Abstract
Objective
To determine if macroscopic intralesional fat detected in bone lesions on CT by Hounsfield unit (HU) measurement and on MRI by macroscopic assessment excludes malignancy.
Materials and methods
All consecutive CT-guided core needle biopsies (CNB) of non-spinal bone lesions performed at a tertiary center between December 2005 and September 2021 were reviewed. Demographic and histopathology data were recorded. All cases with malignant histopathology were selected, and imaging studies were reviewed. Two independent readers performed CT HU measurements on all bone lesions using a circular region of interest (ROI) to quantitate intralesional fat density (mean HU < −30). MRI images were reviewed to qualitatively assess for macroscopic intralesional fat signal in a subset of patients. Inter-reader agreement was assessed with Cronbach’s alpha and intraclass correlation coefficient.
Results
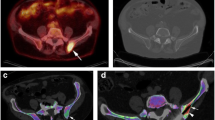
In 613 patients (mean age 62.9 years (range 19–95 years), 47.6% female), CT scans from the CNB of 613 malignant bone lesions were reviewed, and 212 cases had additional MRI images. Only 3 cases (0.5%) demonstrated macroscopic intralesional fat on either CT or MRI. One case demonstrated macroscopic intralesional fat density on CT in a case of metastatic prostate cancer. Two cases demonstrated macroscopic intralesional fat signal on MRI in cases of chondrosarcoma and osteosarcoma. Inter-reader agreement was excellent (Cronbach’s alpha, 0.95–0.98; intraclass correlation coefficient, 0.90–0.97).
Conclusion
Malignant lesions rarely contain macroscopic intralesional fat on CT or MRI. While CT is effective in detecting macroscopic intralesional fat in primarily lytic lesions, MRI may be better for the assessment of heterogenous and infiltrative lesions with mixed lytic and sclerotic components.
Clinical relevance statement
Macroscopic intralesional fat is rarely seen in malignant bone tumors and its presence can help to guide the diagnostic workup of bone lesions.
Key Points
• Presence of macroscopic intralesional fat in bone lesions has been widely theorized as a sign of benignity, but there is limited supporting evidence in the literature.
• CT and MRI are effective in evaluating for macroscopic intralesional fat in malignant bone lesions with excellent inter-reader agreement.
• Macroscopic intralesional fat is rarely seen in malignant bone lesions.




Similar content being viewed by others
Abbreviations
- CNB:
-
Core needle biopsies
- HU:
-
Hounsfield unit
- MSK:
-
Musculoskeletal
- PACS:
-
Picture archiving and communication system
- ROI:
-
Region of interest
References
Schweitzer ME, Levine C, Mitchell DG et al (1993) Bull’s-eyes and halos: useful MR discriminators of osseous metastases. Radiology 188:249–252
Simpfendorfer CS, Ilaslan H, Davies AM et al (2008) Does the presence of focal normal marrow fat signal within a tumor on MRI exclude malignancy? An analysis of 184 histologically proven tumors of the pelvic and appendicular skeleton. Skeletal Radiol 37:797–804
Chung CB, Murphey M, Cho G et al (2005) Osseous lesions of the pelvis and long tubular bones containing both fat and fluid-like signal intensity: an analysis of 28 patients. Eur J Radio 53:103–109
Kenneally BE, Gutowski CJ, Reynolds AW et al (2015) Utility of opposed-phase magnetic resonance imaging in differentiating sarcoma from benign bone lesions. J Bone Oncology 4:110–114
Omoumi P (2022) The Dixon method in musculoskeletal MRI: from fat-sensitive to fat-specific imaging. Skeletal Radiol 51:1365–1369
Park S, Do Huh J (2022) Differentiation of bone metastases from benign red marrow depositions of the spine: the role of fat-suppressed T2-weighted imaging compared to fat fraction map. Eur Radiol 32:6730–6738
Kim YP, Kannengiesser S, Paek MY et al (2014) Differentiation between focal malignant marrow-replacing lesions and benign red marrow deposition of the spine with T2*-corrected fat-signal fraction map using a three-echo volume interpolated breath-hold gradient echo Dixon sequence. Korean J Radiol 15:781
Douis H, Davies AM, Jeys L, Sian P (2016) Chemical shift MRI can aid in the diagnosis of indeterminate skeletal lesions of the spine. Eur Radiol 26(4):932–40
