Abstract
Purpose
To examine the association between positive surgical margins (PSMs) and preoperative circulating estradiol (E2), total testosterone (tT), and sex hormone–binding globulin (SHBG) in patients undergoing retropubic radical prostatectomy (RRP).
Methods
A cohort of 665 non-screened patients who underwent RRP at a single institute was studied. Serum tT, E2, and SHBG were measured the day before surgery (8–10 am) in all cases. Logistic regression models tested the association between predictors [e.g., PSA, clinical stage, biopsy Gleason sum, body mass index (BMI), tT, E2, and SHBG] and PSM. Circulating tT was included in the model as both a continuous variable and a categorized variable [according to the definition of hypogonadism (<3 ng/ml)].
Results
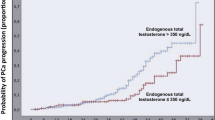
PSMs were found in 175 patients (26.3%) within the whole cohort of men and in 78 (16.2%) of the pT2 patients. Patients with PSMs had significantly higher PSA, a higher proportion of more advanced clinical stage, and a lower rate of well-differentiated biopsy Gleason sum than those without PSMs (all P ≤ 0.03). Conversely, no significant differences were found regarding age, BMI, preoperative tT, E2, and SHBG between patients with and without PSMs. At multivariate analysis, tT, hypogonadism, E2, and SHBG were not significantly associated with PSMs, after accounting for routinely available preoperative parameters.
Conclusions
In contrast to previously published data, preoperative tT was not an independent predictive factor for PSM at RRP. Likewise, hypogonadism, E2, and SHBG did not achieve independent predictor status for PSM, after accounting for routinely available preoperative parameters.
Similar content being viewed by others
References
Somford DM, van Oort IM, Cosyns JP, Witjes JA, Kiemeney LA, Tombal B. (2011) Prognostic relevance of number and bilaterality of positive surgical margins after radical prostatectomy. World J Urol [Epub ahead of print] doi:10.1007/s00345-010-0641-4
Ficarra V, Novara G, Secco S, D’Elia C, Boscolo-Berto R, Gardiman M, Cavalleri S, Artibani W (2009) Predictors of positive surgical margins after laparoscopic robot assisted radical prostatectomy. J Urol 182:2682–2688. doi:10.1016/j.juro.2009.08.037
Endogenous Hormones and Prostate Cancer Collaborative Group, Roddam AW, Allen NE, Appleby P, Key TJ (2008) Endogenous sex hormones and prostate cancer: a collaborative analysis of 18 prospective studies. J Natl Cancer Inst 100:170–183. doi:10.1093/jnci/djm323
Isbarn H, Pinthus JH, Marks LS, Montorsi F, Morales A, Morgentaler A, Schulman C (2009) Testosterone and prostate cancer: revisiting old paradigms. Eur Urol 56:48–56. doi:10.1016/j.eururo.2009.03.088
Isom-Batz G, Bianco FJ Jr, Kattan MW, Mulhall JP, Lilja H, Eastham JA (2005) Testosterone as a predictor of pathological stage in clinically localized prostate cancer. J Urol 173:1935–1937. doi:10.1097/01.ju.0000158040.33531.e7
Teloken C, Da Ros CT, Caraver F, Weber FA, Cavalheiro AP, Graziottin TM (2005) Low serum testosterone levels are associated with positive surgical margins in radical retropubic prostatectomy: hypogonadism represents bad prognosis in prostate cancer. J Urol 174:2178–2180. doi:10.1097/01.ju.0000181818.51977.29
Morgentaler A, Rhoden EL (2006) Prevalence of prostate cancer among hypogonadal men with prostate-specific antigen levels of 4.0 ng/ml or less. Urology 68:1263–1267. doi:10.1016/j.urology.2006.08.1058
