Abstract
Introduction
Many LUTS/BPH treatments currently available may affect sexual function (SD). We wished to assess urologists’ attitude and practice in this area.
Methods
Attendees of an international meeting were randomly selected, interviewed and stratified by professional status and LUTS/BPH cases seen per month. There were four questions: treatment options offered, frequency of discussing erectile dysfunction (ED) with each treatment, frequency of discussing ejaculatory dysfunction (EjD) with each treatment, and offering alternative treatment based on the risks of sexual dysfunction.
Results
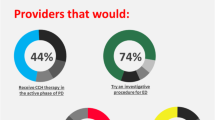
199 of the 245 interviewed (81%) were urologists. The most common treatments offered were α-blockers (99.5%), 5-ARI (95.0%) and TURP (92.5%). About 70% of the specialists discuss ED before α-blockers (not known to cause ED). Regarding EjD, 70% discuss this prior to prescribing α-blockers, 60% before 5-ARI therapy, while 80% before TURP. A significant minority fails to discuss this complication in all areas. Many respondents do not routinely discuss alternative therapies on the risk of SD. The higher the caseload, the less likely was a urologist to offer alternative therapies, with 37% of urologists seeing over 30 LUTS/BPH patients per month stating they would “Not at all often” offer alternative therapies for this reason.
Conclusions
There is a significant discrepancy in attitudes to counselling patients on SD related to LUTS/BPH treatments. This may, in some cases, affect the validity of consent to the treatment. Most urologists do not discuss alternative treatments with patients based on the risks of different outcomes and complications, and this seems more marked in those with the busier practices. This may sit ill with the concept of personalised healthcare.





Similar content being viewed by others
References
van Dijk MM, de la Rosette JJ, Michel MC (2006) Effects of alpha (1)-adrenoceptor antagonists on male sexual function. Drugs. 66:287–301
Roehrborn CG, Siami P, Barkin J et al (2009) The influence of baseline parameters on changes in international prostate symptom score with dutasteride, tamsulosin, and combination therapy among men with symptomatic benign prostatic hyperplasia and an enlarged prostate: 2-year data from the CombAT study. Eur Urol. 55:461–471
Roehrborn CG, Boyle P, Nickel JC et al (2002) Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 60:434–441
Roehrborn CG, Siami P, Barkin J et al (2008) The effects of dutasteride, tamsulosin and combination therapy on lower urinary tract symptoms in men with benign prostatic hyperplasia and prostatic enlargement: 2-year results from the CombAT study. J Urol 179:616–621 (discussion 621)
McConnell JD, Roehrborn CG, Bautista OM et al (2003) The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 349:2387–2398
Roehrborn CG, Siami P, Barkin J et al (2010) The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol 57:123–131
Naslund MJ, Miner M (2007) A review of the clinical efficacy and safety of 5alpha-reductase inhibitors for the enlarged prostate. Clin Ther 29:17–25
Madersbacher S, Marberger M (1999) Is transurethral resection of the prostate still justified? BJU Int. 83:227–237
McConnell JD BM, Bruskewitz RC. Benign prostatic hyperplasia: diagnosis and treatment. In: (AHCPR) AfHCPaR (ed), vol 81994.
Emberton M, Neal DE, Black N et al (1996) The effect of prostatectomy on symptom severity and quality of life. Br J Urol 77:233–247
Horasanli K, Silay MS, Altay B, Tanriverdi O, Sarica K, Miroglu C (2008) Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology 71:247–251
Alivizatos G, Skolarikos A, Chalikopoulos D et al (2008) Transurethral photoselective vaporization versus transvesical open enucleation for prostatic adenomas > 80 ml: 12-mo results of a randomized prospective study. Eur Urol. 54:427–437
Bouchier-Hayes DM, Anderson P, Van Appledorn S, Bugeja P, Costello AJ (2006) KTP laser versus transurethral resection: early results of a randomized trial. J Endourol 20:580–585
Naspro R, Suardi N, Salonia A et al (2006) Holmium laser enucleation of the prostate versus open prostatectomy for prostates > 70 g: 24-month follow-up. Eur Urol. 50:563–568
Briganti A, Naspro R, Gallina A et al (2006) Impact on sexual function of holmium laser enucleation versus transurethral resection of the prostate: results of a prospective, 2-center, randomized trial. J Urol. 175:1817–1821
Tabatabaei S, Choi B, Muir G. 2272 Ejaculation-preserving photoselective vaporization of prostate (EP-PVP): six years experience from a multi-centre study. J Urol 185:e910–e911
Kim M, Song SH, Ku JH, Kim HJ, Paick JS (2015) Pilot study of the clinical efficacy of ejaculatory hood sparing technique for ejaculation preservation in Holmium laser enucleation of the prostate. Int J Impot Res 27:20–24
Bruskewitz R, Issa MM, Roehrborn CG et al (1998) A prospective, randomized 1-year clinical trial comparing transurethral needle ablation to transurethral resection of the prostate for the treatment of symptomatic benign prostatic hyperplasia. J Urol 159:1588–1593 (discussion 1593–1584)
Hill B, Belville W, Bruskewitz R et al (2004) Transurethral needle ablation versus transurethral resection of the prostate for the treatment of symptomatic benign prostatic hyperplasia: 5-year results of a prospective, randomized, multicenter clinical trial. J Urol. 171:2336–2340
Cimentepe E, Unsal A, Saglam R (2003) Randomized clinical trial comparing transurethral needle ablation with transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: results at 18 months. J Endourol/Endourol Soc 17:103
Woo HH, Chin PT, McNicholas TA et al (2011) Safety and feasibility of the prostatic urethral lift: a novel, minimally invasive treatment for lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH). BJU Int. 108:82–88
Acknowledgements
We thank Jacqueline Welch for the support and the statistical analysis provided.
Funding
Study funded by unrestricted educational grant from Neotract inc. Gordon Muir has received funding as investigator, consultant and mentor for both BSCI and Neotract.
Author information
Authors and Affiliations
Contributions
S Giona: Data collection and management, Data analysis, Manuscript writing. I Ganguly: Data collection. G Muir: Protocol development, Manuscript editing
Corresponding author
Ethics declarations
Conflict of interest
Study funded by unrestricted educational grant from Neotract inc. Gordon Muir has received funding as investigator, consultant and mentor for both BSCI and Neotract.
Research involving Human Participants and/or Animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required
Rights and permissions
About this article
Cite this article
Giona, S., Ganguly, I. & Muir, G. Urologists’ attitudes to sexual complications of LUTS/BPH treatments. World J Urol 36, 1449–1453 (2018). https://doi.org/10.1007/s00345-018-2283-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2283-x