Abstract
Objectives
To investigate the value of extracellular volume (ECV) fraction and fat fraction (FF) derived from dual- energy CT (DECT) for predicting postpancreatectomy acute pancreatitis (PPAP) after pancreatoduodenectomy (PD).
Methods
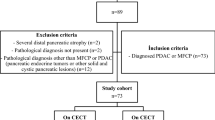
This retrospective study included patients who underwent DECT and PD between April 2022 and September 2022. PPAP was determined according to the International Study Group for Pancreatic Surgery (ISGPS) definition. Iodine concentration (IC) and FF of the pancreatic parenchyma were measured on preoperative DECT. The ECV fraction was calculated from iodine map images of the equilibrium phase. The independent predictors for PPAP were assessed by univariate and multivariable logistic regression analysis and receiver operating characteristic (ROC) curve analysis.
Results
Sixty-nine patients were retrospectively enrolled (median age, 60 years; interquartile range, 55–70 years; 47 men). Of these, nine patients (13.0%) developed PPAP. These patients had lower portal venous phase IC, equilibrium phase IC, FF, and ECV fraction, and higher pancreatic parenchymal-to-portal venous phase IC ratio and pancreatic parenchymal-to-equilibrium phase IC ratio, compared with patients without PPAP. After multivariable analysis, ECV fraction was independently associated with PPAP (odd ratio [OR], 0.87; 95% confidence interval [CI]: 0.79, 0.96; p < 0.001), with an area under the curve (AUC) of 0.839 (sensitivity 100.0%, specificity 58.3%).
Conclusions
A lower ECV fraction is independently associated with the occurrence of PPAP after PD. ECV fraction may serve as a potential predictor for PPAP after PD.
Clinical relevance statement
DECT-derived ECV fraction of pancreatic parenchyma is a promising biomarker for surgeons to preoperatively identify patients with higher risk for postpancreatectomy acute pancreatitis after PD and offer selective perioperative management.
Key Points
-
PPAP is a complication of pancreatic surgery, early identification of higher-risk patients allows for risk mitigation.
-
Lower DECT-derived ECV fraction was independently associated with the occurrence of PPAP after PD.
-
DECT aids in preoperative PAPP risk stratification, allowing for appropriate treatment to minimize complications.





Similar content being viewed by others
Abbreviations
- CECT:
-
Contrast-enhanced computed tomography
- DECT:
-
Dual-energy CT
- ECV:
-
Extracellular volume
- FF:
-
Fat fraction
- IC:
-
Iodine concentration
- PD:
-
Pancreatoduodenectomy
- POPF:
-
Postoperative pancreatic fistula
- PPAP:
-
Postpancreatectomy acute pancreatitis
References
Marchegiani G, Barreto SG, Bannone E et al (2022) Postpancreatectomy acute pancreatitis (PPAP): definition and grading From the International Study Group for Pancreatic Surgery (ISGPS). Ann Surg 275:663–672
Chen H, Wang W, Ying X et al (2020) Predictive factors for postoperative pancreatitis after pancreaticoduodenectomy: a single-center retrospective analysis of 1465 patients. Pancreatology 20:211–216
Globke B, Timmermann L, Klein F et al (2020) Postoperative acute necrotizing pancreatitis of the pancreatic remnant (POANP): a new definition of severe pancreatitis following pancreaticoduodenectomy. HPB (Oxford) 22:445–451
Loos M, Strobel O, Dietrich M et al (2021) Hyperamylasemia and acute pancreatitis after pancreatoduodenectomy: two different entities. Surgery 169:369–376
Zimmitti G, Langella S, Sega V et al (2021) Serum amylase elevation following pancreatoduodenectomy with pancreatogastrostomy is strongly associated with major complications. ANZ J Surg 91:348–354
Bannone E, Andrianello S, Marchegiani G et al (2021) Postoperative hyperamylasemia (POH) and acute pancreatitis after pancreatoduodenectomy (POAP): state of the art and systematic review. Surgery 169:377–387
Wu S, Wu H, Xu G et al (2022) Risk factors and clinical impacts of post-pancreatectomy acute pancreatitis after pancreaticoduodenectomy: a single-center retrospective analysis of 298 patients based on the ISGPS definition and grading system. Front Surg 9:916486
Bannone E, Andrianello S, Marchegiani G et al (2018) Postoperative acute pancreatitis following pancreaticoduodenectomy: a determinant of fistula potentially driven by the intraoperative fluid management. Ann Surg 268:815–822
Chen H, Fu N, Zhong J et al (2023) Enhancement pattern of the pancreatic parenchyma predicts postpancreatectomy acute pancreatitis after pancreaticoduodenectomy. Eur Radiol 34:6–15
Tang B, Lin Z, Ma Y et al (2021) A modified alternative fistula risk score (a-FRS) obtained from the computed tomography enhancement pattern of the pancreatic parenchyma predicts pancreatic fistula after pancreatoduodenectomy. HPB (Oxford) 23:1759–1766
Shi H-Y, Lu Z-P, Li M-N, Ge Y-Q, Jiang K-R, Xu Q (2022) Dual-energy CT iodine concentration to evaluate postoperative pancreatic fistula after pancreatoduodenectomy. Radiology 304:65–72
