Abstract
Purpose
To evaluate the impact of COVID-19 pandemic on functional urology procedures in France.
Methods
A prospective study was conducted within 11 secondary and tertiary referral centers in France. Patients aged > 18 years who were diagnosed with a functional urology disease before the national lockdown (March 17th, 2020) and who required a surgery were included. Study period went from March 17th to September 30th 2020. The included interventions were listed according to the guidelines for functional urology enacted by the French Association of Urology and delay of reoperation was compared to the guidelines’ delay. The primary outcome was the number of procedures left unscheduled at the end of the study period. Descriptive statistics were performed.
Results
From March 17th 2020 to September 3 rd 2020, 1246 patients with a previous diagnosis of a functional urological disease requiring a surgery were included. The mean follow-up was 140.4 days (± 53.4). Overall, 316 interventions (25.4%) were maintained whereas 74 (5.9%) were canceled, 848 (68.1%) postponed and 8 patients (0.6%) died. At the end of the follow-up, 184 patients (21.7%) were still not rescheduled. If the intervention was postponed, the mean delay between the initial and final date was 85.7 days (± 64.4).
Conclusion
Overall, more than two thirds of interventions had to be postponed and the mean delay between the initial and final date was about three months.
Similar content being viewed by others
Introduction
Starting in Wuhan (Hubei, China) in December 2019, the coronavirus disease-2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread worldwide and was declared as a pandemic by the World Health Organization [1]. After Asian countries, Italy was hit, followed by other European countries, with an immense impact on local populations [2]. Because of the contagious nature of the virus and the lack of effective treatment, authorities of many countries were forced to impose total lockdown [3]. In France, lockdown was decreed from March 17th 2020. Non-urgent interventions began to be postponed to this date.
The whole healthcare system has been massively impacted to accommodate COVID-19 patients [4]. Telemedicine, including outpatient clinics and virtual boards, have been increasingly and quickly developed, staying however irrelevant for surgery [5].
As the decision to maintain a surgical intervention can place the patient and/or health care workers at risk of infection with Sars-CoV-2, each surgery should be approached with consideration [6]. This new disease has changed urology practice in most countries around the world. In this context, the French Association of Urology has published recommendations to help clinicians to prioritize surgeries, including functional procedures [7]. Hence, guidelines were provided to manage patients affected by urological cancers to avoid significant delays that could have important impact on patient outcomes [8]. Regarding the field of functional urology, including urinary incontinence, prolapse, lower urinary tract symptoms, reconstructive urology and neuro-urology, the majority of surgical procedures were considered as being non-urgent although they could sometimes lead to an infectious or renal failure risk with a detrimental impact on quality of life and mental health. Consequently, functional, benign, and pelvic floor conditions have often been considered suitable for delay in challenging times. However, the long-term implications of this reduction in functional urology clinical activity are currently unknown. We decided to conduct a multicentric study to evaluate the impact of COVID-19 pandemic on functional urological procedures in France 6 months after the start of the first lockdown.
Patients and methods
Study design
This was a prospective observational and multicenter study conducted during the first lockdown within 11 centers in France, among secondary and tertiary settings, under the umbrella of neuro-urology, male LUTS and female pelvic floor scientific committees of the French Association of Urology (AFU: Association Française d’Urologie).
Inclusion criteria
Patients aged > 18 years who were diagnosed with a functional urology disease (urinary incontinence, prolapse, LUTS, neuro-urology) before the lockdown (March 17th 2020) and for whom a surgical procedure was planned were included.
The study period went from March 17th 2020 to September 30th 2020. Patients who were diagnosed secondarily with a functional urology disease during the study period were excluded.
The included interventions (see above) were listed according to the guidelines for functional urology enacted by the French Association of Urology [9] and were classified as follows:
-
Priority level A: intervention must not be postponed (conclusion of a neuromodulation test in progress -implantation or explantation, botulinum toxin A bladder injections for high-risk neurogenic bladder, cystectomy and ileal conduit for urinary fistula in perineal bedsore or refractory high-risk neurogenic bladder with acute renal failure or vesico-enteric or prostato-pubic fistulas).
-
Priority level B: intervention should be rescheduled within eight weeks (treatment of benign hypertrophy of prostatic with complications such as urinary retention, bladder stones or renal failure).
