Abstract
Purpose
To determine if patients can accurately estimate volumes voided in a bladder diary, and to determine the patient characteristics that are most predictive of accuracy in volume estimation in the workup of lower urinary tract symptoms (LUTs).
Methods
We prospectively collected data on 180 consecutive patients undergoing a workup for LUTs at a tertiary care facility. Data collected include American Urological Association Symptom Scores (AUASS), flow time and rate, and one time measurement of voided volume into a blinded uroflow. Baseline characteristics and demographics were recorded. Descriptive statistics and linear regression analysis were performed to examine predictors of estimated voiding volume (mL) in SAS Version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
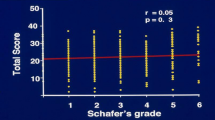
Median age and BMI were 64 years (SD = 15.4) and 26.9 kg/m2 (SD = 4.6), respectively. The median estimated voided volume and actual voided volume were 120 mL (range 1–480) and 101.5 mL (range 6.5–622.0), respectively. On linear regression analysis, 47.1% of patients estimated volume voided with a 20% margin of error, and 63.2% of patients estimated with a 30% margin of error. Each 1-year increase in age correlated with a 2% decrease in the odds of estimating voided volume within 20% of actual volume (p < 0.05). For each 1 unit increase in flow rate, there was an 8% (p < 0.005) increase in the odds of estimating voided volume within 20% of actual volume.
Conclusions
Just under half of patients can accurately estimate volume voided with a margin of error of 20%.
Similar content being viewed by others
References
Bright E, Drake MJ, Abrams P (2011) Urinary diaries: evidence for the development and validation of diary content, format, and duration. Neurourol Urodyn 30(3):348–352. https://doi.org/10.1002/nau.20994
Pauls RN, Hanson E, Crisp CC (2015) Int Urogynecol J 26:91. https://doi.org/10.1007/s00192-014-2470-2
Colley W (2015) Use of frequency volume charts and voiding diaries. Nurs Times. 111(5):12–16. www.nursingtimes.net. Accessed Nov 2018
Arya LA, Banks C, Gopal M et al (2008) Development and testing of a new instrument to measure fluid intake, output, and urinary symptoms: the questionnaire-based voiding diary. Am J Obstet Gynecol 198:559.e1–559.e7
Elmer C, Murphy A, Elliott JO, Book NM (2017) Twenty-four–hour voiding diaries versus 3-day voiding diaries: a clinical comparison. Female Pelvic Med Reconstr Surg 23(6):429–432. https://doi.org/10.1097/spv.0000000000000412
Ku JH, Jeong IG, Lim DJ, Byun S, Paick J, Oh S (2004) Voiding diary for the evaluation of urinary incontinence and lower urinary tract symptoms: prospective assessment of patient compliance and burden. Neurourol Urodyn 23:331–335. https://doi.org/10.1002/nau.20027
Chiang C, Fan Y, Lin AT, Chen K (2014) First morning voided volume as a valuable tool for evaluating patients with overactive bladder. Urol Sci 25(3):79–82. https://doi.org/10.1016/j.urols.2014.03.002
Blaivas JG, Tsui JF, Amirian M, Ranasinghe B, Weiss JP, Haukka J, Tikkinen KAO (2014) Relationship between voided volume and the urge to void among patients with lower urinary tract symptoms. Scand J Urol. 48:6. https://doi.org/10.3109/21681805.2014.932842(554-558)
Fujita K, Kanayama Y, Kim J, Nakajima K (2019) A preliminary study on a voided volume measuring method using noncontact temperature sensors under the toilet seat. Adv Biomed Eng 8:1–6. https://doi.org/10.14326/abe.8.1
Chan C, Yip SK, Wu IP, Li ML, Chan NH (2011) Evaluation of the clinical value of a simple flowmeter in the management of male lower urinary tract symptoms. BJUI 109(11):1690–1696. https://doi.org/10.1111/j.1464-410X.2011.10581.x
Krhut J, Gartner M et al (2015) Comparison between uroflowmetry and sonouroflowmetry in recording of urinary flow in healthy men. Int J Urol 22(8):761–765. https://doi.org/10.1111/iju.12796
Acknowledgements
The authors thank Victoria Cooley, MS and Paul Christos, Dr.PH, MS.
Funding
There was no funding provided for this manuscript.
Author information
Authors and Affiliations
Contributions
MK: protocol/project development, data collection or management, data analysis, manuscript writing/editing. DT: protocol/project development, data collection or management, data analysis, manuscript writing/editing. NZ: protocol/project development, data collection or management, data analysis, manuscript writing/editing. DD: data collection or management, data analysis, manuscript writing/editing. RD: protocol/project development, data collection or management, manuscript writing/editing. BC: protocol/project development, data collection or management, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
MK, DT, NZ, DD, and RD have nothing to disclose. BC is an investigator for Ipsen, Astellas, and Medi-tate. BC is also a key opinion leader for Boston Scientific. BC is a speaker for Allergan (instructor) and Mist Pharmaceuticals (discontinued).
Research involving Human Participants and/or Animals
Human participants were involved in this review. Animals were not included in this review.
Informed consent
Informed consent was collected.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kini, M., Thomas, D., Zaidi, N. et al. Can men with lower urinary tract symptoms (LUTs) predict voided volumes?. World J Urol 38, 1261–1266 (2020). https://doi.org/10.1007/s00345-019-02907-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02907-3