Abstract
Purpose
To assess the available literature evidence that discusses the effect of surgical experience on patient outcomes in robotic setting. This information is used to help understand how we can develop a learning process that allows surgeons to maximally accommodate patient safety.
Methods
A literature search of the MEDLINE/PubMed and Scopus database was performed. Original and review articles published in the English language were included after an interactive peer-review process of the panel.
Results
Robotic surgical procedures require high level of experience to guarantee patient safety. This means that, for some procedures, the learning process might be longer than originally expected. In this context, structured training programs that assist surgeons to improve outcomes during their learning processes were extensively discussed. We identified few structured robotic curricula and demonstrated that for some procedures, curriculum trained surgeons can achieve outcomes rates during their initial learning phases that are at least comparable to those of experienced surgeons from high-volume centres. Finally, the importance of non-technical skills on patient safety and of their inclusion in robotic training programs was also assessed.
Conclusion
To guarantee safe robotic surgery and to optimize patient outcomes during the learning process, standardized and validated training programs are instrumental. To date, only few structured validated curricula exist for standardized training and further efforts are needed in this direction.
Similar content being viewed by others
References
Makary MA, Daniel M (2016) Medical error-the third leading cause of death in the US. BMJ 353:1–5. https://doi.org/10.1136/bmj.i2139
Kohn LT, Corrigan JM, Donaldson MS (eds) (2000) To err is human: building a safer health system. Institute of Medicine (US) Committee on Quality of Health Care in America. National Academies Press (US), Washington, DC
World Health Organization (2009) WHO guidelines for safe surgery: safe surgery saves lives
Mazzone E, Mistretta FA, Knipper S, Tian Z, Larcher A, Widmer H et al (2019) Contemporary North-American assessment of robot-assisted surgery rates and total hospital charges for major surgical uro-oncological procedures. J Endourol 33(6):438–447
Sridhar AN, Briggs TP, Kelly JD, Nathan S (2017) Training in robotic surgery—an overview. Curr Urol Rep 18(8):58
Schreuder HWR, Wolswijk R, Zweemer RP, Schijven MP, Verheijen RHM (2012) Training and learning robotic surgery, time for a more structured approach: a systematic review. BJOG 119(2):137–149
Brook NR, Dell’Oglio P, Barod R, Collins J, Mottrie A (2018) Comprehensive training in robotic surgery. Curr Opin Urol 29(1):1–9
Ahmed K, Khan R, Mottrie A, Lovegrove C, Abaza R, Ahlawat R et al (2015) Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int 116(1):93–101
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST et al (2012) Developing a comprehensive, proficiency-based training program for robotic surgery. Surgery 152(3):477–488
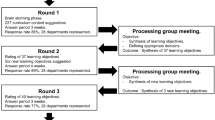
Collins JW, Levy J, Stefanidis D, Gallagher A, Coleman M, Cecil T et al (2019) Utilising the delphi process to develop a proficiency-based progression train-the-trainer course for robotic surgery training. Eur Urol. https://doi.org/10.1016/j.eururo.2018.12.044
Fiorini P, Grespan L. SAFROS project: patient safety in robotic surgery. Seventh framework programme research project (FP7-ICT-2009.5.2). University of Verona
Vickers A, Savage C, Bianco F, Mulhall J, Sandhu J, Guillonneau B et al (2011) Cancer control and functional outcomes after radical prostatectomy as markers of surgical quality: analysis of heterogeneity between surgeons at a single cancer center. Eur Urol 59(3):317–322. https://doi.org/10.1016/j.eururo.2010.10.045
Thompson JE, Egger S, Böhm M, Siriwardana AR, Haynes A-M, Matthews J et al (2017) Superior biochemical recurrence and long-term quality-of-life outcomes are achievable with robotic radical prostatectomy after a long learning curve - updated analysis of a prospective single-surgeon cohort of 2206 consecutive cases. Eur Urol 73(5):664–671. https://doi.org/10.1016/j.eururo.2017.11.035
