guidelines panel assessment and recommendations. Eur Urol 61:341–349. https://doi.org/10.1016/j.eururo.2011.10.033
Mitropoulos D, Artibani W, Biyani CS, Bjerggaard Jensen J, Rouprêt M, Truss M (2018) Validation of the Clavien-Dindo grading system in urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur Urol Focus 4:608–613. https://doi.org/10.1016/J.EUF.2017.02.014
Joshi PM, Bandini M, Bafna S, Sharma V, Patil A, Bhadranavar S et al (2021) Graft plus fasciocutaneous penile flap for nearly or completely obliterated long bulbar and penobulbar strictures. Eur Urol Open Sci 35:21–28. https://doi.org/10.1016/J.EUROS.2021.10.009
Funding
None.
Author information
Authors and Affiliations
Contributions
SBK, PMJ, GB and MB were involved in protocol/project development. MB was involved in data collection or management.GB and MB analyzed the data and wrote and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Informed consent
No.
Research involving human participants and/or animals
No.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 312334 KB)
345_2023_4514_MOESM2_ESM.docx
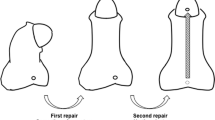
Supplementary file2 Supplementary Figure 1. Surgical steps of spiral preputial graft urethroplasty. A) After perineal invagination of the penis, a dorsal urethrotomy is created along the entire length of the urethral stricture until healthy tissue is encountered. B)The graft is created using a 5-cm-wide preputial skin, which is harvested using a helicoidal shape (DOCX 83 KB)
345_2023_4514_MOESM3_ESM.docx
Supplementary file3 Supplementary Figure 2. Surgical steps of spiral preputial graft urethroplasty. To create the spiral skin graft, two circumferential incisions were performed, the first 5 cm proximally in the outer preputial skin (A) and the second 5 mm below the coronal sulcus in the inner preputial mucosa (B) (DOCX 55 KB)
345_2023_4514_MOESM4_ESM.docx
Supplementary file4 Supplementary Figure 3. Surgical steps of spiral preputial graft urethroplasty. A)To facilitate the harvesting of the spiral preputial graft, the preputial mucocutaneous cylinder is placed around a 30cc syringe and fixed with two tourniquets on both extremities, which helped to stretch the cylinder itself B) The graft is anastomosed proximally at the level of the bulbo-membranous junction using three interrupted 4-0 polyglactin sutures. Then, the spiral graft is quilted to the corpora with three running sutures and anastomosed to the left margin of the native urethral plate. A continuous 4-0 polyglactin suture is to tabularize the neo-urethra by securing the corpus spongiosum to the lateral margin of the graft and the left corpus cavernosum (DOCX 61 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kulkarni, S.B., Joshi, P.M., Basile, G. et al. Novel single-stage preputial spiral graft for panurethral stricture: a step-by-step description of the technique. World J Urol 41, 2459–2463 (2023). https://doi.org/10.1007/s00345-023-04514-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04514-9