Abstract
Objective
To compare the rate of hospital-based outcomes including costs, 30-day readmission, mortality, and length of stay in patients who underwent major urologic oncologic procedures in academic and community hospitals.
Methods
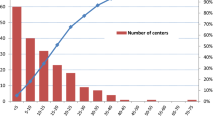
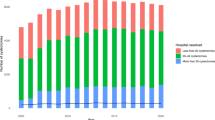
We retrospectively reviewed the Vizient Database (Irving, Texas) from September 2014 to December 2017. Vizient includes ~ 97% of academic hospitals (AH) and more than 60 community hospitals (CH). Patients aged ≥ 18 with urologic malignancies who underwent surgical treatment were included. Chi square and Student t tests were used to compare categorical and continuous variables, respectively.
Results
We identified a total of 37,628 cases. There were 33,290 (88%) procedures performed in AH and 4330 (12%) in CH. These included prostatectomy (18,540), radical nephrectomy (rNx) 8059, partial nephrectomy (pNx) (5287), radical cystectomy (4421), radical nephroureterectomy (rNu) (1006), and partial cystectomy (321). There were no significant differences in 30-day readmission rates or mortality for any procedure between academic and community hospitals (Table 1), p > 0.05 for all. Length of stay was significantly lower for radical cystectomy and prostatectomy in AH (p < 0.01 for both) and lower for rNx in CH (p = 0.03). The mean direct cost for index admission was significantly higher in AH for rNx, pNx, rNu, and prostatectomy. Case mix index was similar between the community and academic hospitals.
Conclusion
Despite academic and community hospitals having similar case complexity, direct costs were lower in community hospitals without an associated increase in readmission rates or deaths. Length of stay was shorter for cystectomy in academic centers.
Similar content being viewed by others
References
Chow W-H, Dong LM, Devesa SS (2010) Epidemiology and risk factors for kidney cancer. Nat Rev Urol 7:245–257. https://doi.org/10.1038/nrurol.2010.46
Hock LM, Lynch J, Balaji KC (2002) Increasing incidence of all stages of kidney cancer in the last 2 decades in the United States: an analysis of surveillance, epidemiology and end results program data. J Urol 167:57–60. https://doi.org/10.1016/S0022-5347(05)65382-7
Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O et al (2012) International variation in prostate cancer incidence and mortality rates. Eur Urol 61:1079–1092. https://doi.org/10.1016/j.eururo.2012.02.054
Antoni S, Ferlay J, Soerjomataram I, Znaor A, Jemal A, Bray F (2017) Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol 71:96–108. https://doi.org/10.1016/j.eururo.2016.06.010
Tsui K-H, Shvarts O, Smith RB, Figlin R, de Kernion JB, Belldegrun A (2000) Renal cell carcinoma: prognostic significance of incidentally detected tumors. J Urol 163:426–430. https://doi.org/10.1016/s0022-5347(05)67892-5
Jayson M, Sanders H (1998) Increased incidence of serendipitously discovered renal cell carcinoma. Urology 51:203–205. https://doi.org/10.1016/S0090-4295(97)00506-2
Victoor A, Delnoij DM, Friele RD, Rademakers JJ (2012) Determinants of patient choice of healthcare providers: a scoping review. BMC Health Serv Res 12:272. https://doi.org/10.1186/1472-6963-12-272
Victoor A, Delnoij D, Friele R, Rademakers J (2016) Why patients may not exercise their choice when referred for hospital care. An exploratory study based on interviews with patients. Heal Expect 19:667–678. https://doi.org/10.1111/hex.12224
Gao Y, Pugely A, Karam M, Phisitkul P, Mendoza S, Johnston RC (2013) Is hospital teaching status a key factor in hospital charge for children with hip fractures?: preliminary findings from KID database. Iowa Orthop J 33:130–135