Collins JW, Tyritzis S, Nyberg T, Schumacher MC, Laurin O, Adding C et al (2014) Robot-assisted radical cystectomy (RARC) with intracorporeal neobladder—what is the effect of the learning curve on outcomes? BJU Int 113(1):100–107
Larcher A, Muttin F, Peyronnet B, De Naeyer G, Khene ZE, Dell’Oglio P et al (2018) The learning curve for robot-assisted partial nephrectomy: impact of surgical experience on perioperative outcomes. Eur Urol. https://doi.org/10.1016/j.eururo.2018.08.042
Vickers AJ, Bianco FJ, Serio AM, Eastham JA, Schrag D, Klein EA et al (2007) The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst 99(15):1171–1177
Cook JA, Ramsay CR, Fayers P (2007) Using the literature to quantify the learning curve: a case study. Int J Technol Assess Health Care 23(2):255–260
Subramonian K, Muir G (2004) The “learning curve” in surgery: what is it, how do we measure it and can we influence it? BJU Int 93(9):1173–1174
Abboudi H, Khan MS, Guru KA, Froghi S, De Win G, Van Poppel H et al (2014) Learning curves for urological procedures: a systematic review. BJU Int 114(4):617–629
Di Pierro GB, Wirth JG, Ferrari M, Danuser H, Mattei A (2014) Impact of a single-surgeon learning curve on complications, positioning injuries, and renal function in patients undergoing robot-assisted radical prostatectomy and extended pelvic lymph node dissection. Urology 84(5):1106–1111
Monnerat Lott F, Siqueira D, Argolo H, Lindberg Nobrega B, Campos FS, Favorito LA (2018) Analysis of the learning curve of surgeons without previous experience in laparoscopy to perform robot-assisted radical prostatectomy. Adv Urol 2018:9073807
Ou Y-C, Yang C-R, Wang J, Yang C-K, Cheng C-L, Patel VR et al (2011) The learning curve for reducing complications of robotic-assisted laparoscopic radical prostatectomy by a single surgeon. BJU Int 108(3):420–425. https://doi.org/10.1111/j.1464-410X.2010.09847.x
O’Malley PJ, Van Appledorn S, Bouchier-Hayes DM, Crowe H, Costello AJ (2006) Robotic radical prostatectomy in Australia: initial experience. World J Urol 24(2):165–170
Sharma NL, Papadopoulos A, Lee D, Mcloughlin J, Vowler SL, Baumert H et al (2010) First 500 cases of robotic-assisted laparoscopic radical prostatectomy from a single UK centre: learning curves of two surgeons. BJU Int 108(5):739–747
Giberti C, Schenone M, Gallo F, Cortese P, Ninotta G (2011) 343 Robot assisted laparoscopic prostatectomy (ralp): the “real” learning curve. Eur Urol Suppl 10(2):125. http://www.sciencedirect.com/science/article/pii/S1569905611603394
Gumus E, Boylu U, Turan T, Onol FF (2011) The learning curve of robot-assisted radical prostatectomy. J Endourol 25(10):1633–1637. https://doi.org/10.1089/end.2011.0071
Hayn MH, Hussain A, Mansour AM, Andrews PE, Carpentier P, Castle E et al (2010) The learning curve of robot-assisted radical cystectomy: results from the international robotic cystectomy consortium. Eur Urol 58(2):197–202. https://doi.org/10.1016/j.eururo.2010.04.024
Sivaraman A, Sanchez-Salas R, Prapotnich D, Yu K, Olivier F, Secin FP et al (2017) Learning curve of minimally invasive radical prostatectomy: comprehensive evaluation and cumulative summation analysis of oncological outcomes. Urol Oncol 35(4):149.e1–149.e6
Ou YC, Yang CR, Wang J, Yang CK, Cheng CL, Patel VR et al (2011) The learning curve for reducing complications of robotic-assisted laparoscopic radical prostatectomy by a single surgeon. BJU Int 108(3):420–425
Vickers AJ, Maschino A, Savage CJ, Cronin AM (2012) Assessing the learning curve for prostate cancer surgery BT. In: Patel VR (ed) Robotic urologic surgery. Springer, London, pp 49–60. https://doi.org/10.1007/978-1-84882-800-1_6
Vickers AJ, Savage CJ, Hruza M, Tuerk I, Koenig P, Martínez-Piñeiro L et al (2009) The surgical learning curve for laparoscopic radical prostatectomy: a retrospective cohort study. Lancet Oncol 10(5):475–480
Bravi CA, Tin A, Vertosick E, Mazzone E, Martini A, Dell’Oglio P et al (2019) The impact of experience on the risk of surgical margins and biochemical recurrence after robot-assisted radical prostatectomy: a learning-curve study. J Urol 202(1):108–113
