Abstract
Purpose
There is sparse evidence on outcomes of resected occult LN metastases at the time of nephrectomy (synchronous disease). We sought to analyse a large international cohort of patients and to identify clinico-pathological predictors of long-term survival.
Materials and methods
We collected data of consecutive patients who underwent nephrectomy and LND for Tany cN0-1pN1 and cM0-1 RCC at 7 referral centres between 1988 and 2019. Patients were stratified into four clinico-pathological groups: (1) cN0cM0-pN1, (2) cN1cM0-pN1(limited, 1–3 positive nodes), (3) cN1cM0-pN1(extensive, > 3 positive nodes), and (4) cM1-pN1. Overall survival (OS) was estimated using the Kaplan–Meier method, and associations with all-cause mortality (ACM) were evaluated using Cox models with multiple imputations.
Results
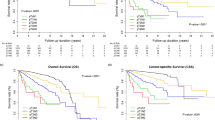
Of the 4370 patients with LND, 292 patients with pN1 disease were analysed. Median follow-up was 62 months, during which 171 patients died. Median OS was 21 months (95% CI 17–30 months) and the 5-year OS rate was 24% (95% CI 18–31%). Patients with cN0cM0-pN1 disease had a median OS of 57 months and a 5-year OS rate of 43%. 5-year OS (median OS) decreased to 29% (33 months) in cN1cM0-pN1(limited) and to 23% (23 months) in cN1cM0-pN1(extensive) patients. Those with cM1-pN1 disease had the worst prognosis, with a 5-year OS rate of 13% (9 months). On multivariable analysis, age (p = 0.034), tumour size (p = 0.02), grade (p = 0.02) and clinico-pathological group (p < 0.05) were significant predictors of ACM.
Conclusion
Depending on clinico-pathological group, grade and tumour size, 5-year survival of patients with LN metastases varies from 13 to 43%. Patients with resected occult lymph node involvement (cN0/pN1 cM0) have the best prognosis with a considerable chance of long-term survival.

Similar content being viewed by others
References
Chandrasekar T, Klaassen Z, Goldberg H et al (2017) Metastatic renal cell carcinoma: patterns and predictors of metastases-a contemporary population-based series. Urol Oncol 35(11):661.e7-661.e14
Bhindi B, Wallis CJD, Boorjian SA et al (2018) The role of lymph node dissection in the management of renal cell carcinoma: a systematic review and meta-analysis. BJU Int 121(5):684–698
Delacroix SE Jr, Chapin BF, Chen JJ et al (2011) Can a durable disease-free survival be achieved with surgical resection in patients with pathological node positive renal cell carcinoma? J Urol 186:1236–1241
Gershman B, Moreira DM, Thompson RH et al (2017) Renal cell carcinoma with isolated lymph node involvement: long-term natural history and predictors of oncologic outcomes following surgical resection. Eur Urol 72:300–306
Canfield SE, Kamat AM, Sanchez-Ortiz RF et al (2006) Renal cell carcinoma with nodal metastases in the absence of distant metastatic disease (clinical stage TxN1-2M0): the impact of aggressive surgical resection on patient outcome. J Urol 175:864–869
Leibovich BC, Lohse CM, Cheville JC et al (2018) Predicting oncologic outcomes in renal cell carcinoma after surgery. Eur Urol 73(5):772–780
Rieken M, Boorjian SA, Kluth LA et al (2019) Development and external validation of a pathological nodal staging score for patients with clear cell renal cell carcinoma. World J Urol 37(8):1631–1637
Leibovich BC, Lohse CM, Cheville JC, Zaid HB, Boorjian SA, Frank I, Thompson RH, Parker WP (2018) Predicting oncologic outcomes in renal cell carcinoma after surgery. Eur Urol 73(5):772–780
Rosiello G, Palumbo C, Knipper S et al (2020) Histotype predicts the rate of lymph node invasion at nephrectomy in patients with nonmetastatic renal cell carcinoma. Urol Oncol 38:537–544
Blom JH, van Poppel H, Marechal JM et al (2009) Radical nephrectomy with and without lymph-node dissection: final results of European Organization for Research and Treatment of Cancer (EORTC) randomized phase 3 trial 30881. Eur Urol 55:28–34
Bacic J, Liu T, Thompson RH et al (2020) Emulating target clinical trials of radical nephrectomy with or without lymph node dissection for renal cell carcinoma. Urology 140:98–106
Ljungberg B, Albiges L, Abu-Ghanem Y et al (2019) European Association of Urology guidelines on renal cell carcinoma: the 2019 update. Eur Urol 75(5):799–810
Escudier B, Porta C, Schmidinger M, Rioux-Leclercq N et al (2019) Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 30(5):706–720
