Abstract
Objectives
To determine whether radiomics features derived from diffusion-weighted imaging (DWI) and arterial spin labeling (ASL) can improve the differentiation between radiation-induced brain injury (RIBI) and tumor recurrence (TR) in glioma patients.
Methods
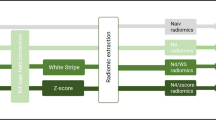
A total of 4199 radiomics features were extracted from conventional MRI, apparent diffusion coefficient (ADC), and cerebral blood flow (CBF) maps, obtained from 96 pathologically confirmed WHO grade 2~4 gliomas with enhancement after standard treatment. The intraclass correlation coefficient (ICC) was used to test segmentation stability between two doctors. Radiomics features were selected using the Mann–Whitney U test, LASSO regression, and RFE algorithms. Four machine learning classifiers were adopted to establish radiomics models. The diagnostic performance of multiparameter, conventional, and single-parameter MRI radiomics models was compared using the area under the curve (AUC). The models were evaluated in the subsequent independent validation set (n = 30).
Results
Eight important radiomics features (3 from conventional MRI, 1 from ADC, and 4 from CBF) were selected. Support vector machine (SVM) was chosen as the optimal classifier. The diagnostic performance of the multiparameter MRI radiomics model (AUC 0.96) was higher than that of the conventional MRI (AUC 0.88), ADC (AUC 0.91), and CBF (AUC 0.95) radiomics models. For subgroup analysis, the multiparameter MRI radiomics model showed similar performance, with AUCs of 0.98 in WHO grade 2~3 and 0.96 in WHO grade 4.
Conclusion
The incorporation of noninvasive DWI and ASL into the MRI radiomics model improved the diagnostic performance in differentiating RIBI from TR; ASL, especially, played a significant role.
Key Points
• The multiparameter MRI radiomics model was superior to the conventional MRI radiomics model in differentiating glioma recurrence from radiation-induced brain injury.
• Diffusion and perfusion MRI could improve the ability of the radiomics model in predicting the progression in patients with glioma.
• Arterial spin labeling played an important role in predicting glioma progression using radiomics models.





Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- ASL:
-
Arterial spin labeling
- AUC:
-
Area under the receiver operating characteristics curve
- BBB:
-
Blood–brain barrier
- CBF:
-
Cerebral blood flow
- CE:
-
Contrast-enhanced
- DSC:
-
Dynamic susceptibility contrast-enhanced
- DWI:
-
Diffusion-weighted imaging
- GLCM:
-
Gray-level co-occurrence matrix
- GLRLM:
-
Gray-level run-length matrix
- GLSZM:
-
Gray-level size zone matrix
- ICC:
-
Intraclass correlation coefficient
- IDH:
-
Isocitrate dehydrogenase
- KNN:
-
K-nearest neighbor
- LASSO:
-
Least absolute shrinkage and selection operator
- LR:
-
Logistic regression
- MRS:
-
Magnetic resonance spectroscopy
- NB:
-
Naive Bayes
- PsP:
-
Pseudoprogression
- RFE:
-
Recursive feature elimination
- RIBI:
-
Radiation-induced brain injury
- RN:
-
Radiation necrosis
- ROC:
-
Receiver operating characteristic curves
- ROI :
-
Regions of interest
- SVM:
-
Support vector machine
- TMZ:
-
Temozolomide
- TR:
-
Tumor recurrence
References
Ostrom QT, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (2021) CBTRUS Statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2014-2018. Neuro Oncol 23:i1–i105
Weller M, van den Bent M, Preusser M et al (2021) EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol 18:170–186
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Parvez K, Parvez A, Zadeh G (2014) The diagnosis and treatment of pseudoprogression, radiation necrosis and brain tumor recurrence. Int J Mol Sci 15:11832–11846