Salonia A, Gallina A, Briganti A, Abdollah F, Suardi N, Capitanio U, Colombo R, Freschi M, Rigatti P, Montorsi F (2011) Preoperative hypogonadism is not an independent predictor of high-risk disease in patients undergoing radical prostatectomy. Cancer 117:3953–3962. doi:10.1002/cncr.25985
Heracek J, Urban M, Sachova J, Kuncova J, Eis V, Mandys V, Hampl R, Starka L (2007) The endocrine profiles in men with localized and locally advanced prostate cancer treated with radical prostatectomy. Neuro Endocrinol Lett 28:45–51
Bonkhoff H, Berges R (2009) The evolving role of oestrogens and their receptors in the development and progression of prostate cancer. Eur Urol 55:533–542. doi:10.1016/j.eururo.2008.10.035
Lee SE, Chung JS, Han BK, Park CS, Moon KH, Byun SS, Choe G, Hong SK (2008) Preoperative serum sex hormone-binding globulin as a predictive marker for extraprostatic extension of tumor in patients with clinically localized prostate cancer. Eur Urol 54:1324–1332. doi:10.1016/j.eururo.2008.02.032
Salonia A, Gallina A, Briganti A, Zanni G, Suardi N, Capitanio U, Colombo R, Bertini R, Freschi M, Guazzoni G, Rigatti P, Montorsi F (2010) Sex hormone-binding globulin is a significant predictor of extracapsular extension in men undergoing radical prostatectomy. BJU Int. [Epub ahead of print] doi:10.1111/j.1464-410X.2010.09582.x
Svatek RS, Jeldres C, Karakiewicz PI, Suardi N, Walz J, Roehrborn CG, Montorsi F, Slawin KM, Shariat SF (2009) Pre-treatment biomarker levels improve the accuracy of post-prostatectomy nomogram for prediction of biochemical recurrence. Prostate 69:886–894. doi:10.1002/pros.20938
Ohori M, Wheeler TM, Kattan MW, Goto Y, Scardino PT (1995) Prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol 154:1818–1824
Petak SM, Nankin HR, Spark RF, Swerdloff RS, Rodriguez-Rigau LJ, American Association of Clinical Endocrinologists (2002) Medical guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients–2002 update. Endocr Pract 8:440–456
Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, Gooren LJ, Kaufman JM, Legros JJ, Lunenfeld B, Morales A, Morley JE, Schulman C, Thompson IM, Weidner W, Wu FC, International Society of Andrology; International Society for the Study of Aging Male; European Association of Urology; European Academy of Andrology; American Society of Andrology (2009) Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA Recommendations. Eur Urol 55:121–130. doi:10.1016/j.eururo.2008.08.033
Tajar A, Forti G, O’Neill TW, Lee DM, Silman AJ, Finn JD, Bartfai G, Boonen S, Casanueva FF, Giwercman A, Han TS, Kula K, Labrie F, Lean ME, Pendleton N, Punab M, Vanderschueren D, Huhtaniemi IT, Wu FC, EMAS Group (2010) Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European male ageing study. J Clin Endocrinol Metab 95:1810–1818. doi:10.1210/jc.2009-1796
Pelzer AE, Colleselli D, Bektic J, Schaefer G, Ongarello S, Schwentner C, Pallwein L, Mitterberger M, Steiner E, Bartsch G, Horninger W (2008) Clinical and pathological features of screen vs non-screen-detected prostate cancers: is there a difference? BJU Int 102:24–27. doi:10.1111/j.1464-410X.2008.07566.x
Santoro N, Torrens J, Crawford S, Allsworth JE, Finkelstein JS, Gold EB, Korenman S, Lasley WL, Luborsky JL, McConnell D, Sowers MF, Weiss G (2005) Correlates of circulating androgens in mid-life women: the study of women’s health across the nation. J Clin Endocrinol Metab 90:4836–4845. doi:10.1210/jc.2004-2063