-
Priority level C: intervention should be postponed and rescheduled between eight to sixteen weeks (sphincterotomy, augmentation cystoplasty, continent urinary diversion, cystectomy and ileal conduit for neurogenic bladder, treatment of urethral or ureteral stricture, treatment of severe urinary incontinence, treatment of severe pelvic organ prolapse).
-
Priority level D: intervention should be canceled, and clinical reevaluation should be performed before rescheduling, after sixteen weeks (treatment of benign prostatic hypertrophy without complications, treatment of urinary incontinence, treatment of genital prolapse).
The following data were collected: center’s name, age, comorbities, Covid-19 status, urological diagnosis and planned surgical procedure, type of anesthesia (local, loco-regional or general), setting (inpatient or outpatient), delay between initial and final dates of operation, last follow-up date and eventually date of death when appropriate).
Outcomes
The primary outcome the number of procedures left unscheduled at the end of the study period, The secondary outcomes were the mean delay between the initial date of intervention and the actual date of the surgery, the number and types of canceled interventions, the number of deaths and types of modifications of medical cares.
Statistical analyses
All analyses were performed using an R statistical package (R version 4.1.0).
The statistics were mainly descriptive (measures of central tendency, measures of dispersion).
Results
Population
From March 17th 2020 to September 30th 2020, 1246 patients, mean age was 58.8 years (± 16.8), with a previous diagnosis of a urological functional disease requiring a surgery were included. Among them, 4 patients (0.3%) were diagnosed positive for COVID-19 whereas 402 (32.2%) were negative and 850 (67.5%) were not tested. There were 724 (58.1%) male patients and 522 female patients (41.9%) which corresponded to a sex ratio of 1.39 (M/F).
Interventions
Interventions were scheduled under local (424–30.0%) or general (822–70.0%) anesthesia. They were planned as inpatient (568–45.6%) or outpatient (678–54.4%) procedures. According to the recent guidelines of the French Association of Urology [9], 153 interventions (12.3%) were classified as priority A, 84 (6.7%) as priority B, 426 (34.2%) as priority C and 583 (46.8%) as priority D. Intensive Care Unit Requirement were planned for 44 of them (2.7%). Surgeries’ characteristics are summarized in Table 1.
Patients’ pathways
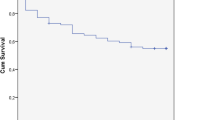
The mean follow-up was 140.4 days (± 53.4). Overall, 316 interventions (25.4%) were maintained whereas 74 (5.9%) were canceled, 848 (68.1%) postponed and 8 patients (0.6%) died. 113 procedures performed under local anesthesia were maintained (26.6%) whereas 138 outpatient operations were maintained (20.4%). Death causes were not related to COVID-19 but to the general health conditions of the patients. If the intervention was postponed, the mean delay between the initial and final date was 85.7 days (± 64.4). For procedures under local anesthesia, the mean delay was 62.6 days (± 65.7) and 79.2 days (± 68.5) for patients who underwent outpatient pathway. At the end of follow-up, 184 (21.7%) patients had not been operated whereas 664 (78.3%) had undergone the planned procedure. The Fig. 1 and Table 2 represent the patients’ pathway. No complications were reported because of the intervention postponement and no deaths were directly linked to COVID-19.
Discussion
The present study highlights the huge impact of the COVID-19 pandemic on the functional urology procedures in France including 74% of them being postponed or canceled. Among these procedures, 21.7% are still not rescheduled.
Since COVID-19 was declared a pandemic, a rich literature have rapidly emerged with guidelines and recommendations in the different fields of surgery [10]. The main messages were to prepare for a rapidly evolving situation, to postpone elective operations, to develop plan for essential operations during the pandemic, to educate surgical staff on personal protective equipment and to decrease exposure of health care staff.
In this perspective, non-urgent procedures were stopped to reallocate nurses (anesthetists nurses and operating room nurses) and anesthesiologists. These measures are allowed to freed ventilators for patients with COVID-19 and converted surgical theatres into additional intensive care unit beds [11]. It was also necessary to free up intensive care beds from planned surgery.
