Abstract
Purpose
To identify potential risk factors for the development of venous thromboembolic events in testicular cancer patients receiving platinum-based chemotherapy.
Methods
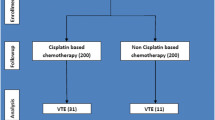
We performed a retrospective analysis including 255 patients with testicular germ cell tumors who received platinum-based chemotherapy from 2003 to 2018 as a multi-center observational cohort study. Patient and tumor characteristics of patients with and without a thromboembolic event were analyzed.
Results
49 (19%) patients experienced a venous thromboembolic event, with the majority representing pulmonary embolism and deep venous thrombosis (47%). There were no significant differences regarding the development of a venous thromboembolic event between first- and second-line regimes. Multivariate analysis showed an increased risk for a venous thromboembolic event in patients with clinical stage ≥ IIC disease (OR 2.259 [95% CI 1.105–4.618], p = 0.026), elevated serum LDH (OR 2.162 [95% CI 1.018–4.593], p = 0.045), febrile neutropenia (OR 2.973 [95% CI 1.363–6.487], p = 0.006) and central venous access (OR 3.465 [95% CI 1.068–11.243], p = 0.039). Patients suffering from a venous thromboembolic event revealed a significantly reduced overall survival (p = 0.033) during a median follow-up of 8 months [IQR 2–18].
Conclusions
19% of all patients treated by platinum-based chemotherapy due to testicular cancer suffered from a venous thromboembolic event, associated with reduced overall survival. As a result, monitoring of cancer patients at risk as well as the improvement of patients’ awareness of a thromboembolic event should thus be the main goal of their treating physicians.
Similar content being viewed by others
Introduction
Testicular germ cell tumors (GCT) represent the most common solid neoplasms in young men with the highest incidence between the second and fourth decade [1]. Due to a risk-adapted interdisciplinary treatment approach including effective platinum-based chemotherapy, GCT shows excellent cure rates even in advanced stages [1]. However, chemotherapy’s substantial efficacy is associated with treatment-related toxicities like thromboembolic events (TEE) [1]. The risk of a TEE is known to be sixfold higher in cancer patients compared to their non-cancer counterparts and the second leading cause of death in cancer patients [2]. In addition, patients suffering from GCTs have a higher mortality from cardiovascular disease compared to the general population [1, 3, 4]. Despite the high number of venous or arterial thrombosis in patients receiving platinum-based chemotherapy for testicular GCT [1, 5], only few studies exist analyzing potential risk factors for TEE in these patients [3, 5,6,7,8,9]. A prior study identified elevated serum lactate dehydrogenase (LDH) and the presence of lymph node metastases to be predictors of TEE [5]. Furthermore, we have previously found a high tumor volume to be associated with an increased risk of a TEE during chemotherapy, which was also seen in another study [6, 10].
The aim of the present study was to assess the clinical and patient characteristics in patients receiving platinum-based chemotherapy including the incidence and localization of TEE. Another objective was to validate known predictors of venous thrombosis and identify potential new risk factors for the development of venous TEE.
Materials and methods
Study population
The testis cancer databases of the University Hospitals of Cologne and Aachen were retrospectively analyzed as a multi-center observational cohort study. 255 patients diagnosed with a malignant GCT of the testis who received a platinum-based chemotherapy between January 2003 and March 2018 have been included in the study, irrespective of tumor stage. Patients who underwent chemotherapy due to another tumor entity as well as patients with a previous history of thrombosis or a known coagulopathy were excluded from the study. The study complies with the Declaration of Helsinki and local ethics committee approval was obtained (17–175). Informed consent was obtained from all individual participants included in the study.
Chemotherapy
All patients received a platinum-based chemotherapy with regimes being administered according to the EAU guidelines [1]. For all regimes, antiemetic prophylaxis consisted of dexamethasone 1–2 × 8 mg on day 1–5 and aprepitant 125 mg on day 1 as well as 80 mg on day 2–5. 2 mg granisetron was added in the PEI (Cisplatin, Etopside, Ifosfamide) and TIP (Cisplatin, Ifosfamide, Paclitaxel) regime on day 1–5. For regimes with high hematotoxic potential granulocyte stimulating factor was given on day 6.