Thompson JE, Egger S, Böhm M, Haynes A-M, Matthews J, Rasiah K et al (2014) Superior quality of life and improved surgical margins are achievable with robotic radical prostatectomy after a long learning curve: a prospective single-surgeon study of 1552 consecutive cases. Eur Urol 65(3):521–531. https://doi.org/10.1016/j.eururo.2013.10.030
Leroy TJ, Thiel DD, Duchene DA, Parker AS, Igel TC, Wehle MJ et al (2010) Safety and peri-operative outcomes during learning curve of robot-assisted laparoscopic prostatectomy: a multi-institutional study of fellowship-trained robotic surgeons versus experienced open radical prostatectomy surgeons incorporating robot-assisted L. J Endourol 24(10):1665–1669
Mottrie A, De Naeyer G, Schatteman P, Carpentier P, Sangalli M, Ficarra V (2010) Impact of the learning curve on perioperative outcomes in patients who underwent robotic partial nephrectomy for parenchymal renal tumours. Eur Urol 58(1):127–132
Dias BH, Ali MS, Dubey S, Krishnaswamy SA, Rao AR, Dubey D (2018) Impact of learning curve on the perioperative outcomes following robot-assisted partial nephrectomy for renal tumors. Indian J Urol 34(1):62–67
Xie Y, Ma X, Gu L, Li H, Lv X, Gao Y et al (2016) Associating the learning curve and tumor anatomical complexity with the margins, ischemia, and complications rate after robot-assisted partial nephrectomy. Int J Surg 36(Pt A):219–224
Hanzly M, Frederick A, Creighton T, Atwood K, Mehedint D, Kauffman EC et al (2015) Learning curves for robot-assisted and laparoscopic partial nephrectomy. J Endourol 29(3):297–303
Larcher A, Muttin F, Peyronnet B, De Naeyer G, Khene Z, Dell P et al (2018) The learning curve for robot-assisted partial nephrectomy: impact of surgical experience on perioperative outcomes. Eur Urol 75(2):253–256
Paulucci DJ, Abaza R, Eun DD, Hemal AK, Badani KK (2017) Robot-assisted partial nephrectomy: continued refinement of outcomes beyond the initial learning curve. BJU Int 119(5):748–754
Richards KA, Kader K, Pettus JA, Smith JJ, Hemal AK (2011) Does initial learning curve compromise outcomes for robot-assisted radical cystectomy? A critical evaluation of the first 60 cases while establishing a robotics program. J Endourol 25(9):1553–1558
Mottrie A, Novara G (2014) Is surgery a never-ending learning process? BJU Int 114(4):472–473
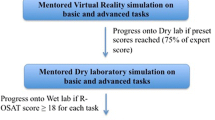
Volpe A, Ahmed K, Dasgupta P, Ficarra V, Novara G, Van Der Poel H et al (2015) Pilot validation study of the european association of urology robotic training curriculum. Eur Urol 68(2):292–299. https://doi.org/10.1016/j.eururo.2014.10.025
Mottrie A, Novara G, van der Poel H, Dasgupta P, Montorsi F, Gandaglia G (2016) The european association of urology robotic training curriculum: an update. Eur Urol Focus 2(1):105–108
Jayakumar N, Brunckhorst O, Dasgupta P, Khan MS, Ahmed K (2015) e-Learning in surgical education: a systematic review. J Surg Educ 72(6):1145–1157
https://www.intuitive.com/. Accessed 2015
Kumar A, Smith R, Patel VR (2015) Current status of robotic simulators in acquisition of robotic surgical skills. Curr Opin Urol 25(2):168–174
Moglia A, Ferrari V, Morelli L, Ferrari M, Mosca F, Cuschieri A (2016) A systematic review of virtual reality simulators for robot-assisted surgery. Eur Urol 69(6):1065–1080
Larcher A, Turri F, Bianchi L, Dell’Oglio P, Collins J, Capitanio U et al (2019) Virtual reality validation of the erus simulation-based training programmes: results from a high-volume training centre for robot-assisted surgery. Eur Urol. https://doi.org/10.1016/j.eururo.2019.02.008
Gallagher A (2012) Metric-based simulation training to proficiency in medical education: what it is and how to do it. Ulster Med J 81(3):107–113
Gallagher A (2018) Proficiency-based progression simulation training for more than an interesting educational experience. J Musculoskelet Surg Res 2(4):139
Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ (2012) Global evaluative assessment of robotic skills: validation of a clinical assessment tool to measure robotic surgical skills. J Urol 187(1):247–252
