Abstract
Objectives
To propose a novel model-free data-driven approach based on the voxel-wise mapping of DCE-MRI time-intensity-curve (TIC) profiles for quantifying and visualizing hemodynamic heterogeneity and to validate its potential clinical applications.
Materials and methods
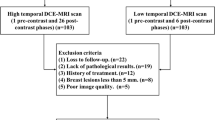
From December 2018 to July 2022, 259 patients with 325 pathologically confirmed breast lesions who underwent breast DCE-MRI were retrospectively enrolled. Based on the manually segmented breast lesions, the TIC of each voxel within the 3D whole lesion was classified into 19 subtypes based on wash-in rate (nonenhanced, slow, medium, and fast), wash-out enhancement (persistent, plateau, and decline), and wash-out stability (steady and unsteady), and the composition ratio of these 19 subtypes for each lesion was calculated as a new feature set (type-19). The three-type TIC classification, semiquantitative parameters, and type-19 features were used to build machine learning models for identifying lesion malignancy and classifying histologic grades, proliferation status, and molecular subtypes.
Results
The type-19 feature-based model significantly outperformed models based on the three-type TIC method and semiquantitative parameters both in distinguishing lesion malignancy (respectively; AUC = 0.875 vs. 0.831, p = 0.01 and 0.875vs. 0.804, p = 0.03), predicting tumor proliferation status (AUC = 0.890 vs. 0.548, p = 0.006 and 0.890 vs. 0.596, p = 0.020), but not in predicting histologic grades (p = 0.820 and 0.970).
Conclusion
In addition to conventional methods, the proposed computational approach provides a novel, model-free, data-driven approach to quantify and visualize hemodynamic heterogeneity.
Clinical relevance statement
Voxel-wise intra-lesion mapping of TIC profiles allows for visualization of hemodynamic heterogeneity and its composition ratio for differentiation of malignant and benign breast lesions.
Key Points
• Voxel-wise TIC profiles were mapped, and their composition ratio was compared between various breast lesions.
• The model based on the composition ratio of voxel-wise TIC profiles significantly outperformed the three-type TIC classification model and the semiquantitative parameters model in lesion malignancy differentiation and tumor proliferation status prediction in breast lesions.
• This novel, data-driven approach allows the intuitive visualization and quantification of the hemodynamic heterogeneity of breast lesions.






Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- DCE-MRI:
-
Dynamic contrast-enhanced magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- TIC:
-
Time-intensity curve
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics. CA Cancer J Clin 70:7–30
Loibl S, Poortmans P, Morrow M, Denkert C, Curigliano G (2021) Breast cancer. Lancet 397:1750–1769
Gerlinger M, Rowan AJ, Horswell S et al (2012) Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 366:883–892
Junttila MR, de Sauvage FJ (2013) Influence of tumour micro-environment heterogeneity on therapeutic response. Nature 501:346–354
Kim C, Suh J-Y, Heo C et al (2018) Spatiotemporal heterogeneity of tumor vasculature during tumor growth and antiangiogenic treatment: MRI assessment using permeability and blood volume parameters. Cancer Med 7:3921–3934
Mann RM, Cho N, Moy L (2019) Breast MRI: state of the art. Radiology 292:520–536
Rahmat K, Mumin NA, Hamid MTR, Hamid SA, Ng WL (2022) MRI breast: current imaging trends, clinical applications, and future research directions. Curr Med Imaging 18:1347–1361
Pinker K, Moy L, Sutton EJ et al (2018) Diffusion-weighted imaging with apparent diffusion coefficient mapping for breast cancer detection as a stand-alone parameter: comparison with dynamic contrast-enhanced and multiparametric magnetic resonance imaging. Invest Radiol 53:587–595
Khalifa F, Soliman A, El-Baz A et al (2014) Models and methods for analyzing DCE-MRI: a review. Med Phys 41:124301
Goto M, Ito H, Akazawa K et al (2007) Diagnosis of breast tumors by contrast-enhanced MR imaging: comparison between the diagnostic performance of dynamic enhancement patterns and morphologic features. J Magn Reson Imaging 25:104–112
Liu HL, Zong M, Wei H et al (2018) Differentiation between malignant and benign breast masses: combination of semi-quantitative analysis on DCE-MRI and histogram analysis of ADC maps. Clin Radiol 73:460–466
Winfield JM, Payne GS, Weller A, deSouza NM (2016) DCE-MRI, DW-MRI, and MRS in cancer: challenges and advantages of implementing qualitative and quantitative multi-parametric imaging in the clinic. Top Magn Reson Imaging 25:245–254
Lavini C, Verhoeff JJ, Majoie CB, Stalpers LJ, Richel DJ, Maas M (2011) Model-based, semiquantitative and time intensity curve shape analysis of dynamic contrast-enhanced MRI: a comparison in patients undergoing antiangiogenic treatment for recurrent glioma. J Magn Reson Imaging 34:1303–1312
Wu S, Berg WA, Zuley ML et al (2016) Breast MRI contrast enhancement kinetics of normal parenchyma correlate with presence of breast cancer. Breast Cancer Res 18:76
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
El Khouli RH, Macura KJ, Kamel IR, Jacobs MA, Bluemke DA (2011) 3-T dynamic contrast-enhanced MRI of the breast: pharmacokinetic parameters versus conventional kinetic curve analysis. AJR Am J Roentgenol 197:1498–1505
Cheng Z, Wu Z, Shi G et al (2018) Discrimination between benign and malignant breast lesions using volumetric quantitative dynamic contrast-enhanced MR imaging. Eur Radiol 28:982–991
Eida S, Ohki M, Sumi M, Yamada T, Nakamura T (2008) MR factor analysis: improved technology for the assessment of 2D dynamic structures of benign and malignant salivary gland tumors. J Magn Reson Imaging 27:1256–1262
Sasaki M, Sumi M, Eida S et al (2011) Multiparametric MR imaging of sinonasal diseases: time-signal intensity curve- and apparent diffusion coefficient-based differentiation between benign and malignant lesions. AJNR Am J Neuroradiol 32:2154–2159
Paldino MJ, Barboriak DP (2009) Fundamentals of quantitative dynamic contrast-enhanced MR imaging. Magn Reson Imaging Clin N Am 17:277–289
Xie T, Zhao Q, Fu C et al (2019) Differentiation of triple-negative breast cancer from other subtypes through whole-tumor histogram analysis on multiparametric MR imaging. Eur Radiol 29:2535–2544
Funding
This study was partially supported by Key Laboratory for Magnetic Resonance and Multimodality Imaging of Guangdong Province (2020B1212060051), Guangdong Innovation Platform of Translational Research for Cerebrovascular Diseases, Shenzhen Clinical Research Center for Cancer (No. [2021] 287) and Shenzhen High-level Hospital Construction Fund.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Na Zhang and Dehong Luo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Yuming Chen kindly provided statistical advice for this manuscript.
Informed consent
Due to the retrospective study design, written informed consent from the subjects was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
The manuscript or part of it has neither been published nor is currently under consideration for publication by any other journal.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Z., Yao, B., Wen, J. et al. Voxel-wise mapping of DCE-MRI time-intensity-curve profiles enables visualizing and quantifying hemodynamic heterogeneity in breast lesions. Eur Radiol 34, 182–192 (2024). https://doi.org/10.1007/s00330-023-10102-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10102-7