Abstract
Objectives
Blood flow into the side branch affects the calculation of coronary angiography-derived fractional flow reserve (FFR), called Angio-FFR. Neglecting or improperly compensating for the side branch flow may decrease the diagnostic accuracy of Angio-FFR. This study aims to evaluate the diagnostic accuracy of a novel Angio-FFR analysis that considers the side branch flow based on the bifurcation fractal law.
Methods
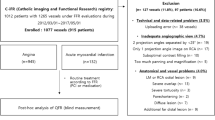
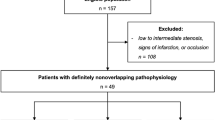
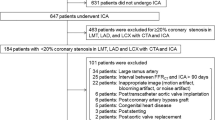
A one-dimensional reduced-order model based on the vessel segment was used to perform Angio-FFR analysis. The main epicardial coronary artery was divided into several segments according to the bifurcation nodes. Side branch flow was quantified using the bifurcation fractal law to correct the blood flow in each vessel segment. In order to verify the diagnostic performance of our Angio-FFR analysis, two other computational methods were taken as control groups: (i) FFR_s: FFR calculated by delineating the coronary artery tree to consider side branch flow, (ii) FFR_n: FFR calculated by just delineating the main epicardial coronary artery and neglecting the side branch flow.
Results
The analysis of 159 vessels from 119 patients showed that our Anio-FFR calculation method had comparable diagnostic accuracy to FFR_s and provided significantly higher diagnostic accuracy than that of FFR_n. In addition, using invasive FFR as a reference, the Pearson correlation coefficients of Angio-FFR and FFRs were 0.92 and 0.91, respectively, while that of FFR_n was only 0.85.
Conclusions
Our Angio-FFR analysis has demonstrated good diagnostic performance in assessing the hemodynamic significance of coronary stenosis by using the bifurcation fractal law to compensate for side branch flow.
Clinical relevance statement
Bifurcation fractal law can be used to compensate for side branch flow during the Angio-FFR calculation of the main epicardial vessel. Compensating for side branch flow can improve the ability of Angio-FFR to diagnose stenosis functional severity.
Key Points
• The bifurcation fractal law could accurately estimate the blood flow from the proximal main vessel into the main branch, thus compensating for the side branch flow.
• Angiography-derived FFR based on the bifurcation fractal law is feasible to evaluate the target diseased coronary artery without delineating the side branch.






Similar content being viewed by others
Abbreviations
- Angio-FFR:
-
Coronary angiography-derived fractional flow reserve based on bifurcation fractal law
- AUC:
-
Area under the receiver operating characteristic curve
- CABG:
-
Coronary artery bypass grafting
- DBP:
-
Diastolic blood pressure
- FFR:
-
Fractional flow reserve
- FFR_finet:
-
FFR calculated based on Finet’s law
- FFR_murray:
-
FFR calculated based on Murray’s law
- FFR_n:
-
FFR calculated by just delineating the main epicardial coronary artery
- FFR_s :
-
FFR calculated by delineating the coronary artery tree
- LAD :
-
Left anterior descending artery
- LCX:
-
Left circumflex artery
- MB:
-
Main branch
- MI :
-
Myocardial infarction
- NPV:
-
Negative predictive value
- PCI:
-
Percutaneous coronary intervention
- PM:
-
Proximal main vessel
- PPV:
-
Positive predictive value
- RCA:
-
Right coronary artery
- SB:
-
Side branch
- SBP:
-
Systolic blood pressure
References
Stergiopoulos K, Boden WE, Hartigan P et al (2014) Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia: a collaborative meta-analysis of contemporary randomized clinical trials. JAMA Intern Med 174(2):232–240
Shaw LJ, Weintraub WS, Maron DJ et al (2012) Baseline stress myocardial perfusion imaging results and outcomes in patients with stable ischemic heart disease randomized to optimal medical therapy with or without percutaneous coronary intervention. Am Heart J 164(2):243–250
Kogame N, Ono M, Kawashima H et al (2020) The impact of coronary physiology on contemporary clinical decision making. JACC Cardiovasc Interv 13(14):1617–1638
Neumann FJ, Sousa-Uva M, Ahlsson A et al (2019) 2018 esc/eacts guidelines on myocardial revascularization. Eur Heart J 40(2):87–165
Maria GL, Garcia-Garcia HM, Scarsini R et al (2020) Novel indices of coronary physiology: do we need alternatives to fractional flow reserve? Circ Cardiovasc Inte 13(4):e008487
Ramasamy A, Jin C, Tufaro V et al (2020) Computerised methodologies for non-invasive angiography-derived fractional flow reserve assessment: a critical review. J Interv Cardiol 6381637
Collet C, Onuma Y, Sonck J et al (2018) Diagnostic performance of angiography-derived fractional flow reserve: a systematic review and Bayesian meta-analysis. Eur Heart J 39(35):3314–3321
Takahashi T, Shin D, Kuno T et al (2022) Diagnostic performance of coronary angiography- and intravascular imaging-based fractional flow reserve to detect functionally significant coronary stenoses: a systemic review and meta-analysis. J Am Coll Cardiol 79(9s):838–838
Xu B, Tu S, Song L et al (2021) Angiographic quantitative flow ratio-guided coronary intervention (favor iii china): a multicentre, randomised, sham-controlled trial. Lancet 398(10317):2149–2159