Thromboembolic events (TEE)
A TEE was defined as a venous or arterial thrombosis as well as embolism that occurred between the start of chemotherapy and 6 months after the last chemotherapy cycle and was related to the corresponding first- or second-line treatment, respectively [11]. A suspected TEE was verified by the measurement of D-Dimer, as well as radiologically via a venous doppler ultrasonography, CT scan and/or lung ventilation-perfusion scintigraphy [11] (Table 1). The treatment of a TEE consisted of a therapeutic anticoagulation with low-molecular weight heparin, phenprocoumon or rivaroxaban for at least 6 months according to the available guidelines [11, 12]. Arterial and venous TEE were analyzed separately. The three patients suffering from an arterial TEE were not included in the main analyses, but the percentage and localization of arterial TEE are displayed in Table 5.
Statistical analysis
Continuous variables were summarized as median (25th–75th‰) and categorical variables as count (n, %). Differences in distribution of any two continuous variables were evaluated by the Mann–Whitney U test and statistical association of any two categorical variables by Pearson’s Chi squared test. We used logistic regression for the univariable and multivariable analysis of venous TEE. For multivariable modelling, missing values were multiple imputed five times (fully conditional specification with ten iterations). The corresponding regression coefficients were pooled. The final (multiple) regression model was obtained by backward stepwise elimination of variables with a p value > 0.05; thus, the risk of overfitting needs to be considered in interpretation [13]. Odds ratios (OR) and the corresponding 95% confidence intervals were calculated. The Kaplan–Meier method was used to estimate the overall survival distribution. All reported p values are two-sided; p values < 0.05 were considered statistically significant. Statistical calculations were done with the software SPSS Statistics (23, IBM Corp., Armonk, NY, USA).
Results
Patient and tumor characteristics
The analysis of patient characteristics revealed a higher incidence of venous TEE in patients with nonpulmonary visceral metastases (18% vs. 6%, p = 0.019, Table 2). Furthermore, a venous TEE was seen significantly more often in patients with clinical stage ≥ IIC disease (67% vs. 44%, p = 0.004, Table 2) as well as extended retroperitoneal lymph node metastases ≥N2 (86% vs. 63%, p = 0.023, Table 2).
Serum tumor markers at diagnosis
We next analyzed the circulating tumor markers and serum testosterone levels at diagnosis (Table 3). Elevated LDH > 250 U/l at diagnosis was found significantly more often in patients with a venous TEE compared to those without a TEE (72% vs. 52%, p = 0.018, Table 3). In addition, an inadequate tumor marker decline was seen more often in venous TEE compared to non-TEE patients (57% vs. 32%, p = 0.026, Table 3).
Chemotherapy and surgical management
192 (86%) patients underwent a first-line chemotherapy according to the BEP (Bleomycin, etoposide, cisplatin) regime and 31 (14%) patients received the TIP (Cisplatin, Ifosfamide, Paclitaxel) regime as a second-line treatment (Table 4). There were no significant differences in the chemotherapy regimens and dosages between patients with and without a venous TEE (BEP 89% vs. 85%, TIP 11% vs. 15%, p = 0.545, Table 4). Febrile neutropenia occurred more often in patients with a venous TEE compared to patients without a TEE (33% vs. 13%, p = 0.001, Table 4). The majority of patients suffered from febrile neutropenia during the first cycle of chemotherapy. All venous TEE occurred after or at the same time point of febrile neutropenia. Post-chemotherapy retroperitoneal lymph node dissection (PC-RPLND) was performed in 75 (32%) of all patients. Of these, 21 (47%) patients showed a venous TEE (p = 0.019, Table 4). Venous TEE occurred prior to the PC-RPLND in the majority of patients (64%). 93% of all patients received a prophylactic anticoagulation with a low-molecular-weight heparin (LMWH) during the chemotherapy treatment (Table 4). The use of thromboprophylaxis was not a predictor for venous TEE in multivariate analysis (OR 1231 [95%CI 0.326–4.646]; p = 0.759). Furthermore, we could not show any significant difference regarding the occurrence of a venous TEE between in the different anticoagulation regimes and dosages used in our cohort of patients (Supp. Table 1).