Pfitzenmaier J, Pahernik S, Tremmel T, Haferkamp A, Buse S, Hohenfellner M (2008) Positive surgical margins after radical prostatectomy: do they have an impact on biochemical or clinical progression? BJU Int 102:1413–1418. doi:10.1111/j.1464-410X.2008.07791.x
Boorjian SA, Karnes RJ, Crispen PL, Carlson RE, Rangel LJ, Bergstralh EJ, Blute ML (2010) The impact of positive surgical margins on mortality following radical prostatectomy during the prostate specific antigen era. J Urol 183:1003–1009. doi:10.1016/j.juro.2009.11.039
Paul A, Ploussard G, Nicolaiew N, Xylinas E, Gillion N, de la Taille A, Vordos D, Hoznek A, Yiou R, Abbou CC, Salomon L (2010) Oncologic outcome after extraperitoneal laparoscopic radical prostatectomy: midterm follow-up of 1,115 procedures. Eur Urol 57:267–272. doi:10.1016/j.eururo.2009.09.029
Yossepowitch O, Bjartell A, Eastham JA, Graefen M, Guillonneau BD, Karakiewicz PI, Montironi R, Montorsi F (2009) Positive surgical margins in radical prostatectomy: outlining the problem and its long-term consequences. Eur Urol 55:87–99. doi:10.1016/j.eururo.2008.09.051
Chun FK, Briganti A, Antebi E, Graefen M, Currlin E, Steuber T, Schlomm T, Walz J, Haese A, Friedrich MG, Ahyai SA, Eichelberg C, Salomon G, Gallina A, Erbersdobler A, Perrotte P, Heinzer H, Huland H, Karakiewicz PI (2006) Surgical volume is related to the rate of positive surgical margins at radical prostatectomy in European patients. BJU Int 98:1204–1209. doi:10.1111/j.1464-410X.2006.06442.x
Morgentaler A, Traish AM (2009) Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth. Eur Urol 55:310–320. doi:10.1016/j.eururo.2008.09.024
Massengill JC, Sun L, Moul JW, Wu H, McLeod DG, Amling C, Lance R, Foley J, Sexton W, Kusuda L, Chung A, Soderdahl D, Donahue T (2003) Pretreatment total testosterone level predicts pathological stage in patients with localized prostate cancer treated with radical prostatectomy. J Urol 169:1670–1675. doi:10.1097/01.ju.0000062674.43964.d0
Giton F, de la Taille A, Allory Y, Galons H, Vacherot F, Soyeux P, Abbou CC, Loric S, Cussenot O, Raynaud JP, Fiet J (2008) Estrone sulfate (E1S), a prognosis marker for tumor aggressiveness in prostate cancer (PCa). J Steroid Biochem Mol Biol 109:158–167. doi:10.1016/j.jsbmb.2007.10.005
Isbarn H, Jeldres C, Budäus L, Salomon G, Schlomm T, Steuber T, Chun FK, Ahyai S, Capitanio U, Haese A, Heinzer H, Huland H, Graefen M, Karakiewicz P (2009) Effect of body mass index on histopathologic parameters: results of large European contemporary consecutive open radical prostatectomy series. Urology 73:615–619. doi:10.1016/j.urology.2008.09.038
Coelho RF, Chauhan S, Orvieto MA, Palmer KJ, Rocco B, Patel VR (2010) Predictive factors for positive surgical margins and their locations after robot-assisted laparoscopic radical prostatectomy. Eur Urol 57:1022–1029. doi:10.1016/j.eururo.2010.01.040
Briganti A, Chun FK, Hutterer GC, Gallina A, Shariat SF, Salonia A, Scattoni V, Valiquette L, Montorsi F, Rigatti P, Graefen M, Huland H, Karakiewicz PI (2007) Systematic assessment of the ability of the number and percentage of positive biopsy cores to predict pathologic stage and biochemical recurrence after radical prostatectomy. Eur Urol 52:733–743. doi:10.1016/j.eururo.2007.02.054
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salonia, A., Gallina, A., Abdollah, F. et al. Preoperative circulating sex hormones are not predictors of positive surgical margins at open radical prostatectomy. World J Urol 30, 533–539 (2012). https://doi.org/10.1007/s00345-011-0761-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-011-0761-5