Abstract
Purpose
To compare the perioperative and postoperative outcomes between Oyster prostate vaporesection using Tm−YAG laser and the conventional transurethral prostatectomy using monopolar energy.
Methods
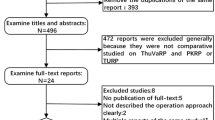
Patients with LUTS with an accumulative size of at least 60 ml were randomly assigned to one of two parallel groups to undergo Tm-YAG laser vaporesection (Group 1) or conventional monopolar transurethral prostatectomy (Group 2). The primary endpoints were the reduction in IPSS and the increase in Qmax postoperatively. Secondary endpoints included the Hemoglobin drop, the complication rate, the changes in urodynamic parameters, the duration of hospitalization and catheterization and the changes in IIEF during the 24-month follow-up.
Results
In total 32 and 30 patients were enrolled in Groups 1 and 2, respectively. Patient age (p = 0.422) and prostate volume were similar among the groups (p = 0.51). The outcomes in terms of IPSS decrease and Qmax amelioration were comparable (p = 0.449 and p = 0.237, respectively). Operative and hospitalization times were lower in Group 1 (p = 0.002 and p = 0.004, respectively). Hemoglobin drop, changes in urodynamic parameters and improvement in IIEF and QoL scores did not differ among the two Groups. The average time with the catheter was 2.06 ± 0.35 and 2.5 ± 0.82 (p = 0.003) days for Group 1 and Group 2, respectively. The overall complication rate was 6.2% for Group 1 and 13.3% for Group 2.
Conclusions
The Oyster technique leads to similar postoperative outcomes compared to the standard monopolar transurethral prostatectomy. The shorter catheterization, hospitalization and operation time should be considered advantages of the Oyster technique.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Robert G, De La Taille A, Descazeaud A (2018) Epidemiology of benign prostatic hyperplasia. Progres Urol: J Assoc Fr Urol Soc Fr Urol 28(15):803–812
Foo KT (2019) What is a disease? What is the disease clinical benign prostatic hyperplasia (BPH)? World J Urol 37(7):1293–1296
Gravas S, Gacci M, Gratzke C, Herrmann TRW, Mamoulakis C, Rieken M, Speakman MJ, Tikkinen KAO (2020) EAU guidelines on management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. Benign prostatic obstruction (BPO). EAU guidelines, pp 34–5
Ho HS, Yip SK, Lim KB, Fook S, Foo KT, Cheng CW (2007) A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. Eur Urol 52(2):517–522
Bach T, Muschter R, Sroka R, Gravas S, Skolarikos A, Herrmann TR et al (2012) Laser treatment of benign prostatic obstruction: basics and physical differences. Eur Urol 61(2):317–325
Deininger S, Herrmann T, Schönburg S, Törzsök P, Kunit T, Lusuardi L (2020) Surgical treatment of benign prostatic obstruction (BPO) in patients under anticoagulation: a review of the bleeding risks of established techniques. Der Urologe Ausg A 59(10):1187–1194
Bach T, Wendt-Nordahl G, Michel MS, Herrmann TR, Gross AJ (2009) Feasibility and efficacy of Thulium:YAG laser enucleation (VapoEnucleation) of the prostate. World J Urol 27(4):541–545
Bach T, Netsch C, Pohlmann L, Herrmann TR, Gross AJ (2011) Thulium:YAG vapoenucleation in large volume prostates. J Urol 186(6):2323–2327
Becker B, Orywal AK, Gross AJ, Netsch C (2019) Thulium vapoenucleation of the prostate (ThuVEP) for prostates larger than 85 ml: long-term durability of the procedure. Lasers Med Sci 34(8):1637–1643
Netsch C, Magno C, Butticè S, Macchione L, Mucciardi G, Herrmann TR et al (2016) Thulium Vaporesection of the prostate and thulium vapoenucleation of the prostate in patients on oral anticoagulants: a retrospective three-centre matched-paired comparison. Urol Int 96(4):421–426
Sener TE, Butticè S, Macchione L, Netsch C, Tanidir Y, Dragos L et al (2017) Thulium laser vaporesection of the prostate: Can we operate without interrupting oral antiplatelet/anticoagulant therapy? Investig Clin Urol 58(3):192–199