Mazzone E, Dell’Oglio P, Mottrie A (2019) Outcome report of the first ERUS robotic urology curriculum-trained surgeon in Turkey: the importance of structured and validated training programs for global outcome improvement. Turk J Urol. https://doi.org/10.5152/tud.2019.19019
Schiavina R, Borghesi M, Dababneh H, Rossi MS, Pultrone CV, Vagnoni V et al (2018) The impact of a structured intensive modular training in the learning curve of robot assisted radical prostatectomy. Arch Ital di Urol Androl 90(1):1–7
Bedir F, Kocaturk H, Canda AE, Atmaca AF, Demirdogen SO, Keske M et al (2019) Robotic radical prostatectomy in 93 cases: outcomes of the first ERUS robotic urology curriculum trained surgeon in Turkey. Turk J Urol 45:183
Larcher A, De Naeyer G, Turri F, Dell’Oglio P, Capitanio U, Collins J et al (2019) The ERUS curriculum for robot-assisted partial nephrectomy: structure definition and pilot clinical validation. Eur Urol 75:1023–1031
Dell’Oglio P, Turri F, Larcher A, D’Hondt F, Sanchez-Salas R, Bochner B et al (2019) Definition of a structured training curriculum for robot-assisted radical cystectomy: a delphi-consensus study led by the ERUS educational board. Eur Urol Suppl 18(1):e1116–e1119. https://doi.org/10.1016/S1569-9056(19)30808-5
BAUS. Robotic surgery curriculum—guidelines for training. https://www.baus.org.uk/professionals/baus_business/publications/83/robotic_surgery_curriculum/
Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R et al (2013) Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology 81(4):767–774
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST et al (2012) Proficiency-based training for robotic surgery: construct validity, workload, and expert levels for nine inanimate exercises. Surg Endosc 26(6):1516–1521. https://doi.org/10.1007/s00464-011-2102-6
Foell K, Finelli A, Yasufuku K, Bernardini MQ, Waddell TK, Pace KT et al (2013) Robotic surgery basic skills training: evaluation of a pilot multidisciplinary simulation-based curriculum. Can Urol Assoc J 7(11–12):430–434. https://www.ncbi.nlm.nih.gov/pubmed/24381662
Fellowship of international college of robotic surgeons. http://icrsonline.org/fellowship.html
Attalla K, Raza S, Rehman S, Din R, Stegemann A, Perusich E et al (2013) Effectiveness of a dedicated robot-assisted surgery training program. Canadian J Urol 20:7084–7090
Macgregor JM, Kim RS, Gallagher JT, Soliman MK, Ferrara A, Baldwin K et al (2012) Fundamentals of robotic surgery. Soc Am Gastrointest Endosc Surg Annu Meet. Poster P151
Lyons C, Goldfarb D, Jones SL, Badhiwala N, Miles B, Link R et al (2013) Which skills really matter? proving face, content, and construct validity for a commercial robotic simulator. Surg Endosc 27(6):2020–2030
Smith R, Patel V, Satava R (2014) Fundamentals of robotic surgery: a course of basic robotic surgery skills based upon a 14-society consensus template of outcomes measures and curriculum development. Int J Med Robot 10(3):379–384
Cecilio-Fernandes D, Cnossen F, Jaarsma DADC, Tio RA (2018) Avoiding surgical skill decay: a systematic review on the spacing of training sessions. J Surg Educ 75(2):471–480
Satava RM, Stefanidis D, Levy JS, Smith R, Martin JR, Monfared S et al (2019) Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum: a single-blinded, multispecialty, multi-institutional randomized control trial. Ann Surg. https://doi.org/10.1097/SLA.0000000000003220
Goldenberg MG, Goldenberg L, Grantcharov TP (2017) Surgeon performance predicts early continence after robot-assisted radical prostatectomy. J Endourol 31(9):858–863
Angelo RL, Ryu RKN, Pedowitz RA, Beach W, Burns J, Dodds J et al (2015) A proficiency-based progression training curriculum coupled with a model simulator results in the acquisition of a superior arthroscopic Bankart skill set. Arthroscopy 31(10):1854–1871. https://doi.org/10.1016/j.arthro.2015.07.001
Cates CU, Lönn L, Gallagher AG (2016) Prospective, randomised and blinded comparison of proficiency-based progression full-physics virtual reality simulator training versus invasive vascular experience for learning carotid artery angiography by very experienced operators. BMJ Simul Technol Enhanc Learn 2(1):1–5. http://stel.bmj.com/content/2/1/1.abstract
