Abstract
Objectives
To evaluate the long-term safety (primary objective) and efficacy/impact on quality of life (QoL, secondary objectives) of silodosin 8 mg once daily in men with LUTS/BPH.
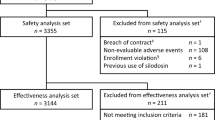
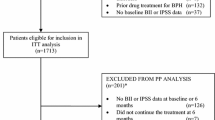
Patients and Methods
Men who completed the 12-week double-blind study with silodosin 8 mg, tamsulosin 0.4 mg, or placebo were offered to continue with the 9-month open-label study during which all patients received silodosin 8 mg once daily. Safety was assessed by analysing vital signs, electrocardiograms, laboratory tests, and adverse events. Efficacy was evaluated with the International Prostate Symptom Score (IPSS), IPSS voiding and storage sub-scores, IPSS–QoL, and maximum urinary flow rate (Q max).
Results
A total of 500 patients (mean age 66 years) entered the 9-month open-label study. Treatment-emergent adverse events (TEAE) were experienced by 33.4 % patients. Ejaculation dysfunction was the most common TEAE (9.0 %) but led to study discontinuations in only 1.6 % of patients. Dizziness without orthostatic hypotension occurred in 0.8 %. A marked reduction in total IPSS (−2.7 ± 3.8) was documented at the first visit of this extension phase in patients having de novo silodosin compared with lesser improvement in patients previously treated with silodosin (−0.82 ± 4.2) or tamsulosin (−0.83 ± 3.8). Improvements were maintained throughout the open-label phase. QoL also improved, with the greatest improvement in de novo silodosin patients. No relevant changes in Q max occurred.
Conclusions
Long-term treatment with silodosin was safe and efficacious. Abnormal ejaculation was the most common TEAE, but led to treatment discontinuation in only 1.6 % of patients. Orthostatic hypotension was not seen, and only a few patients experienced dizziness.



Similar content being viewed by others
References
Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, McKinlay JB, BACH survey investigators (2006) Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Int Med 166:2381–2387
Berry SJ, Coffey DS, Walsh PC, Ewing LL (1984) The development of human benign prostatic hyperplasia with age. J Urol 132:474–479
Sexton CC, Coyne KS, Kopp ZS, Irwin DE, Milsom I, Aiyer LP, Tubaro A, Chapple CR, Wein AJ, EpiLUTS Team (2009) The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA UK and Sweden: EpiLUTS. BJU Int 103(Suppl 3):12–23
van Koeveringe GA, Vahabi B, Andersson KE, Kirschner-Hermanns R, Oelke M (2011) Detrusor underactivity: a plea for new approaches to a common bladder dysfunction. Neurourol Urodyn 30:723–728
Oelke M, Baard J, Wijkstra H, de la Rosette JJ, Jonas U, Höfner K (2008) Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur Urol 54:419–426
Chapple CR, Roehrborn CG (2006) A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol 49:651–658
Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC, N’Dow J, Nordling J, de la Rosette J, European Association of Urology (2013) EAU Guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms, including benign prostatic obstruction. Eur Urol 64:118–140
Chapple CR (2004) Pharmacological therapy of benign prostatic hyperplasia/lower urinary tract symptoms: an overview for the practising clinician. BJU Int 94:738–744
Lepor H, Auerbach S, Puras-Baez A, Narayan P, Soloway M, Lowe F, Moon T, Leifer G, Madsen P (1992) A randomized, placebo-controlled multicenter study of the efficacy and safety of terazosin in the treatment of benign prostatic hyperplasia. J Urol 148:1467–1474
Chapple CR, Carter P, Christmas TJ et al (1994) A three month double-blind study of doxazosin as treatment for benign prostatic bladder outlet obstruction. Br J Urol 74:50–56
Fine SR, Ginsberg P (2008) Alpha-adrenergic receptor antagonists in older patients with benign prostatic hyperplasia: issues and potential complications. J Am Osteopath Assoc 108:333–337
Lowe FC (2004) Role of the newer alpha, -adrenergic-receptor antagonists in the treatment of benign prostatic hyperplasia-related lower urinary tract symptoms. Clin Ther 26:1701–1713
Souverein PC, Van Staa TP, Egberts AC, De la Rosette JJ, Cooper C, Leufkens HG (2003) Use of alpha-blockers and the risk of hip/femur fractures. J Intern Med 254:548–554
Thorpe A, Neal D (2003) Benign prostatic hyperplasia. Lancet 361:1359–1367
Michel MC, Grübbel B, Möllhoff S et al (1994) 1-Adrenoceptor affinities of drugs for the treatment of benign prostatic hyperplasia in human prostate, rat tissues and at cloned subtypes. Abstract presented at: 23rd Congress of the Société Internationale d’Urologie; September 18–24, Sydney, Australia. Abstract 649