Carmignani L, Macchi A, Ratti D, Finkelberg E, Casellato S, Maruccia S et al (2015) One day surgery in the treatment of benign prostatic enlargement with thulium laser: a single institution experience. Korean J Urol 56(5):365–369
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bozzini G, Seveso M, Melegari S, de Francesco O, Buffi NM, Guazzoni G et al (2017) Thulium laser enucleation (ThuLEP) versus transurethral resection of the prostate in saline (TURis): a randomized prospective trial to compare intra and early postoperative outcomes. Actas Urol Esp 41(5):309–315
Peng B, Wang GC, Zheng JH, Xia SQ, Geng J, Che JP et al (2013) A comparative study of thulium laser resection of the prostate and bipolar transurethral plasmakinetic prostatectomy for treating benign prostatic hyperplasia. BJU Int 111(4):633–637
Cui D, Sun F, Zhuo J, Sun X, Han B, Zhao F et al (2014) A randomized trial comparing thulium laser resection to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: four-year follow-up results. World J Urol 32(3):683–689
Castellani D, Di Rosa M (2020) Thulium laser vapoenucleation of the prostate (ThuVEP) in men at high cardiovascular risk and on antithrombotic therapy: a single-center experience. J Clin Med 9(4):917
Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, Zhang YN (2008) Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol 53(2):382–389
Vargas C, Garcia-Larrosa A, Capdevila S, Laborda A (2014) Vaporization of the prostate with 150-w thulium laser: complications with 6-month follow-up. J Endourol 28(7):841–845
Feng L, Zhang D, Tian Y, Song J (2016) Thulium laser enucleation versus plasmakinetic enucleation of the prostate: a randomized trial of a single center. J Endourol 30(6):665–670
Yang Z, Liu T, Wang X (2016) Comparison of thulium laser enucleation and plasmakinetic resection of the prostate in a randomized prospective trial with 5-year follow-up. Lasers Med Sci 31(9):1797–1802
Enikeev D, Glybochko P, Rapoport L, Okhunov Z, O’Leary M, Potoldykova N et al (2018) Impact of endoscopic enucleation of the prostate with thulium fiber laser on the erectile function. BMC Urol 18(1):87
Tiburtius C, Knipper S, Gross AJ, Netsch C (2014) Impact of thulium vapoenucleation of the prostate on erectile function: a prospective analysis of 72 patients at 12-month follow-up. Urology 83(1):175–180
Morozov A, Taratkin M, Kozlov V, Tarasov A, Bezrukov E, Enikeev M et al (2020) Retrospective assessment of endoscopic enucleation of prostate complications: a single-center experience of more than 1400 patients. J Endourol 34(2):192–197
Rijo E, Misrai V, Aho T, Gomez-Sancha F (2018) Recommendations for safe and efficient morcellation after endoscopic enucleation of the prostate. Urology 121:197
Funding
None.
Author information
Authors and Affiliations
Contributions
DK—Data collection and data analysis, interpretation of data and manuscript drafting. VT—Data analysis, interpretation of data and manuscript drafting. AP—Data collection and data analysis. VT—Data analysis, interpretation of data. KP—Data collection and data analysis. PN—Data collection and data analysis. CA—Data analysis, interpretation of data. TV—Critical revision. EL—Project development and critical revision. PK—Project development and conception, critical revision.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
The study involves Humans Participants and has been carried out in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kotsiris, D., Tatanis, V., Peteinaris, A. et al. Outcomes of thulium prostatectomy with “Oyster technique” versus transurethral prostatectomy (TURP): a randomized control trial. World J Urol 41, 2473–2479 (2023). https://doi.org/10.1007/s00345-023-04510-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04510-z