Zampa V, Cosottini M, Michelassi M et al (2002) Value of opposed-phase gradient-echo technique in distinguishing between benign and malignant vertebral lesions. Eur Radiol 12:1811–1818
Dreizin D, Ahlawat S, Del Grande F, Fayad LM (2014) Gradient-echo in-phase and opposed-phase chemical shift imaging: role in evaluating bone marrow. Clin Radiol 69:648–657
Douis H, Davies AM, Jeys L, Sian P (2016) Chemical shift MRI can aid in the diagnosis of indeterminate skeletal lesions of the spine. Eur Radiol 26:932–940
Ladd LM, Roth TD (2017) Computed tomography and magnetic resonance imaging of bone tumors. Semin Roentgenol 52:209–226
Nascimento D, Suchard G, Hatem M, De Abreu A (2014) The role of magnetic resonance imaging in the evaluation of bone tumours and tumour-like lesions. Insights Imaging 5:419–440
Kim WH, Kim CG, Kim DW (2012) Optimal CT number range for adipose tissue when determining lean body mass in whole-body F-18 FDG PET/CT studies. Nucl Med Mol Imaging 46:294–299
Jang S, Graffy PM, Ziemlewicz TJ et al (2019) Opportunistic osteoporosis screening at routine abdominal and thoracic CT: normative L1 trabecular attenuation values in more than 20,000 adults. Radiology 291:360–367
George D, Mallery P (2003) SPSS for Windows step by step: a simple guide and reference. 11.0 update, 4th ed. Boston: Allyn & Bacon. 231
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropractic Med 15:155–163
Stacy GS, Lo R, Montag A (2015) Infarct-associated bone sarcomas: multimodality imaging findings. AJR Am J Roentgenol 205:W432–W441
Hansford BG, Hanrahan CJ, Girard N et al (2020) Untreated plasmacytoma of bone containing macroscopic intralesional fat and mimicking intraosseous lipoma: a case report and review of the literature. Clin Imaging 64:18–23
Tiemeier GL, Brown JM, Pratap SE et al (2018) Pleomorphic liposarcoma of bone: a rare primary malignant bone tumour. Clin Sarcoma Res 8:2
Downey EF, Worsham GF, Brower AC (1982) Liposarcoma of bone with osteosarcomatous foci: case report and review of the literature. Skeletal Radiol 8:47–50
Torigoe T, Matsumoto T, Terakado A et al (2006) Primary pleomorphic liposarcoma of bone: MRI findings and review of the literature. Skeletal Radiol 35:536–538
Palczewski P, Swiątkowski J, Gołębiowski M, Błasińska-Przerwa K (2011) Intraosseous lipomas: a report of six cases and a review of literature. Pol J Radiol 76:52–59
Milgram James W (1990) Malignant transformation in bone lipomas. Skeletal Radiol 19(5):347–52
McMenamin DS, Stuckey SL, Potgieter GJ (2007) T1 Hyperintense vertebral column melanoma metastases. AJNR Am J Neuroradiol 28:1817–1818
Daldrup-Link HE, Henning T, Link TM (2007) MR imaging of therapy-induced changes of bone marrow. Eur Radiol 17:743–761
Park S, Huh JD (2023) Bone metastases with post-treatment intralesional fatty content of the spine: imaging features from T1-weighted imaging with CT finding correlations. Acta Radiol 64:153–163
Lecouvet FE, Larbi A, Pasoglou V et al (2013) MRI for response assessment in metastatic bone disease. Eur Radiol 23:1986–1997
Swartz PG, Roberts CC (2009) Radiological reasoning: bone marrow changes on MRI. AJR Am J Roentgenol 193:S1–S4
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jim S. Wu, MD.
Conflict of Interest
Hillary W. Garner has a Know-How Agreement with Immersive Touch®.
The other authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Jennifer Ni Mhuircheartaigh is a member of the European Radiology Editorial Board. She has not taken part in the review or selection process of this article.
Statistics and Biometry
No complex statistical methods were necessary for this paper.
Informed Consent
Written informed consent was waived by the institutional review board.
Ethical Approval
The institutional review board approval from the Beth Israel Deaconess Medical Center Committee on Clinical Investigations was obtained.
Study subjects or cohorts overlap
None.
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zandee van Rilland, E.D., Yoon, SY., Garner, H.W. et al. Does the presence of macroscopic intralesional fat exclude malignancy? An analysis of 613 histologically proven malignant bone lesions. Eur Radiol (2024). https://doi.org/10.1007/s00330-024-10687-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-024-10687-7