Radbruch A, Fladt J, Kickingereder P et al (2015) Pseudoprogression in patients with glioblastoma: clinical relevance despite low incidence. Neuro Oncol 17:151–159
Wilson CB, Crafts D, Levin V (1977) Brain tumors: criteria of response and definition of recurrence. Natl Cancer Inst Monogr 46:197–203
Furuse M, Nonoguchi N, Kawabata S, Miyatake S, Kuroiwa T (2015) Delayed brain radiation necrosis: pathological review and new molecular targets for treatment. Med Mol Morphol 48:183–190
Abbasi AW, Westerlaan HE, Holtman GA, Aden KM, van Laar PJ, van der Hoorn A (2018) Incidence of tumour progression and pseudoprogression in high-grade gliomas: a systematic review and meta-analysis. Clin Neuroradiol 28:401–411
van West SE, de Bruin HG, van de Langerijt B, Swaak-Kragten AT, van den Bent MJ, Taal W (2017) Incidence of pseudoprogression in low-grade gliomas treated with radiotherapy. Neuro Oncol 19:719–725
Zhou H, Vallieres M, Bai HX et al (2017) MRI features predict survival and molecular markers in diffuse lower-grade gliomas. Neuro Oncol 19:862–870
Prager AJ, Martinez N, Beal K, Omuro A, Zhang Z, Young RJ (2015) Diffusion and perfusion MRI to differentiate treatment-related changes including pseudoprogression from recurrent tumors in high-grade gliomas with histopathologic evidence. AJNR Am J Neuroradiol 36:877–885
Kim JY, Park JE, Jo Y et al (2019) Incorporating diffusion- and perfusion-weighted MRI into a radiomics model improves diagnostic performance for pseudoprogression in glioblastoma patients. Neuro Oncol 21:404–414
Grade M, Hernandez TJ, Pizzini FB, Achten E, Golay X, Smits M (2015) A neuroradiologist’s guide to arterial spin labeling MRI in clinical practice. Neuroradiology 57:1181–1202
Thust SC, van den Bent MJ, Smits M (2018) Pseudoprogression of brain tumors. J Magn Reson Imaging 48:571–589
Jovanovic M, Radenkovic S, Stosic-Opincal T et al (2017) Differentiation between progression and pseudoprogresion by arterial spin labeling MRI in patients with glioblastoma multiforme. J BUON 22:1061–1067
Manning P, Daghighi S, Rajaratnam MK et al (2020) Differentiation of progressive disease from pseudoprogression using 3D PCASL and DSC perfusion MRI in patients with glioblastoma. J Neurooncol 147:681–690
Razek A, El-Serougy L, Abdelsalam M, Gaballa G, Talaat M (2018) Differentiation of residual/recurrent gliomas from postradiation necrosis with arterial spin labeling and diffusion tensor magnetic resonance imaging-derived metrics. Neuroradiology 60:169–177
Ozsunar Y, Mullins ME, Kwong K et al (2010) Glioma recurrence versus radiation necrosis? A pilot comparison of arterial spin-labeled, dynamic susceptibility contrast enhanced MRI, and FDG-PET imaging. Acad Radiol 17:282–290
Lambin P, Leijenaar R, Deist TM et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14:749–762
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972
Chukwueke UN, Wen PY (2019) Use of the Response Assessment in Neuro-Oncology (RANO) criteria in clinical trials and clinical practice. CNS Oncol 8:S28
Hepp T, Schmid M, Gefeller O, Waldmann E, Mayr A (2016) Approaches to regularized regression - a comparison between gradient boosting and the Lasso. Methods Inf Med 55:422–430
Cha J, Kim ST, Kim HJ et al (2014) Differentiation of tumor progression from pseudoprogression in patients with posttreatment glioblastoma using multiparametric histogram analysis. AJNR Am J Neuroradiol 35:1309–1317
Kong DS, Kim ST, Kim EH et al (2011) Diagnostic dilemma of pseudoprogression in the treatment of newly diagnosed glioblastomas: the role of assessing relative cerebral blood flow volume and oxygen-6-methylguanine-DNA methyltransferase promoter methylation status. AJNR Am J Neuroradiol 32:382–387