Localization and time point of thromboembolic events
52 (20%) patients experienced an arterial or venous TEE during or after chemotherapy (Table 5). A venous thromboembolic event occurred in 49 (94%) patients with a TEE, the majority of these patients had a pulmonary embolism plus deep venous thrombosis [23 patients (47%)] or a deep venous thrombosis alone [8 patients (17%), Table 5]. An arterial TEE occurred in 3 (6%) patients: one patient suffered from an ST-elevation myocardial infarction and two patients had a thrombosis of the popliteal artery (Table 5). Unfortunately, one patient had to undergo an amputation of the effected leg due to persistent ischemia despite timely thrombectomy. Patients who received chemotherapy via a central venous access had significantly higher numbers of venous TEE compared to patients in which chemotherapy was administered via a peripheral venous catheter (15% vs. 5%, p = 0.011, Table 4). The majority of venous TEE occurred during the first cycle of chemotherapy (Table 6).
Relapse and overall survival during follow-up
After a median follow-up of 8 months [IQR 2–18], relapses were detected in 49 (19%) of all patients by follow-up CT scans or rising tumor markers (Table 7). 12 (5%) patients died, 25% due to a TEE, 33% due to sepsis and 42% due to tumor progression (Table 7). Kaplan–Meier estimates revealed that patients with a venous TEE showed a significantly reduced overall survival (p = 0.033; Fig. 1).
Analysis of predictors for thromboembolic events
Finally, the possible predictors of a venous TEE were analyzed using a binary logistic regression model (Table 8). Multivariate analysis revealed an increased risk for venous TEE in patients with clinical stage ≥ IIC disease (OR 2.259 [95% CI 1.105–4.618], p = 0.026; Table 8), elevated serum LDH (OR 2.162 [95% CI 1.018–4.593], p = 0.045; Table 8), febrile neutropenia (OR 3.465 [95% CI 1.068–11.243], p = 0.039; Table 8), and a central venous access (OR 2.973 [95% CI 1.363–6.487], p = 0.006; Table 8).
Discussion
Malignancies and platinum-based chemotherapy in the treatment of testicular GCT are correlated with an increased risk of TEEs [1, 14, 15]. As testis cancer patients are generally young and have excellent cure rates due to the substantial efficacy of chemotherapy, the analysis of potential risk factors for the development of a TEE has become an increasing awareness in the treatment of testicular cancer [1].
Patients treated by second-line chemotherapy in case of progression or relapse after initial treatment with BEP consequently received higher dosages of chemotherapy compared to those treated only in the first-line setting. Although cancer itself as well as chemotherapy in testicular cancer is associated with a higher risk of TEE [1, 2], our study did not reveal any difference neither between first- and second-line chemotherapy with BEP or TIP regimen, respectively, nor in the dosages used. Regarding the development of TEE, second-line chemotherapy can thus be safely administered in the salvage situation, as it does not seem to be associated with an increased risk of venous TEE.
Furthermore, we revealed a reduced overall survival in patients with a venous TEE. The most frequent cause of mortality in our patient cohort suffering from venous TEE was thrombosis and tumor progression. A prior study identified thrombosis accounting for 9% of cancer-related deaths during chemotherapy [16]. Congruently, venous TEE was associated with an increased mortality in prostate cancer patients showing a hazard ratio of 6.89 [17]. Nevertheless, a better understanding of the mechanism responsible for the association between tumor biology and the development of TEE is warranted.
Prior studies have identified several risk factors for the development of TEE in the past decades [3, 5, 6, 8, 18, 19]. Recent studies found an elevated serum LDH to be a significant risk factor [3, 5, 18]. In accordance, 72% of our patients with a venous TEE showed an elevated serum LDH which was an independent risk factor for venous TEE in multivariate analysis. Thus, the level of serum LDH might not only be related to the prognosis of advanced GCTs according to the IGCCCG risk classification, but also predict the occurrence of TEE [20]. In contrast to the other tumor markers, AFP and ß-hCG, LDH can be measured as a surrogate for tissue damage. However, it remains still unclear whether the destroyed cells or LDH itself are potentially associated with procoagulant factors and, therefore, responsible for an increased risk of TEE.
Furthermore, prior studies showed the presence of enlarged lymph nodes to be a risk factor for the development of TEE in platinum-based chemotherapy patients with GCTs [5, 10, 18, 19]. In addition, we have previously demonstrated that a clinical stage ≥ IIC is associated with an increased risk of a venous TEE during chemotherapy [6]. The present study strongly supports these findings as multivariate analysis found clinical stage ≥ IIC to be an independent risk factor for TEE. A possible explanation for a high tumor load correlated with the development of a TEE might be the compression of retroperitoneal and femoral vessels. In line with these findings, we showed that PC-RPLND was associated with the occurrence of venous TEE. As PC-RPLND is performed only in case of persisting residual tumors > 1 cm after chemotherapy [1], these findings corroborate with the fact that a high tumor load, characterised by clinical stage ≥ IIC, was shown to be an independent predictor of a venous TEE.
