Abstract
Objectives
To evaluate three subtypes of continent-cutaneous urinary diversion (CCUD); Indiana pouch (IP), right colon pouch with appendico-umbilicostomy (AU), and right colon pouch with neo-appendico-umbilicostomy (NAU), by investigating diversion-specific complications and quality-of-life outcomes.
Materials and methods
A retrospective review of an IRB-approved database was conducted for perioperative and outcome data. The EORTC QLQ-C30 questionnaire was used to assess quality of life; all responses were obtained > 6 months after diversion.
Results
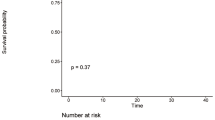
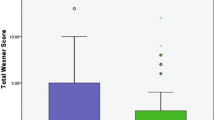
Fifty-eight patients who underwent a CCUD at our institution from 2010 to 2016 (33 IP by two surgeons, 15 AU and ten NAU by third surgeon) were identified for this study. Higher age and Charlson Comorbidity Index (CCI) ≥ 3 were seen in the AU cohort when compared to the IP cohort (P = 0.02 and 0.02, respectively). NAU group were also older when compared to the IP group (P = 0.02). After a median follow-up of 21 months (range: 0.8–81.0), more high-grade diversion-related complications were reported for AU and NAU patients comparing to the IP group (P < 0.01 and P = 0.02, respectively). More stoma complications were also reported for the NAU cohort than the IP cohort (70% vs 30%, P = 0.03). In all groups, > 60% of stoma complications occurred at the skin or fascia level. In the 90-day postoperative period, a higher continence rate was reported for the IP cohort, and this difference was significant when compared to the NAU cohort (P = 0.04). Length of stay after surgery and revision rates were not significantly different. For all groups, the majority of patients reported little-to-no disturbance of daily functions and rated overall quality of life as good-to-excellent.
Conclusion
Urinary diversion using the Indiana pouch and right colon pouch with appendico/neo-appendico-umbilicostomy are all associated with high rates of continence and patient satisfaction. When compared to IP, AU and NAU patients had higher rates of high-grade diversion-related complications and NAU patients had a higher stoma complications with lower 90-day continence rate.


Similar content being viewed by others
References
Rink M, Kluth L, Eichelberg E, Fisch M, Dahlem R (2010) Continent catheterizable pouches for urinary diversion. Eur Urol Suppl 9(10):754–762
Lee RK, Abol-Enein H, Artibani W et al (2014) Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int 113(1):11–23
Pearce SM, Daneshmand S (2018) Continent cutaneous diversion. Urol Clin N Am 45(1):55–65
Stein JP, Daneshmand S, Dunn M, Garcia M, Lieskovsky G, Skinner DG (2004) Continent right colon reservoir using a cutaneous appendicostomy. Urology 63(3):577–580
Wagner M, Bayne A, Daneshmand S (2008) Application of the Yang-Monti channel in adult continent cutaneous urinary diversion. Urology 72(4):828–831
Rowland RG, Mitchell ME, Bihrle R, Kahnoski RJ, Piser JE (1987) Indiana continent urinary reservoir. J Urol 137(6):1136–1139
Rowland RG, Kropp BP (1994) Evolution of the Indiana continent urinary reservoir. J Urol 152(6 Part 2):2247–2251
Riedmiller H, Bürger R, Müller S, Thüroff J, Hohenfellner R (1990) Continent appendix stoma: a modification of the Mainz pouch technique. J Urol 143(6):1115–1117
Myers JB, Lenherr SM (2016) Perioperative and long-term surgical complications for the Indiana pouch and similar continent catheterizable urinary diversions. Curr Opin Urol 26(4):376–382
Castillo OA, Aranguren G, Campos-Juanatey F (2014) Indiana continent catheterizable urinary reservoir. Actas Urol Esp 38(6):413–418
Holmes DG, Thrasher JB, Park GY, Kueker DC, Weigel JW (2002) Long-term complications related to the modified Indiana pouch. Urology 60(4):603–606
Gerharz EW, Roosen A, Månsson W (2005) Complications and quality of life following urinary diversion after cystectomy. EAU Update Ser 3(3):156–168
Lemelle JL, Simo AK, Schmitt M (2004) Comparative study of the Yang-Monti channel and appendix for continent diversion in the Mitrofanoff and Malone principles. J Urol 172(5):1907–1910
Nazmy M, Yuh B, Kawachi M et al (2014) Early and late complications of robot-assisted radical cystectomy: a standardized analysis by urinary diversion type. J Urol 191(3):681–687
Monn MF, Kaimakliotis HZ, Cary KC et al (2014) Short-term morbidity and mortality of Indiana pouch, ileal conduit, and neobladder urinary diversion following radical cystectomy. Urol Oncol 32(8):1151–1157
Skinner EC (2015) Continent cutaneous diversion. Curr Opin Urol 25(6):555–561
Yang LS, Shan BL, Shan LL et al (2016) A systematic review and meta-analysis of quality of life outcomes after radical cystectomy for bladder cancer. Surg Oncol 25(3):281–297
Gerharz EW, Månsson Å, Hunt S, Skinner EC, Månsson W (2005) Quality of life after cystectomy and urinary diversion: an evidence based analysis. J Urol 174(5):1729–1736
Large M, Katz M, Shikanov S, Eggener S, Steinberg G (2010) orthotopic neobladder versus Indiana pouch in women. J Urol 183(1):201–206
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
KWC: data collection or management, data analysis, and manuscript writing/editing. WY: data analysis and manuscript writing/editing. AS: data analysis and manuscript writing/editing. LGM: data analysis and manuscript writing/editing. AG: data analysis and manuscript writing/editing. GM: data collection or management, critical review, and supervision. AS: protocol/project development and manuscript writing/editing. SD: protocol/project development and manuscript writing/editing. HD: protocol/project development, data analysis, and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheng, K.W., Yip, W., Shah, A. et al. Stoma complications and quality of life in patients with Indiana pouch versus appendico/neo-appendico-umbilicostomy urinary diversions. World J Urol 39, 1521–1529 (2021). https://doi.org/10.1007/s00345-020-03348-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03348-z