Abstract
Purpose
Stress urinary incontinence (SUI) is a well-known adverse outcome following robotic-assisted laparoscopic prostatectomy (RALP). Although postoperative SUI has been extensively studied, little focus has been placed on understanding the natural history and impact of urgency symptoms following RALP. The UVA prostatectomy functional outcomes program (PFOP) was developed to comprehensively assess and optimize continence outcomes following RALP. The present study focuses on assessing urgency outcomes in this cohort.
Methods
PFOP patients with a minimum of 6-months follow up following RALP were included. The PFOP includes prospectively assessed incontinence and quality of life outcomes utilizing ICIQ-MLUTS, Urgency Perception Score (UPS), and IIQ-7 questionnaires. The primary study outcome was urgency urinary incontinence (UUI) as determined by ICIQ-MLUTS UUI domain. Secondary outcomes included urgency (UPS score) and quality of life (IIQ-7).
Results
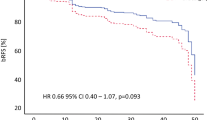
Forty patients were included with median age 63.5 years. Fourteen (35%) patients reported UUI at baseline. UUI and QOL scores worsened compared to baseline at all time-points. Urgency worsened at 3-weeks and 3-months but returned to baseline by 6-months. Notably, 63% of patients without baseline UUI reported de-novo UUI at 6 months. Although QOL was lower in patients with versus without UUI (IIQ-7 score 3.0 vs 0.0, p = 0.009), severity of UUI was not associated with QOL when controlling for SUI severity.
Conclusion
Our data demonstrate significantly worsened UUI from baseline and a large incidence of de-novo UUI following RALP. Further study is needed to inform how urgency and UUI and its treatment affect health-related quality of life following RALP.
Similar content being viewed by others
Data availability
Data information is available upon request.
References
Bauer RM et al (2011) Contemporary management of postprostatectomy incontinence. Eur Urol 59(6):985–996. https://doi.org/10.1016/j.eururo.2011.03.020
Stanford JL et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer the prostate cancer outcomes study. https://jamanetwork.com/
Hoyland K, Vasdev N (2014) Post–radical prostatectomy incontinence: etiology and prevention. ChM (Urol) 16(4):181–188. https://doi.org/10.3909/riu0606
Thiruchelvam N, Cruz F, Kirby M, Tubaro A, Chapple CR, Sievert KD (2015) A review of detrusor overactivity and the overactive bladder after radical prostate cancer treatment. BJU Int 116(6):853–861. https://doi.org/10.1111/bju.13078
Das AK, Kucherov V, Glick L and Chung P (2020) Male urinary incontinence after prostate disease treatment
Agarwal A et al (2014) What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women. Eur Urol 65(6):1211–1217. https://doi.org/10.1016/j.eururo.2014.01.019
Abrams P, Avery K, Gardener N, Donovan J (2006) The international consultation on incontinence modular questionnaire: www.iciq.net. J Urol 175(3):1063–1066. https://doi.org/10.1016/S0022-5347(05)00348-4
Cardozo L, Coyne KS, Versi E (2005) Validation of the urgency perception scale. BJU Int 95(4):591–596. https://doi.org/10.1111/j.1464-410X.2005.05345.x
Rosen R, Cappelleri J, Smith M, Lipsky J, Peña B (1999) Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 11(6):319–326. https://doi.org/10.1038/sj.ijir.3900472
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA (1994) Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Qual Life Res 3(5):291–306. https://doi.org/10.1007/BF00451721
Hosier GW, Tennankore KK, Himmelman JG, Gajewski J, Cox AR (2016) Overactive bladder and storage lower urinary tract symptoms following radical prostatectomy. Urology 94:193–197. https://doi.org/10.1016/j.urology.2016.05.007
Matsukawa Y et al (2018) De novo overactive bladder after robot-assisted laparoscopic radical prostatectomy. Neurourol Urodyn 37(6):2008–2014. https://doi.org/10.1002/nau.23556
Kan KM, Tin AL, Stearns GL, Eastham JA, Sjoberg DD, Sandhu JS (2022) De novo urinary storage symptoms are common after radical prostatectomy: incidence, natural history and predictors. J Urol 207(3):601–608. https://doi.org/10.1097/JU.0000000000002312
Ventimiglia B, Tsirgiotis A, Panzone I, Coco T, Privitera S (2011) Urinary incontinence after radical prostatectomy. Neurophysiological and urodynamic diagnosis. Urologia Journal 78(2):82–85. https://doi.org/10.5301/RU.2011.7975
Giannantoni A et al (2008) Bladder and urethral sphincter function after radical retropubic prostatectomy: a prospective long-term study. Eur Urol 54(3):657–664. https://doi.org/10.1016/j.eururo.2007.10.054
Leach GE, Trockman B, Wong A, Hamilton J, Haab F, Zimmern PE (1996) Post-prostatectomy incontinence: urodynamic findings and treatment outcomes. J Urol 155(4):1256–1259. https://doi.org/10.1016/S0022-5347(01)66235-9
Jung SY et al (1999) Urethral afferent nerve activity affects the micturition reflex; implication for the relationship between stress incontinence and detrusor instability. J Urol 162(1):204–212. https://doi.org/10.1097/00005392-199907000-00069
Castellani D et al (2022) Change in postoperative storage symptoms and de novo urge incontinence after Thulium: YAG laser enucleation of the prostate: results from a prospective multicenter study. J Endourol. https://doi.org/10.1089/end.2022.0118
Cho MC et al (2011) Predictor of de novo urinary incontinence following holmium laser enucleation of the prostate. Neurourol Urodyn. https://doi.org/10.1002/nau.21050
Coyne KS et al (2009) The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS
Funding
None.
Author information
Authors and Affiliations
Contributions
EHK—protocol/project development, data analysis, manuscript writing/editing. JZ—protocol/project development, data analysis, manuscript writing/editing. MA—protocol/project development, data analysis, manuscript writing/editing. DH—protocol/project development, data analysis. JF—protocol/project development, data analysis, data collection. AD—protocol/project development, data collection. DB—data collection. DER—protocol/project development, data analysis, manuscript writing/editing, data collection.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human participants
This study was approved by the UVA IRB (IRB-HSR #20830) and we certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kennady, E.H., Zillioux, J., Ali, M. et al. Longitudinal urgency outcomes following robotic-assisted laparoscopic prostatectomy. World J Urol 41, 1885–1889 (2023). https://doi.org/10.1007/s00345-023-04458-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04458-0