Moreover, febrile neutropenia was identified as an independent risk factor for venous TEE, which was underlined by a prior study [21]. TEE was recently reported to occur in 7.98% of all hospitalized adult cancer patients with febrile neutropenia including testicular cancer patients with an increasing incidence from 1995 to 2002 [22]. Another study identified multiple neutropenic episodes as a risk factor for TEE recurrence [23]. Although the conditions possibly relevant to the pathogenesis of TEE in patients suffering from febrile neutropenia are not fully understood yet, one reason might be the frequently discussed thrombogenetic potential of hematopoietic growth factors that are commonly administered to patients with febrile neutropenia [22]. The majority of patients suffered from a febrile neutropenia in the first cycle of chemotherapy and all venous TEE occurred after or at the same time in our study. Thus, focused screening for TEE is warranted in patients with a febrile neutropenia.
Although the majority of venous TEE occurred as pulmonary embolism or deep venous thrombosis in our study, venous thrombosis was also seen in the upper extremities. Several studies identified the presence of a central venous access as associated with an increased risk of thrombosis in the upper extremities, also the treatment of GCTs [18]. According to prior investigations, this high potential of TEE might be provoked by contact and irritation of vascular walls with the port material [18]. In our study, patients receiving chemotherapy via a central venous access had significantly higher numbers of venous TEE compared to the administration of chemotherapy via a peripheral venous catheter (p = 0.011) and was furthermore identified as an independent risk factor for venous TEE. As recommendations are still missing, we consequently favour the administration of chemotherapy via a peripheral venous catheter and use a central venous access only in case of poor peripheral venous access or previously implanted port systems.
In our study, 93% of all patients received a prophylactic anticoagulation, which is in line with the management of thromboprophylaxis in German-speaking countries, which was analyzed using standardized questionnaire [24]. Inspite of that, 19% of all GCT patients suffered from a venous TEE undergoing platinum-based chemotherapy in the present study. Furthermore, we found that prophylactic anticoagulation was not a predictor for the occurrence of venous TEE and that the anticoagulation regimes and dosages did not significantly differ between patients with and without a venous TEE. The incidence of TEE was slightly higher in our dataset compared to prior studies showing a TEE rate of 8–19% [3, 5, 8, 18, 19]. However, one prior analysis showed an even higher incidence of 23.7%, not revealing any difference in the development of TEE between an extended antithrombotic prophylaxis during the complete cycle of chemotherapy and a limited prophylaxis only during hospitalization [9]. In addition, two other prior studies confirmed that anticoagulation (dosage and duration not specified) had no significant effect on the prevention of thrombosis [3, 18]. Consequently, an intensified anticoagulation using a half-therapeutic dose or even therapeutic-dose regimes in the course of chemotherapy should be discussed in patients with risk factors for a TEE to reduce the occurrence of a TEE. Furthermore, even newer anticoagulants, that might promise a more effective and convenient prophylaxis of TEE, could be used in these patients [25]. However, further studies including these different anticoagulation regimes are warranted.
Furthermore, patients with risk factors for a TEE should be monitored more intensively for the development of venous TEE. According to recent studies, monitoring using fibrin-related markers as D-dimer, soluble fibrin, fibrinogen and fibrin degradation products can also be performed in cancer patients [26,27,28]. Additionally, the PELICAN study showed that patients are not well informed about the risk factors and subsequent behavioral factors of TEE [29]. Thus, patients’ awareness of TEE should be proactively improved by their treating physicians to reduce mortality and morbidity. Furthermore, a prevention program for patients at risk, also informing about further, modifiable risk factors for thrombosis such as obesity, might reduce the relatively high incidence of 19% to suffer from a venous TEE during platinum-based chemotherapy for GCTs [30].
Certainly, there are some limitations to our study. First, the retrospective study design constitutes a restricted accuracy, which is usually considered to be of lower level of evidence compared to a prospective trial. Secondly, the relatively small number of cases limits the explanatory power of the study. Therefore, additional studies with a larger patient cohort are needed in order to further extend the present findings.