Motzer RJ, Jonasch E, Agarwal N et al (2015) Kidney cancer, version 3.2015. J Natl Compr Canc Netw 13(2):151–159
Campbell S, Uzzo RG, Allaf ME et al (2017) Renal mass and localized renal cancer: AUA guideline. J Urol 198(3):520–529
Pantuck AJ, Zisman A, Dorey F et al (2003) Renal cell carcinoma with retroperitoneal lymph nodes: role of lymph node dissection. J Urol 169:2076–2083
Whitson JM, Harris CR, Reese AC et al (2011) Lymphadenectomy improves survival of patients with renal cell carcinoma and nodal metastases. J Urol 185:1615–1620
Karakiewicz PI, Trinh QD, Bhojani N et al (2007) Renal cell carcinoma with nodal metastases in the absence of distant metastatic disease: prognostic indicators of disease-specific survival. Eur Urol 51:1616–1624
Capitanio U, Suardi N, Matloob R et al (2014) Extent of lymph node dissection at nephrectomy affects cancer-specific survival and metastatic progression in specific sub-categories of patients with renal cell carcinoma (RCC). BJU Int 114:210–215
Golijanin B, Pereira J, Mueller-Leonhard C et al (2019) The natural history of renal cell carcinoma with isolated lymph node metastases following surgical resection from 2006 to 2013. Urol Oncol 37(12):932–940
Kuusk T, Zondervan P, Lagerveld B et al (2020) Topographic distribution of first landing sites of lymphatic metastases from patients with renal cancer. Urol Oncol 38(5):521–525
Sobin LH, Gospodarowicz MK, Wittekind C (2009) TNM Classification of Malignant Tumours, 7th edn. Wiley-Blackwell, Chichester, pp 255–257
White IR, Royston P (2009) Imputing missing covariate values for the Cox model. Stat Med 28:1982–1998
Marshall A, Altman DG, Holder RL et al (2009) Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines. BMC Med Res Methodol 9:57
Belsante M, Darwish O, Youssef R et al (2014) Lymphovascular invasion in clear cell renal cell carcinoma-association with disease-free and cancer-specific survival. Urol Oncol 32(1):30.e23–8
Yu KJ, Keskin SK, Meissner MA et al (2018) Renal cell carcinoma and pathologic nodal disease: Implications for American Joint Committee on Cancer staging. Cancer 124(20):4023–4031
Zareba P, Russo P (2019) The prognostic significance of nodal disease burden in patients with lymph node metastases from renal cell carcinoma. Urol Oncol 37(5):302.e1-302.e6
Terrone C, Cracco C, Porpiglia F et al (2006) Reassessing the current TNM lymph node staging for renal cell carcinoma. Eur Urol 49(2):324–331
Trinh QD, Schmitges J, Bianchi M et al (2012) Node-positive renal cell carcinoma in the absence of distant metastases: predictors of cancer-specific mortality in a population-based cohort. BJU Int 110:E21–E27
Bex A, Vermeeren L, de Windt G et al (2010) Feasibility of sentinel node detection in renal cell carcinoma: a pilot study. Eur J Nucl Med Mol Imaging 37(6):1117–1123
Kuusk T, De Bruijn R, Brouwer OR et al (2018) Lymphatic drainage from renal tumors in vivo: a prospective sentinel node study using SPECT/CT imaging. J Urol 199(6):1426–1432
Verhoeff SR, van Es SC, Boon E et al (2019) Lesion detection by [89Zr]Zr-DFO-girentuximab and [18F]FDG-PET/CT in patients with newly diagnosed metastatic renal cell carcinoma. Eur J Nucl Med Mol Imaging 46(9):1931–1939
Funding
No funds, grants, or other support was received. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
TK: protocol/project development, data collection or management and manuscript writing/editing. TK: data analysis and manuscript writing/editing. PZ: data collection or management and manuscript writing/editing. BL: data collection or management and manuscript writing/editing. NG: data collection or management and manuscript writing/editing. KH: data collection or management and manuscript writing/editing. UC: data collection or management and manuscript writing/editing. AM: data collection or management and manuscript writing/editing. DGS: data collection or management and manuscript writing/editing. BL: data collection or management and manuscript writing/editing. SH: data collection or management, manuscript writing/editing. AB: protocol/project development, data collection or management and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kuusk, T., Klatte, T., Zondervan, P. et al. Outcome after resection of occult and non-occult lymph node metastases at the time of nephrectomy. World J Urol 39, 3377–3383 (2021). https://doi.org/10.1007/s00345-021-03633-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03633-5