Hatano A, Takahashi H, Tamaki M, Komeyama T, Koizumi T, Takeda M (1994) Pharmacological evidence of distinct alpha 1-adrenoceptor subtypes mediating the contraction of human prostatic urethra and peripheral artery. Br J Pharmacol 113:723–728
Tatemichi S, Kobayashi K, Maezawa A, Kobayashi M, Yamazaki Y, Shibata N (2006) Alpha1-adrenoceptor subtype selectivity and organ specificity of silodosin (KMD-3213). Yakugaku Zasshi 126:209–216
Chapple CR, Montorsi F, Tammela TL, Wirth M, Koldewijn E, Fernandez EF, European Silodosin Study Group (2011) Silodosin therapy for lower urinary tract symptoms in men with suspected benign prostatic hyperplasia: results of an international, randomized, double-blind, placebo- and active-controlled clinical trial performed in Europe. Eur Urol 59:342–352
Kawabe K, Yoshida M, Homma Y, Silodosin Clinical Study Group (2006) Silodosin, a new alpha1A-adrenoceptor-selective antagonist for treating benign prostatic hyperplasia: results of a phase III randomized, placebo-controlled, double-blind study in Japanese men. BJU Int 98:1019–1024
Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G (2009) Rapid efficacy of the highly selective alpha1A-adrenoceptor antagonist silodosin in men with signs and symptoms of benign prostatic hyperplasia: pooled results of 2 phase 3 studies. J Urol 181:2634–2640
Miller J, Carson CC (2007) Alpha blockers and ejaculatory function: a state of the art review. Curr Sex Health Rep. 4:141–144
Osman NI, Chapple CR, Cruz F, Desgrandchamps F, Llorente C, Montorsi F (2012) Silodosin: a new subtype selective alpha-1 antagonist for the treatment of lower urinary tract symptoms in patients with benign prostatic hyperplasia. Expert Opin Pharmacother 13:2085–2096
Montorsi F, Mercadante D (2013) Diagnosis of BPH and treatment of LUTS among GPs: a European survey. Int J Clin Pract 67:114–119
Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G (2009) Silodosin in the treatment of the signs and symptoms of benign prostatic hyperplasia: a 9-month, open-label extension study. Urology 74:1318–1322
van Dijk MM, de la Rosette JJ, Michel MC (2006) Effects of α1-adrenoceptor antagonists on male sexual function. Drugs 66:287–301
Roehrborn CG, Kaplan SA, Lepor H, Volinn W (2011) Symptomatic and urodynamic responses in patients with reduced or no seminal emission during silodosin treatment for LUTS and BPH. Prostate Cancer Prostatic Dis. 14:143–148
Homma Y, Kawabe K, Takeda M, Yoshida M (2010) Ejaculation disorder is associated with increased efficacy of silodosin for benign prostatic hyperplasia. Urology 76:1446–1450
Hellstrom WJ, Giuliano F, Rosen RC (2009) Ejaculatory dysfunction and its association with lower urinary tract symptoms of benign prostatic hyperplasia and BPH treatment. Urology 74:15–21
Blanker MH, Bosch JL, Groeneveld FP, Bohnen AM, Prins A, Thomas S, Hop WC (2001) Erectile and ejaculatory dysfunction in a community-based sample of men 50 to 78 years old: prevalence, concern, and relation to sexual activity. Urology 57:763–768
Hutchison A, Farmer R, Chapple C, Berges R, Pientka L, Teillac P, Borkowski A, Dobronski P (2006) Characteristics of patients presenting with LUTS/BPH in six European countries. Eur Urol 50:555–561
Acknowledgments
This study was initiated and supported by Recordati Industria Chimica e Farmaceutica SpA, Milan, Italy. The authors would like to thank Mr. Alessandro Antonellini and Mr. Massimo Casi for their valuable support with regard to study monitoring, data summary, and proof reading.
Conflicts of interest
Nadir I. Osman has no conflict of interest. Christopher R. Chapple is a consultant and researcher for Allergan, Astellas, Pfizer, and Recordati. Teuvo L. Tammela is a consultant and researcher for Astellas, Pfizer, and Recordati. Andreas Eisenhardt is speaker, advisor and/or trial participant of Berlin-Chemie, Ipsen, Janssen-Cilag, Lilly, Recordati, and Takeda. Matthias Oelke is speaker, advisor and/or trial participant of Apogepha, Astellas, GlaxoSmithKline, Lilly, Mundipharma, Pfizer, Recordati, and Sophiris.
Ethical standard
The trial was registered under clinical trials registration number NCT00359905. Ethics committee approval was obtained for each centre, and written informed consent was obtained from all study participants. The study was designed and performed according to the GCP recommendations and the 1964 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Osman, N.I., Chapple, C.R., Tammela, T.L. et al. Open-label, 9-month extension study investigating the uro-selective alpha-blocker silodosin in men with LUTS associated with BPH. World J Urol 33, 697–706 (2015). https://doi.org/10.1007/s00345-015-1519-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1519-2