Conclusions
Taken together, patients with testicular GCTs undergoing platinum-based chemotherapy are at high risk of developing a venous TEE. However, second-line chemotherapy in the salvage setting was not associated with an increased risk of venous TEE. Elevated serum LDH, clinical stage ≥ IIC, a central venous access and presence of febrile neutropenia during or after chemotherapy were identified as independent risk factors for the development of venous TEE in patients with GCT. Additionally, venous TEE led to a significantly reduced overall survival in GCT patients receiving platinum-based chemotherapy. Arterial embolism is rare but can have tremendous impact, so early diagnosis and therapy are mandatory. As a result, patients at risk should be monitored more intensively by their treating physicians and patients’ awareness of TEE should be proactively improved.
Abbreviations
- AFP:
-
Alpha-Fetoprotein
- BEP:
-
Bleomycin, etoposide, cisplatin
- GCT:
-
Germ cell tumors
- β-hCG:
-
Human chorionic gonadotropin
- IGCCCG:
-
International germ cell cancer collaborative group
- IQR:
-
Interquartile range
- LDH:
-
Lactate dehydrogenase
- PEI:
-
Cisplatin, etopside, ifosfamide
- PC-RPLND:
-
Post-chemotherapy retroperitoneal lymph node dissection
- TIP:
-
Cisplatin, ifosfamide, paclitaxel
References
Albers P, Albrecht W, Algaba F et al (2015) Guidelines on testicular cancer: 2015 update. Eur Urol 68:1054–1068. https://doi.org/10.1016/j.eururo.2015.07.044
Donnellan E, Khorana AA (2017) Cancer and venous thromboembolic disease: a review. Oncologist 22:199–207. https://doi.org/10.1634/theoncologist.2016-0214
Piketty A-C, Fléchon A, Laplanche A et al (2005) The risk of thrombo-embolic events is increased in patients with germ-cell tumours and can be predicted by serum lactate dehydrogenase and body surface area. Br J Cancer 93:909–914. https://doi.org/10.1038/sj.bjc.6602791
Fosså SD, Aass N, Harvei S, Tretli S (2004) Increased mortality rates in young and middle-aged patients with malignant germ cell tumours. Br J Cancer 90:607–612. https://doi.org/10.1038/sj.bjc.6601558
Gizzi M, Oberic L, Massard C et al (2016) Predicting and preventing thromboembolic events in patients receiving cisplatin-based chemotherapy for germ cell tumours. Eur J Cancer 69:151–157. https://doi.org/10.1016/j.ejca.2016.10.003
Heidegger I, Porres D, Veek N et al (2017) Predictive factors for developing venous thrombosis during cisplatin-based chemotherapy in testicular cancer. Urol Int 99:104–109. https://doi.org/10.1159/000471888
Dieckmann K-P, Gerl A, Witt J et al (2010) Myocardial infarction and other major vascular events during chemotherapy for testicular cancer. Ann Oncol 21:1607–1611. https://doi.org/10.1093/annonc/mdp597
Weijl NI, Rutten MFJ, Zwinderman AH et al (2000) Thromboembolic events during chemotherapy for germ cell cancer: a cohort study and review of the literature. J Clin Oncol 18:2169–2178. https://doi.org/10.1200/JCO.2000.18.10.2169
Solari L, Krönig M, Ihorst G et al (2016) High rates of thromboembolic events in patients with germ cell cancer undergoing cisplatin-based polychemotherapy. Urol Int 96:399–405. https://doi.org/10.1159/000445126
Bezan A, Posch F, Ploner F et al (2017) Risk stratification for venous thromboembolism in patients with testicular germ cell tumors. PLoS One 12:e0176283. https://doi.org/10.1371/journal.pone.0176283
Mandala M, Falanga A, Roila F, ESMO Guidelines Working Group (2011) Management of venous thromboembolism (VTE) in cancer patients: ESMO clinical practice guidelines. Ann Oncol 22:vi85–vi92. https://doi.org/10.1093/annonc/mdr392
Burness CB, Perry CM (2014) Rivaroxaban: a review of its use in the treatment of deep vein thrombosis or pulmonary embolism and the prevention of recurrent venous thromboembolism. Drugs 74:243–262. https://doi.org/10.1007/s40265-013-0174-4
Babyak MA (2004) What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med 66:411–421
Moore RA, Adel N, Riedel E et al (2011) High incidence of thromboembolic events in patients treated with cisplatin-based chemotherapy: a large retrospective analysis. J Clin Oncol 29:3466–3473. https://doi.org/10.1200/JCO.2011.35.5669