Jablonowski R, Wilson MW, Do L, Hetts SW, Saeed M (2015) Multidetector CT measurement of myocardial extracellular volume in acute patchy and contiguous infarction: validation with microscopic measurement. Radiology 274:370–378
Kumar V, Harfi TT, He X et al (2019) Estimation of myocardial fibrosis in humans with dual energy CT. J Cardiovasc Comput Tomogr 13:315–318
Zhou Z, Gao Y, Wang H et al (2021) Myocardial extracellular volume fraction analysis in doxorubicin-induced beagle models: comparison of dual-energy CT with equilibrium contrast-enhanced single-energy CT. Cardiovasc Diagn Ther 11:102–110
Bandula S, Punwani S, Rosenberg WM et al (2015) Equilibrium contrast-enhanced CT imaging to evaluate hepatic fibrosis: initial validation by comparison with histopathologic sampling. Radiology 275:136–143
Bak S, Kim JE, Bae K et al (2020) Quantification of liver extracellular volume using dual-energy CT: utility for prediction of liver-related events in cirrhosis. Eur Radiol 30:5317–5326
Sofue K, Tsurusaki M, Mileto A et al (2018) Dual-energy computed tomography for non-invasive staging of liver fibrosis: Accuracy of iodine density measurements from contrast-enhanced data. Hepatol Res 48:1008–1019
Sofue K, Ueshima E, Masuda A et al (2022) Estimation of pancreatic fibrosis and prediction of postoperative pancreatic fistula using extracellular volume fraction in multiphasic contrast-enhanced CT. Eur Radiol 32:1770–1780
Fukukura Y, Kumagae Y, Higashi R et al (2020) Extracellular volume fraction determined by equilibrium contrast-enhanced dual-energy CT as a prognostic factor in patients with stage IV pancreatic ductal adenocarcinoma. Eur Radiol 30:1679–1689
Hyodo T, Yada N, Hori M et al (2017) Multimaterial decomposition algorithm for the quantification of liver fat content by using Fast-Kilovolt-Peak switching dual-energy CT: clinical evaluation. Radiology 283:108–118
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Ansorge C, Strömmer L, Andrén-Sandberg Å, Lundell L, Herrington MK, Segersvärd R (2012) Structured intraoperative assessment of pancreatic gland characteristics in predicting complications after pancreaticoduodenectomy. Br J Surg 99:1076–1082
El Nakeeb A, Salah T, Sultan A et al (2013) Pancreatic anastomotic leakage after pancreaticoduodenectomy. Risk factors, clinical predictors, and management (single center experience). World J Surg 37:1405–1418
Sugimoto M, Takahashi S, Kojima M et al (2014) What is the nature of pancreatic consistency? Assessment of the elastic modulus of the pancreas and comparison with tactile sensation, histology, and occurrence of postoperative pancreatic fistula after pancreaticoduodenectomy. Surgery 156:1204–1211
Nahm CB, Brown KM, Townend PJ et al (2018) Acinar cell density at the pancreatic resection margin is associated with post-pancreatectomy pancreatitis and the development of postoperative pancreatic fistula. HPB (Oxford) 20:432–440
Nahm CB, Lui I, Naidoo CS et al (2019) Density and enhancement of the pancreatic tail on computer tomography predicts acinar score and pancreatic fistula after pancreatoduodenectomy. HPB (Oxford) 21:604–611
Bockman DE (1992) Microvasculature of the pancreas. Relation to pancreatitis. Int J Pancreatol 12:11–21
Kim PK, Hong YJ, Sakuma H et al (2018) Myocardial extracellular volume fraction and change in hematocrit level: MR evaluation by using T1 mapping in an experimental model of anemia. Radiology 288:93–98
Fukukura Y, Kumagae Y, Higashi R et al (2019) Extracellular volume fraction determined by equilibrium contrast-enhanced multidetector computed tomography as a prognostic factor in unresectable pancreatic adenocarcinoma treated with chemotherapy. Eur Radiol 29:353–361
Masamune A, Watanabe T, Kikuta K, Shimosegawa T (2009) Roles of pancreatic stellate cells in pancreatic inflammation and fibrosis. Clin Gastroenterol Hepatol 7:S48–S54
Klöppel G, Detlefsen S, Feyerabend B (2004) Fibrosis of the pancreas: the initial tissue damage and the resulting pattern. Virchows Arch 445:1–8
Mathur A, Pitt HA, Marine M et al (2007) Fatty pancreas: a factor in postoperative pancreatic fistula. Ann Surg 246:1058–1064
Sugimoto M, Takahashi S, Kojima M, Kobayashi T, Gotohda N, Konishi M (2017) In patients with a soft pancreas, a thick parenchyma, a small duct, and fatty infiltration are significant risks for pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg 21:846–854
Yoon JH, Lee JM, Lee KB et al (2016) Pancreatic steatosis and fibrosis: quantitative assessment with preoperative multiparametric MR imaging. Radiology 279:140–150
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Qing Xu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohort overlap has been reported.
Methodology
-
Retrospective
-
Diagnostic or prognostic study
-
Performed at one institution
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bai, XH., Yin, J., Yu, SY. et al. Extracellular volume fraction derived from dual-energy CT: a potential predictor for acute pancreatitis after pancreatoduodenectomy. Eur Radiol (2024). https://doi.org/10.1007/s00330-024-10750-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-024-10750-3