In our study, in accordance with national guidelines [9], the mean delay to reschedule an intervention was 85.7 days (12.4 weeks). Indeed, most of the guidelines endowed 1 to 3-month delays for elective and non-urgent operations [12]. Moreover, 46% of procedures were classified rank D therefore schedulable to more than 4 months.
Actually, no complications were reported because of the intervention postponement and no death was directly linked to COVID-19. In other words, the imposed delay did not worsen clinical conditions of patients at this stage. Even if we did not record any complications, the impact of quality of life and the psychological repercussions are certain even if difficult to assess.
In all the treatment schemes proposed in the literature on the COVID-19 pandemic, functional urology surgery is not adequately covered and usually grouped into the category that is not urgent or can be delayed, but in a sustained pandemic scenario there are cases that cannot be delayed that should be considered for surgery as a priority [13]. In the, oncological surgery field, potential second mortality rebound in populations have been reported. Indeed, because of the lockdown, many patients could have neglected their symptoms or failed to consult a physician due to fear, resulting in advanced disease at diagnosis with less treatment options [14]. Focusing on pelvic floor dysfunction area, Sacco et al. reported a cancellation of 78.4% of outpatient services and 82.7% of functional surgeries, without significant differences by geographical distribution. However, an impact on patients' quality of life was anticipated by most of the respondents of the surveys (87%) and 48.2% also reported potentially serious health risks for patients.
In addition, clinicians are now facing huge challenges: catching up on canceled/postponed operations, maintaining optimal healthcare access and preventing further waves of COVID-19. Moreover, even with the progressive end of the lockdown, the global effect of the COVID-19 pandemic will probably last for some time during which national health systems will have to treat COVID-19 and non-COVID-19 patients simultaneously. Therefore, functional urology units will have to reorganize their activity according to patient priority and the scope of the pandemic in each area. An international, multicenter, prospective cohort study included patients undergoing elective or emergency surgery during the pandemic, showed that surgery should be delayed for at least 7 weeks following SARS-CoV-2 infection. Patients with ongoing symptoms ≥ 7 weeks from diagnosis may benefit from further delay [15]. Patients still not rescheduled after 6 months, have to be re-evaluated before undergoing surgery to detect any changing in their conditions. The authors also hypothesized that if the Italy‐wide surgical activity increases by 20% post-pandemic, it would take 37 months to clear the backlog of functional surgeries [16]. A huge accumulated work load should be anticipated, not to mention the major financial issues with COVID-19 pandemic [17]. Most often, it is not possible to increase the number of operative shifts. Thus, the accumulated delay cannot be made up for. The 21% of patients who were not scheduled at the end of the study were scheduled in the following months at the expense of other patients who experienced an increased delay for treatment. Moreover, there are certain “functional” procedures which are in reality life-threatening such as neurological bladder of spinal cord injured patients or unbalanced spina bifida with renal failure, which are often unrecognized and neglected.
The decision to postpone an invasive procedure is driven by a case-by-case discussion. Therefore, postponed patients have to be carefully monitored to provide when possible, the standard of care for their conditions after resolution of the crisis. It is essential to keep the traceability of all information exchanged on the patients during the whole period and make these available for future questioning about possible direct or indirect consequences and that what we aimed to provide in the present study. To face the post-epidemic phase, the way to resume progressively our activities has be anticipated now to avoid overwhelming due to complicated, rescheduled and new patients. In this reflexion, the pathway of outpatient setting may be privileged. Indeed, operations under local anesthesia and/or outpatient surgeries consume little hospital and human resources. They are also low risk of complications and should be maintained to limit delays, deterioration of quality of life and loss of opportunity for patients. In a long-term crisis perspective, these operations should be preserved from massive cancelations.
Our study has several limitations including the lack of patient‐reported quality of life outcomes in case of postponed/cancelation of procedures and the short follow-up. However, a study is ongoing until the end of the crisis.
Conclusions
The current situation leads to major disturbances regarding patient care in the field of functional urology. The long-term implications of this reduction in functional urology clinical activities are still unknown.
Overall, more than two thirds of interventions had to be postponed and the mean delay between the initial and final date was about three months. However, for 22% of patients who had their surgery postponed at the first lockdown, the procedure has not yet been rescheduled.
Efforts should be made to minimize the burden for this patient group without endangering patients and health care workers. Finally, a comprehensive and in-depth analysis of what worked and what failed during these exceptional circumstances will be necessary, hopefully in the coming months, to draw the lessons and anticipate any further shortage in healthcare resources.