Gallagher AG, Seymour NE, Jordan-Black J-A, Bunting BP, McGlade K, Satava RM (2013) Prospective, randomized assessment of transfer of training (ToT) and transfer effectiveness ratio (TER) of virtual reality simulation training for laparoscopic skill acquisition. Ann Surg 257(6):1025–1031
Van Sickle KR, Ritter EM, Baghai M, Goldenberg AE, Huang I-P, Gallagher AG et al (2008) Prospective, randomized, double-blind trial of curriculum-based training for intracorporeal suturing and knot tying. J Am Coll Surg 207(4):560–568
De Win G, Van Bruwaene S, Kulkarni J, Van Calster B, Aggarwal R, Allen C et al (2016) An evidence-based laparoscopic simulation curriculum shortens the clinical learning curve and reduces surgical adverse events. Adv Med Educ Pract 7:357–370
Hung AJ, Chen J, Ghodoussipour S, Oh PJ, Liu Z, Nguyen J et al (2019) A deep-learning model using automated performance metrics and clinical features to predict urinary continence recovery after robot-assisted radical prostatectomy. BJU Int. https://doi.org/10.1111/bju.14735
Collins JW, Dell’Oglio P, Hung AJ, Brook NR (2018) The Importance of Technical and Non-technical Skills in Robotic Surgery Training. Eur Urol Focus 4(5):674–676. https://doi.org/10.1016/j.euf.2018.08.018
van der Poel H, Brinkman W, van Cleynenbreugel B, Kallidonis P, Stolzenburg J-U, Liatsikos E et al (2016) Training in minimally invasive surgery in urology: European Association of Urology/International Consultation of Urological Diseases consultation. BJU Int 117(3):515–530
Yule J, Hill K, Yule S (2018) Development and evaluation of a patient-centred measurement tool for surgeons’ non-technical skills. BJS 105(7):876–884
Undre S, Healey AN, Darzi A, Vincent CA (2006) Observational assessment of surgical teamwork: a feasibility study. World J Surg 30(10):1774–1783
Raison N, Wood T, Brunckhorst O, Abe T, Ross T, Challacombe B et al (2017) Development and validation of a tool for non-technical skills evaluation in robotic surgery—the ICARS system. Surg Endosc 31(12):5403–5410. https://doi.org/10.1007/s00464-017-5622-x
Leonard M, Graham S, Bonacum D (2004) The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 13(Suppl 1):i85–i90. https://www.ncbi.nlm.nih.gov/pubmed/15465961
Nance JJ (2008) Why hospitals should fly: the ultimate flight plan to patient safety and quality care. Second River Healthcare Press, Bozeman, Montana
Brewin J, Ahmed K, Challacombe B (2014) An update and review of simulation in urological training. Int J Surg 12(2):103–108
Brunckhorst O, Volpe A, Van Der Poel H, Mottrie A, Ahmed K, Catto J (2016) Training, simulation, the learning curve, and how to reduce complications in urology. Eur Urol Focus 2(1):10–18
Chen J, Cheng N, Cacciamani G, Oh P, Lin-Brande M, Remulla D et al (2019) Objective assessment of robotic surgical technical skill: a systematic review. J Urol 201(3):461–469
Mazzocco K, Petitti DB, Fong KT, Bonacum D, Brookey J, Graham S et al (2009) Surgical team behaviors and patient outcomes. Am J Surg 197(5):678–685
Collins JW, Dell’Oglio P, Hung AJ, Brook NR (2018) The importance of technical and non-technical skills in robotic surgery training. Eur Urol Focus 4(5):674–676
Flin R, Yule S, Paterson-Brown S, Maran N, Rowley D, Youngson G (2007) Teaching surgeons about non-technical skills. Surgeon 5(2):86–89
Dasgupta P, Ahmed K, Jaye P, Khan M (2014) Surgical simulation. Anthem Press, London
Fanning RM, Gaba DM (2007) The role of debriefing in simulation-based learning. Simul Healthc 2(2):115–125
Undre S, Koutantji M, Sevdalis N, Gautama S, Selvapatt N, Williams S et al (2007) Multidisciplinary crisis simulations: the way forward for training surgical teams. World J Surg 31(9):1843–1853
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Palagonia, E., Mazzone, E., De Naeyer, G. et al. The safety of urologic robotic surgery depends on the skills of the surgeon. World J Urol 38, 1373–1383 (2020). https://doi.org/10.1007/s00345-019-02901-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02901-9