Chen Q, Bagante F, Merath K, Idrees J, Beal EW, Cloyd J et al (2018) Hospital teaching status and medicare expenditures for hepato-pancreato-biliary surgery. World J Surg 42:2969–2979. https://doi.org/10.1007/s00268-018-4566-1
Pradarelli JC, Scally CP, Nathan H, Thumma JR, Dimick JB (2017) Hospital teaching status and medicare expenditures for complex surgery. Ann Surg 265:502–513. https://doi.org/10.1097/SLA.0000000000001706
Perfetti DC, Sodhi N, Khlopas A, Sultan AA, Lamaj S, Boylan MR et al (2017) Is orthopaedic department teaching status associated with adverse outcomes of primary total knee arthroplasty? Surg Technol Int 31:379–383
Lai PMR, Lin N, Du R (2014) Effect of teaching hospital status on outcome of aneurysm treatment. World Neurosurg 82:380–385. https://doi.org/10.1016/j.wneu.2013.07.015
Sandhu A, Moscucci M, Dixon S, Wohns DH, Share D, LaLonde T et al (2013) Differences in the outcome of patients undergoing percutaneous coronary interventions at teaching versus non-teaching hospitals. Am Heart J 166:401–408. https://doi.org/10.1016/j.ahj.2013.06.018
Jalisi S, Bearelly S, Abdillahi A, Truong MT (2013) Outcomes in head and neck oncologic surgery at academic medical centers in the United States. Laryngoscope 123:689–698. https://doi.org/10.1002/lary.23835
Rinaldo L, Brinjikji W, Cloft H, DeMartino RR, Lanzino G (2017) Investigation into drivers of cost of stenting for carotid stenosis. J Vasc Surg 66:786–793. https://doi.org/10.1016/j.jvs.2017.03.433
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617
Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29:434–440. https://doi.org/10.1016/j.clnu.2010.01.004
Cerantola Y, Valerio M, Persson B, Jichlinski P, Ljungqvist O, Hubner M et al (2013) Guidelines for perioperative care after radical cystectomy for bladder cancer: Enhanced Recovery After Surgery (ERAS((R))) society recommendations. Clin Nutr 32:879–887. https://doi.org/10.1016/j.clnu.2013.09.014
Pang KH, Groves R, Venugopal S, Noon AP, Catto JWF (2017) Prospective implementation of enhanced recovery after surgery protocols to radical cystectomy. Eur Urol. https://doi.org/10.1016/j.eururo.2017.07.031
Frees SK, Aning J, Black P, Struss W, Bell R, Chavez-Munoz C et al (2018) A prospective randomized pilot study evaluating an ERAS protocol versus a standard protocol for patients treated with radical cystectomy and urinary diversion for bladder cancer. World J Urol 36:215–220. https://doi.org/10.1007/s00345-017-2109-2
Semerjian A, Milbar N, Kates M, Gorin MA, Patel HD, Chalfin HJ et al (2018) Hospital charges and length of stay following radical cystectomy in the enhanced recovery after surgery era. Urology 111:86–91. https://doi.org/10.1016/j.urology.2017.09.010
Tang K, Xia D, Li H, Guan W, Guo X, Hu Z et al (2014) Robotic vs. open radical cystectomy in bladder cancer: a systematic review and meta-analysis. Eur J Surg Oncol 40:1399–1411. https://doi.org/10.1016/j.ejso.2014.03.008
Gandaglia G, Karl A, Novara G, de Groote R, Buchner A, D’Hondt F et al (2016) Perioperative and oncologic outcomes of robot-assisted vs. open radical cystectomy in bladder cancer patients: a comparison of two high-volume referral centers. Eur J Surg Oncol 42:1736–1743. https://doi.org/10.1016/j.ejso.2016.02.254
Winters BR, Bremjit PJ, Gore JL, Lin DW, Ellis WJ, Dalkin BL et al (2016) Preliminary comparative effectiveness of robotic versus open radical cystectomy in elderly patients. J Endourol 30:212–217. https://doi.org/10.1089/end.2015.0457
Wallerstedt A, Tyritzis SI, Thorsteinsdottir T, Carlsson S, Stranne J, Gustafsson O et al (2015) Short-term results after robot-assisted laparoscopic radical prostatectomy compared to open radical prostatectomy. Eur Urol 67:660–670. https://doi.org/10.1016/j.eururo.2014.09.036