References
World Health Organisation (WHO). Coronavirus disease (COVID-19) outbreak webpage. mars 2020; Disponible sur: https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd
Pellino G, Spinelli A (2020) How coronavirus disease 2019 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum 63:720–722
Tabourin T, Sarfati J, Pinar U, Beaud N, Parra J, Vaessen C et al (2020) Postoperative assessment of nosocomial transmission of COVID-19 after robotic surgical procedures during the pandemic. Urol Oncol. https://doi.org/10.1016/j.urolonc.2020.09.008
Pinar U, Anract J, Perrot O, Tabourin T, Chartier-Kastler E, Parra J et al (2020) Preliminary assessment of patient and physician satisfaction with the use of teleconsultation in urology during the COVID-19 pandemic. World J Urol 39:1991–1996
Chesnel C, Hentzen C, Le Breton F, Turmel N, Tan E, Haddad R et al (2021) Efficiency and satisfaction with telephone consultation of follow-up patients in neuro-urology: Experience of the COVID-19 pandemic. Neurourol Urodyn 40:929–937
Steward JE, Kitley WR, Schmidt CM, Sundaram CP (2020) Urologic surgery and COVID-19: How the pandemic is changing the way we operate. J Endourol 34:541–549
Méjean A, Rouprêt M, Rozet F, Bensalah K, Murez T, Game X et al (2020) Recommendations CCAFU on the management of cancers of the urogenital system during an epidemic with Coronavirus COVID-19. Prog Urol 30:221–231
Ribal MJ, Cornford P, Briganti A, Knoll T, Gravas S, Babjuk M et al (2020) European association of urology guidelines office rapid reaction group: an organisation-wide collaborative effort to adapt the european association of urology guidelines recommendations to the coronavirus disease 2019 Era. Eur Urol 78:21–28
Michel F, Gaillet S, Cornu JN, Robert G, Game X, Phé V et al (2020) French association of urology. COVID-19: recommendations for functional urology. Prog Urol 30:414–425
Elizabeth Brindle M, Gawande A (2020) Managing COVID-19 in surgical systems. Ann Surg 272:e1-2
Spinelli A, Pellino G (2020) COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 107:785–787
Heldwein FL, Loeb S, Wroclawski ML, Sridhar AN, Carneiro A, Lima FS et al (2020) A systematic review on guidelines and recommendations for urology standard of care during the COVID-19 pandemic. Eur Urol Focus 6:1070–1085
Hojaij FC, Chinelatto LA, Boog GHP, Kasmirski JA, Lopes JVZ, Sacramento FM (2020) Surgical practice in the current COVID-19 pandemic: a rapid systematic review. Clinics (Sao Paulo) 75:e1923
Gomolin T, Cline A, Handler MZ (2020) The danger of neglecting melanoma during the COVID-19 pandemic. J Dermatol Treat 31:444–445
COVIDSurg Collaborative, GlobalSurg Collaborative (2021) Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anesthesia
Magnavita N, Chirico F, Sacco A (2021) COVID-19: from hospitals to courts. Lancet 397:1542
Khullar D, Bond AM, Schpero WL (2020) COVID-19 and the financial health of US hospitals. JAMA 323:2127–2128
Author information
Authors and Affiliations
Contributions
CG-T: Project development / Data collection / Data analysis / Manuscript writing. GR: Manuscript writing. AR: Manuscript writing. XG: Manuscript writing. AB: Data collection. TC: Data collection. PVC: Data collection. JS: Data collection. MB Data collection. RF: Data collection. PLD: Data collection. SD: Data collection. CJ: Data collection. LV: Data collection. VA: Data collection. PL: Data collection / Manuscript writing. MAP-V: Manuscript writing. BP: Manuscript writing. XB: Manuscript writing. JNC: Manuscript writing. GK: Manuscript writing. VP: Project development / Manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Research involving Human Participants and/or Animals
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guillot-Tantay, C., Robert, G., Ruffion, A. et al. Impact of COVID-19 pandemic on functional urology procedures in France: a prospective study. World J Urol 40, 277–282 (2022). https://doi.org/10.1007/s00345-021-03821-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03821-3