Abstract
Objective
To characterize the current evaluation, and efficacy of treatments in patients with the primary complaint of nocturia.
Methods
A retrospective chart review was performed of new patient encounters seen in a tertiary urology practice from May 2010 to September 2016 with the primary diagnosis of nocturia (ICD-9 788.43 and ICD-10 R35.1).
Results
595 patients were identified. 403 met inclusion criteria. The median patient reported that nocturia episodes were 4 (1–20). 192 patients (48%) reported previous treatment for nocturia. After the index visit, a bladder diary (BD) was utilized in 50% of patients, with a 62% (n = 124) completion rate at follow-up visit. On BD analysis, the most common etiologies of nocturia were nocturnal polyuria 76% (n = 90) and overactive bladder in 21% (n = 26). Patient reported improvement with therapy after BD completion was 46% (n = 34), similar to patients without voiding diaries (43% improvement, n = 153). Anticholinergics and alpha blockers were the most commonly recommended drug, but no specific medication was associated with nocturia improvement. Oral desmopressin was used in 5% of patients.
Conclusion
Nocturia is a common condition and very commonly patients have sought treatment prior to presentation. Bladder diaries were recommended to half of the patients. Patient reported that improvement did not seem to correlate with completion of a bladder diary. Though most patients had NP the use of desmopressin was very low. Current treatments used in managing nocturia may lack efficacy.


Similar content being viewed by others
References
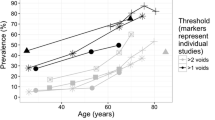
Cornu J-N et al (2012) A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management–a systematic review and meta-analysis. Eur Urol 62:877–890
DuBeau CE, Yalla SV, Resnick NM (1995) Implications of the most bothersome prostatism symptom for clinical care and outcomes research. J Am Geriatr Soc 43:985–992
Tikkinen KAO et al (2010) Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol 57:488–496
Nimeh T, Alvarez P, Mufarreh N, Lerner LB (2015) Nocturia: current evaluation and treatment for urology. Curr Urol Rep 16:66
van Kerrebroeck P et al (2002) The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:179–183
Bosch JLHR, Weiss JP (2013) The prevalence and causes of nocturia. J Urol 189:S86–S92
Aizen J, Lee CL, Olugbade K, Weiss JP (2015) AUA update series 2015, evaluation and management of nocturia. Lesson 38:34. https://auau.auanet.org/node/4884. Accessed 9 Dec 2016
Rudy D, Cline K, Harris R, Goldberg K, Dmochowski R (2006) Multicenter phase III trial studying trospium chloride in patients with overactive bladder. Urology 67:275–280
Eisenhardt A, Schneider T, Cruz F, Oelke M (2014) Consistent and significant improvement of nighttime voiding frequency (nocturia) with silodosin in men with LUTS suggestive of BPH: pooled analysis of three randomized, placebo-controlled, double-blind phase III studies. World J Urol 32:1119–1125
Oelke M, Anderson P, Wood R, Holm-Larsen T (2016) Nocturia is often inadequately assessed, diagnosed and treated by physicians: results of an observational, real-life practice database containing 8659 European and US-American patients. Int J Clin Pract 70:940–949
Jimenez-Cidre MA et al (2015) The 3-day bladder diary is a feasible, reliable and valid tool to evaluate the lower urinary tract symptoms in women. Neurourol Urodyn 34:128–132
Jayadevappa R, Newman DK, Chhatre S, Wein AJ (2015) Medication adherence in the management of nocturia: challenges and solutions. Patient Prefer Adherence 9:77–85
Chen F-Y et al (2007) Perception of nocturia and medical consulting behavior among community-dwelling women. Int Urogynecol J Pelvic Floor Dysfunct 18:431–436
Wennberg A-L et al (2009) Lower urinary tract symptoms: lack of change in prevalence and help-seeking behaviour in two population-based surveys of women in 1991 and 2007. BJU Int 104:954–959
Johnson TM et al (2003) Changes in nocturia from medical treatment of benign prostatic hyperplasia: secondary analysis of the Department of Veterans Affairs Cooperative Study Trial. J Urol 170:145–148
van Doorn B, Kok ET, Blanker MH, Westers P, Bosch JLHR (2014) Determinants of nocturia: the Krimpen study. J Urol 191:1034–1039
van Kerrebroeck P et al (2007) Desmopressin in the treatment of nocturia: a double-blind, placebo-controlled study. Eur Urol 52:221–229
Weiss JP, Zinner NR, Klein BM, Nørgaard JP (2012) Desmopressin orally disintegrating tablet effectively reduces nocturia: results of a randomized, double-blind, placebo-controlled trial. Neurourol Urodyn 31:441–447
Noctiva [package insert] (2017). https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/201656lbl.pdf. Accessed 1 May 2018
Acknowledgements
None.
Funding
There was no source of funding from any company.
Author information
Authors and Affiliations
Contributions
SD protocol/project development, data collection, data analysis, manuscript writing/editing. BP manuscript writing/editing. AR data collection, data analysis. NR data collection. VN data collection, manuscript writing/editing, data analysis. BB protocol/project development, manuscript writing/editing
Corresponding author
Ethics declarations
Conflict of interest
Siri Drangsholt: None; Maria Juliana Arcila Ruiz: None; Benjamin Brucker: Avadel, Serenity, Allergan, Medtronic, Watkins-Conti, Ipsen; Avadel- Consultant and Speaker; Serenity—Consultant; Allergan—Speaker, Consultant, Investigator; Metronic- Investigator; Watkins-Conti- advisor; Ipsen—Investigator; Victor Nitti: Owns stock in Serenity; Benoit Peyronnet: Astellas, Medtronic, Allergan, Boston Scientific, Ipsen; Astellas—Consultant; Allergan—Consultant; Metronic—Consultant; Boston Scientific—Consultant; Ipsen—Investigator; Nirit Rosenblum: None.
Ethical approval
This study was approved by the New York University Institutional Review Board as it involved research on human subjects.
Informed consent
This study was retrospective using de-identified data and thus informed consent was not needed.
Rights and permissions
About this article
Cite this article
Drangsholt, S., Ruiz, M.J.A., Peyronnet, B. et al. Diagnosis and management of nocturia in current clinical practice: who are nocturia patients, and how do we treat them?. World J Urol 37, 1389–1394 (2019). https://doi.org/10.1007/s00345-018-2511-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2511-4