Ilic D, Evans SM, Allan CA, Jung JH, Murphy D, Frydenberg M (2018) Laparoscopic and robot-assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review. BJU Int 121:845–853. https://doi.org/10.1111/bju.14062
Wenderoth UK, Bachor R, Egghart G, Frohneberg D, Miller K, Hautmann RE (1990) The ileal neobladder: experience and results of more than 100 consecutive cases. J Urol 143:492–497
Figueroa AJ, Stein JP, Dickinson M, Skinner EC, Thangathurai D, Mikhail MS et al (1998) Radical cystectomy for elderly patients with bladder carcinoma: an updated experience with 404 patients. Cancer 83:141–147
Chang SS, Cookson MS, Baumgartner RG, Wells N, Smith JA Jr (2002) Analysis of early complications after radical cystectomy: results of a collaborative care pathway. J Urol 167:2012–2016
Stimson CJ, Chang SS, Barocas DA, Humphrey JE, Patel SG, Clark PE et al (2010) Early and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary series. J Urol 184:1296–1300. https://doi.org/10.1016/j.juro.2010.06.007
Altobelli E, Buscarini M, Gill HS, Skinner EC (2017) Readmission rate and causes at 90-day after radical cystectomy in patients on early recovery after surgery protocol. Bladder Cancer 3:51–56. https://doi.org/10.3233/blc-160061
Zainfeld D, Shah A, Daneshmand S (2018) enhanced recovery after surgery pathways: role and outcomes in the management of muscle invasive bladder cancer. Urol Clin North Am 45:229–239. https://doi.org/10.1016/j.ucl.2017.12.007
Shabsigh A, Korets R, Vora KC, Brooks CM, Cronin AM, Savage C et al (2009) Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol 55:164–174. https://doi.org/10.1016/j.eururo.2008.07.031
Yuh BE, Nazmy M, Ruel NH, Jankowski JT, Menchaca AR, Torrey RR et al (2012) Standardized analysis of frequency and severity of complications after robot-assisted radical cystectomy. Eur Urol 62:806–813. https://doi.org/10.1016/j.eururo.2012.06.007
Chappidi MR, Kates M, Stimson CJ, Bivalacqua TJ, Pierorazio PM (2017) Quantifying nonindex hospital readmissions and care fragmentation after major urological oncology surgeries in a nationally representative sample. J Urol 197:235–240. https://doi.org/10.1016/j.juro.2016.07.078
Leow JJ, Reese SW, Jiang W, Lipsitz SR, Bellmunt J, Trinh QD et al (2014) Propensity-matched comparison of morbidity and costs of open and robot-assisted radical cystectomies: a contemporary population-based analysis in the United States. Eur Urol 66:569–576. https://doi.org/10.1016/j.eururo.2014.01.029
Tinay I, Gelpi-Hammerschmidt F, Leow JJ, Allard CB, Rodriguez D, Wang Y et al (2016) Trends in utilisation, perioperative outcomes, and costs of nephroureterectomies in the management of upper tract urothelial carcinoma: a 10-year population-based analysis. BJU Int 117:954–960. https://doi.org/10.1111/bju.13375
Jeong IG, Khandwala YS, Kim JH, Han DH, Li S, Wang Y et al (2017) Association of robotic-assisted vs laparoscopic radical nephrectomy with perioperative outcomes and health care costs, 2003 to 2015. JAMA 318:1561–1568. https://doi.org/10.1001/jama.2017.14586
Mossanen M, Krasnow RE, Lipsitz SR, Preston MA, Kibel AS, Ha A et al (2018) Associations of specific postoperative complications with costs after radical cystectomy. BJU Int 121:428–436. https://doi.org/10.1111/bju.14064
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Syed, J.S., Abello, A., Nguyen, J. et al. Outcomes for urologic oncology procedures: are there differences between academic and community hospitals?. World J Urol 38, 1187–1193 (2020). https://doi.org/10.1007/s00345-019-02902-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02902-8