Shlebak AA, Smith DB (1997) Incidence of objectively diagnosed thromboembolic disease in cancer patients undergoing cytotoxic chemotherapy and/or hormonal therapy. Cancer Chemother Pharmacol 39:462–466. https://doi.org/10.1007/s002800050599
Khorana AA (2010) Venous thromboembolism and prognosis in cancer. Thromb Res 125:490–493. https://doi.org/10.1016/j.thromres.2009.12.023
Chaturvedi S, Sidana S, Elson P et al (2014) Symptomatic and incidental venous thromboembolic disease are both associated with mortality in patients with prostate cancer. PLoS One 9:e94048. https://doi.org/10.1371/journal.pone.0094048
Honecker F, Koychev D, Luhmann AD et al (2013) Venous thromboembolic events in germ cell cancer patients undergoing platinum-based chemotherapy. Onkologie 36:7–7. https://doi.org/10.1159/000355652
Srikanthan A, Tran B, Beausoleil M et al (2015) Large retroperitoneal lymphadenopathy as a predictor of venous thromboembolism in patients with disseminated germ cell tumors treated with chemotherapy. J Clin Oncol 33:582–587. https://doi.org/10.1200/JCO.2014.58.6537
Mead GM, Stenning SP (1997) The international germ cell consensus classification: a new prognostic factor-based staging classification for metastatic germ cell tumours. Clin Oncol (R Coll Radiol) 9:207–209
Kyriazi V, Theodoulou E (2013) Assessing the risk and prognosis of thrombotic complications in cancer patients. Arch Pathol Lab Med 137:1286–1295. https://doi.org/10.5858/arpa.2012-0490-RA
Khorana AA, Francis CW, Culakova E et al (2006) Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol 24:484–490. https://doi.org/10.1200/JCO.2005.03.8877
Lin J, Proctor MC, Varma M et al (2003) Factors associated with recurrent venous thromboembolism in patients with malignant disease. J Vasc Surg 37:976–983. https://doi.org/10.1067/mva.2003.191
Nestler T, Huber J, Laury AM et al (2018) Thromboprophylaxis and the route of administration of chemotherapy in testicular cancer patients in German-speaking countries. World J Urol. https://doi.org/10.1007/s00345-018-2222-x
Carrier M, Lee AY (2009) Prophylactic and therapeutic anticoagulation for thrombosis—major issues in oncology. Nat Clin Pract Oncol 6:74–84. https://doi.org/10.1038/ncponc1244
Yamashita Y, Wada H, Nomura H et al (2014) Elevated fibrin-related markers in patients with malignant diseases frequently associated with disseminated intravascular coagulation and venous thromboembolism. Intern Med 53:413–419
Li XD, Guo SJ, Chen SL et al (2017) Clinical outcome of postchemotherapy retroperitoneal lymph node dissection and predicting retroperitoneal histology in advanced nonseminomatous germ cell tumours of the testis. Zhonghua Wai Ke Za Zhi 55:603–607. https://doi.org/10.3760/cma.j.issn.0529-5815.2017.08.010
Madoiwa S (2017) Management of venous thromboembolism in cancer patients. Gan To Kagaku Ryoho 44:2064–2071
Noble S, Prout H, Nelson A (2015) Patients’ Experiences of LIving with CANcer-associated thrombosis: the PELICAN study. Patient Prefer Adherence 9:337. https://doi.org/10.2147/PPA.S79373
Cushman M (2007) Epidemiology and risk factors for venous thrombosis. Semin Hematol 44:62–69. https://doi.org/10.1053/j.seminhematol.2007.02.004
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MG: manuscript editing. KG: data collection or management, data analysis. IH: manuscript editing. AH: project development, manuscript editing, supervision. MH: data analysis, manuscript editing. TN: manuscript editing. PP: project development, data collection or management, data analysis, manuscript writing/editing. DP: project development, manuscript editing, supervision. JS: manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Paffenholz, P., Grein, K., Heidegger, I. et al. Predictors of thrombosis in testicular cancer during platinum-based chemotherapy. World J Urol 37, 1907–1916 (2019). https://doi.org/10.1007/s00345-018-2598-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2598-7