Li Y, Guti´errez-Chico JL, Holm NR et al (2015) Impact of side branch modeling on computation of endothelial shear stress in coronary artery disease: coronary tree reconstruction by fusion of 3d angiography and oct. J Am Coll Cardiol 66(2):125–135
Choi KH, Dai N, Li Y et al (2021) Functional coronary angiography–derived index of microcirculatory resistance in patients with st-segment elevation myocardial infarction. JACC Cardiovasc Interv 14(15):1670–1684
Papafaklis MI, Muramatsu T, Ishibashi Y et al (2014) Fast virtual functional assessment of intermediate coronary lesions using routine angiographic data and blood flow simulation in humans: comparison with pressure wire-fractional flow reserve. EuroIntervention 10(5):574–583
Kornowski R, Lavi I, Pellicano M et al (2016) Fractional flow reserve derived from routine coronary angiograms. J Am Coll Cardiol 68(20):2235–2237
Tu S, Barbato E, Ko¨szegi Z et al (2014) Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count: a fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC Cardiovasc Interv 7(7):768–777
Tu S, Westra J, Yang J et al (2016) (2016) Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the international multicenter favor pilot study. JACC Cardiovasc Interv 9(19):2024–2035
Gibson CM, Cannon CP, Daley WL et al (1996) Timi frame count: a quantitative method of assessing coronary artery flow. Circulation 93(5):879–888
Zhang H, Zhang D, Gao Z, Zhang H (2021) Joint segmentation and quantification of main coronary vessels using dual-branch multi-scale attention network. Int Conf Med Image Comput Comput-Assist Interv 369–378
Greenspan H, Laifenfeld M, Einav S, Barnea O (2001) Evaluation of center-line extraction algorithms in quantitative coronary angiography. IEEE Trans Med Imaging 20(9):928–941
Zhang Y, Zhang S, Westra J et al (2019) Automatic coronary blood flow computation: validation in quantitative flow ratio from coronary angiography. Int J Cardiovas Imag 35(4):587–595
Huo Y, Kassab GS (2009) A scaling law of vascular volume. Biophys J 96(2):347–353
Huo Y, Finet G, Lefèvre T, Louvard Y, Moussa I, Kassab GS (2012) Optimal diameter of diseased bifurcation segment: a practical rule for percutaneous coronary intervention. EuroIntervention 7(11):1310–1316
Liu X, Xu C, Rao S et al (2022) Physiologically personalized coronary blood flow model to improve the estimation of noninvasive fractional flow reserve. Med Phys 49(1):583–597
Gosling RC, Sturdy J, Morris PD et al (2020) Effect of side branch flow upon physiological indices in coronary artery disease. J Biomech 103:109698
Tu S, Ding D, Chang Y, Li C, Wijns W, Xu B (2021) Diagnostic accuracy of quantitative flow ratio for assessment of coronary stenosis significance from a single angiographic view: a novel method based on bifurcation fractal law. Catheter Cardio Inte 97:1040–1047
Yu W, Tanigaki T, Ding D et al (2021) Accuracy of intravascular ultrasound-based fractional flow reserve in identifying hemodynamic significance of coronary stenosis. Circ Cardiovasc Inte 14(2):e009840
Murray CD (1926) The physiological principle of minimum work: I. the vascular system and the cost of blood volume. Proc Natl Acad Sci U S A 12(3):207–214
Finet G, Gilard N, Perrenot B et al (2008) Fractal geometry of arterial coronary bifurcations: a quantitative coronary angiography and intravascular ultrasound analysis. EuroIntervention 3(4):490–498
D´erimay F, Kassab GS, Finet G (2021) Structure-function relation in the coronary artery tree: theory and applications in interventional cardiology. Biomechanics of Coronary Atherosclerotic Plaque. Academic Press 545– 554
Blanco PJ, Bulant CA, M ̈uller LO et al (2018) Comparison of 1d and 3d models for the estimation of fractional flow reserve. Sci rep 8(1):1–12
Young DF, Tsai FY (1973) Flow characteristics in models of arterial stenoses—ii. unsteady flow. J Biomech 6(5):547–559
Hajian-Tilaki K (2014) Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform 48:193–204
Koo BK, Kang HJ, Youn TJ et al (2015) Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol 46:633–637
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Shahzad R, Kirişli H, Metz C et al (2013) Automatic segmentation, detection and quantification of coronary artery stenoses on CTA. Int J Cardiovas Imag 29(8):1847–1859
Pijls NH, De Bruyne B, Peels K et al (1996) Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 334(26):1703–1708
Funding
This study has received funding from the Clinical Research Program of Nanfang Hospital, Southern Medical University (2021CR007), and the National Natural Science Foundation of China (81974266, 82270439, 62101610).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xiujian Liu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
No subject has been previously reported.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, H., Zhang, Q., Gao, Y. et al. Diagnostic performance of angiography-derived fractional flow reserve analysis based on bifurcation fractal law for assessing hemodynamic significance of coronary stenosis. Eur Radiol 33, 6771–6780 (2023). https://doi.org/10.1007/s00330-023-09682-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09682-1