Song YS, Choi SH, Park CK et al (2013) True progression versus pseudoprogression in the treatment of glioblastomas: a comparison study of normalized cerebral blood volume and apparent diffusion coefficient by histogram analysis. Korean J Radiol 14:662–672
Lee WJ, Choi SH, Park CK et al (2012) Diffusion-weighted MR imaging for the differentiation of true progression from pseudoprogression following concomitant radiotherapy with temozolomide in patients with newly diagnosed high-grade gliomas. Acad Radiol 19:1353–1361
Thomsen H, Steffensen E, Larsson EM (2012) Perfusion MRI (dynamic susceptibility contrast imaging) with different measurement approaches for the evaluation of blood flow and blood volume in human gliomas. Acta Radiol 53:95–101
Patel M, Zhan J, Natarajan K et al (2021) Machine learning-based radiomic evaluation of treatment response prediction in glioblastoma. Clin Radiol 76:617–628
Reimer C, Deike K, Graf M et al (2017) Differentiation of pseudoprogression and real progression in glioblastoma using ADC parametric response maps. PLoS One 12:e174620
Choi YJ, Kim HS, Jahng GH, Kim SJ, Suh DC (2013) Pseudoprogression in patients with glioblastoma: added value of arterial spin labeling to dynamic susceptibility contrast perfusion MR imaging. Acta Radiologica 54:448–454
Wang YL, Chen S, Xiao HF et al (2018) Differentiation between radiation-induced brain injury and glioma recurrence using 3D pCASL and dynamic susceptibility contrast-enhanced perfusion-weighted imaging. Radiother Oncol 129:68–74
Gutsche R, Scheins J, Kocher M et al (2021) Evaluation of FET PET radiomics feature repeatability in glioma patients. Cancers (Basel) 13
Chang PD, Malone HR, Bowden SG et al (2017) A multiparametric model for mapping cellularity in glioblastoma using radiographically localized biopsies. AJNR Am J Neuroradiol 38:890–898
Materka A, Strzelecki M (1998) Texture analysis methods - a review. Institute of Electronics Technical University of Lodz
Su C, Jiang J, Zhang S et al (2019) Radiomics based on multicontrast MRI can precisely differentiate among glioma subtypes and predict tumour-proliferative behaviour. Eur Radiol 29:1986–1996
Ion-Margineanu A, Van Cauter S, Sima DM et al (2016) Classifying glioblastoma multiforme follow-up progressive vs. responsive forms using multi-parametric MRI features. Front Neurosci 10:615
Hashido T, Saito S, Ishida T (2020) A radiomics-based comparative study on arterial spin labeling and dynamic susceptibility contrast perfusion-weighted imaging in gliomas. Sci Rep 10:6121
Tan Y, Zhang ST, Wei JW et al (2019) A radiomics nomogram may improve the prediction of IDH genotype for astrocytoma before surgery. Eur Radiol 29:3325–3337
Akbari H, Bakas S, Pisapia JM et al (2018) In vivo evaluation of EGFRvIII mutation in primary glioblastoma patients via complex multiparametric MRI signature. Neuro Oncol 20:1068–1079
Funding
This work was supported by the National Key R&D Program of China (2019YFB1311600) and the National Natural Science Foundation of China (62072358).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Lin Ma, MD.
Conflict of interests
The authors of this manuscript declare no relationship with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise (Guangming Zhu, 8 years of experience).
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Cross-sectional study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jun Zhang and Yue Wu are co-first authors.
Supplementary Information
ESM 1
(DOC 93.5 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, J., Wu, Y., Wang, Y. et al. Diffusion-weighted imaging and arterial spin labeling radiomics features may improve differentiation between radiation-induced brain injury and glioma recurrence. Eur Radiol 33, 3332–3342 (2023). https://doi.org/10.1007/s00330-022-09365-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09365-3